Practice Management | August 2020 Hearing Review
Real-life examples and ideas for enhancing teleaudiology functionality within hearing care
By Bopanna Ballachanda, PhD
A large selection of teleaudiology solutions now exist that provides greater practice efficiencies and much higher levels of outreach and accessibility for your patients—and for other consumers who should be your patients. Here is just a brief sampling of some of the options for enhancing your teleaudiology capabilities.
Teleaudiology is the utilization of telehealth to provide audiological services. It utilizes electronic information and telecommunications technologies to support remote hearing care, professional and public education, public health matters, and health administration. In general, audiologists and hearing aid specialists have been behind the curve in adopting teleaudiology advances,1-3 with the major impediments being limitations in infrastructure, reimbursement, and licensure,2 as well as a hesitancy to change long-standing practice procedures. There may be several reasons for this hesitancy, among them a perception that telecare represents a disruptive business threat, and that it may one day become the “standard of practice” in audiology.
During the Covid-19 pandemic of 2020, this has proven to be false. Contrary to the paranoia, teleaudiology provides supplemental care in the absence of face-to-face encounters, and can be readily employed in the way a practitioner thinks is best for his/her patients and practice.
10 Reasons to Pursue Teleaudiology
The current situation of social distancing has given impetus to the adoption of teleaudiology. But, beyond our current situation with Covid-19, there are at least 10 good reasons for hearing care professionals (HCPs) to embrace and incorporate teleaudiology:
- Covid-19 is not the first and certainly won’t be the last infectious disease to pose a threat to seniors (and others), and telecare provides a vast range of services that offer limited patient-HCP contact during these times;
- The shortage of audiologists at present and in the future4;
- The burgeoning aging population, creating higher demand for hearing services from a limited number of HCPs;
- Healthcare pressure to contain the cost of doing business5;
- Introduction of over-the-counter (OTC) hearing aids, as well as hybrid delivery models (eg, Blamey-Saunders, Lively), and the competitive challenges/opportunities they might bring;
- Changes in payment/reimbursement for hearing care by third-party payers;
- Healthcare worker burnout and lifestyle aspirations of younger professionals;
- The need for customized care to patients, including self-driven care/management;
- Changes in healthcare behavior by the general public to have personalized and on-demand support, and
- Easy and convenient access by mobile phones to hearing care services.
Although I have written and co-written several articles about teleaudiology,7-10 there exist few explicit instructions about how to incorporate teleaudiology into an existing practice or to set up a new teleaudiology practice using specific examples. Therefore, the goals of this article are to: 1) Briefly identify and explain two teleaudiology delivery models; 2) Provide some real examples for installing a new teleaudiology clinic and/or convert a current clinic to provide teleaudiology services, and 3) Explain the workings of telecare during the pandemic and beyond.
Author’s Note: It should be understood that the downside of citing specific technologies and products is the exclusion other equally good—or perhaps even better—options. Thus, the reader should be aware that, in almost all the examples cited here, there are many other teleaudiology options available; this article uses a limited number of products that I’m most familiar. Additionally, HCPs should note that states, licensing bodies, and third-party payers may have their own sets of rules pertaining to teleaudiology, and there are also the HIPAA-compliance rules that need to be observed, all subjects beyond the scope of this article.
3 Teleaudiology Delivery Modalities
There are three primary modes of telehealth delivery:
Synchronous: This involves live two-way interaction between patient (and family member or caregiver) and provider using audiovisual telecommunications technology. Typical applications/procedures can include audiological evaluation, hearing aid fittings, real-ear measures, hearing aid counseling, tinnitus management, and aural rehabilitation.
Remote patient monitoring (RPM): RPM involves personal health and medical data collection from an individual in one location via electronic communication technologies, then transmitted to a provider (sometimes via a data processing service) in a different place for use in care and related support. This type of service allows a provider to continue to track healthcare data for a patient once released to home or a care facility, reducing readmission rates. One obvious example of RPM is its use by HCPs to address hearing aid issues such as programming and other related services.
Asynchronous: Also known as “store-and-forward,” the asynchronous mode is most often used in newborn hearing screening, video otoscopy, and automated hearing testing. In these cases, the audiologist receives the audiometric data following collection, then reviews it for interpretation (eg, audiometry, immittance, OAE, etc).
TWO BASIC Teleaudiology Delivery Models
Teleaudiology and remote hearing care services don’t necessarily have to entail a complex program and don’t always have to be between two clinics. A comprehensive teleaudiology clinic can provide: 1) Video otoscopy; 2) Hearing screening; 3) Diagnostic testing with pure-tone and speech audiometry, tympanometry, reflexes, auditory brainstem testing, OAE testing, etc. 4) Hearing aid recommendation, orientation, fitting, programming, verification, and validation of the hearing aid fitting; 5) Counseling and aural rehab programs; 6) Trouble-shooting hearing aids, and 7) Tinnitus evaluation and management; 7) Cochlear implant programming and management; 8) Balance testing and management (again not wholly integrated into teleaudiology). Model 1 provides examples of how it’s possible to provide the comprehensive audiology services listed above remotely via specialized audiologic equipment; Model 2 provides examples of technologies that promise wider consumer/global access to audiologic services—albeit not comprehensive services—through a new class of emerging mobile technology.
Model 1: Connecting Two Clinics/Sites
Probably the most common scenario for teleaudiology implementation is establishing a connection between two clinics or locations—usually from the main clinic to a remote or satellite location, such as subsidiary office or even the home of a patient (Figure 1 and Table 1). In particular, this is quite common when a provider is unable to travel to a satellite location, or a clinician at a satellite location wishes to “take over” a computer to assist with patients in the main clinic. A second option is connecting between the clinic and another location, such as a home, senior care facility, etc (eg, for social distancing and/or when the clinician cannot make it to the loacation). Again, using this model, all types of remote testing can be done with the help of an assistant or a facilitator for clinical service.
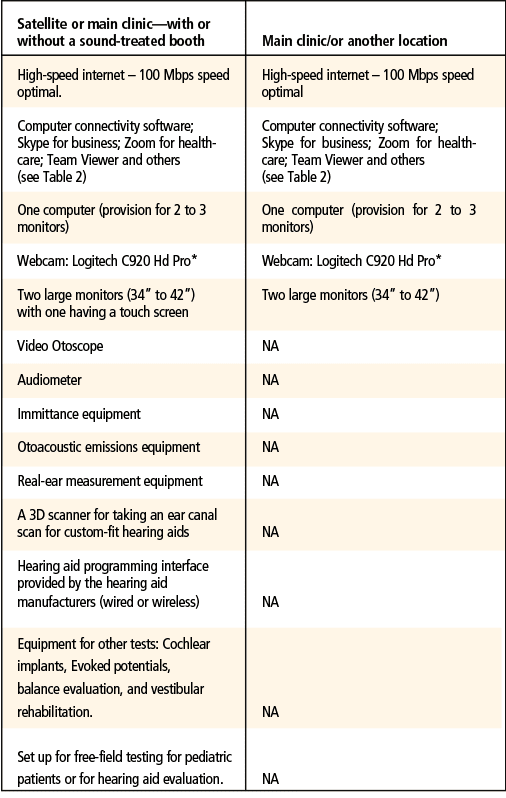
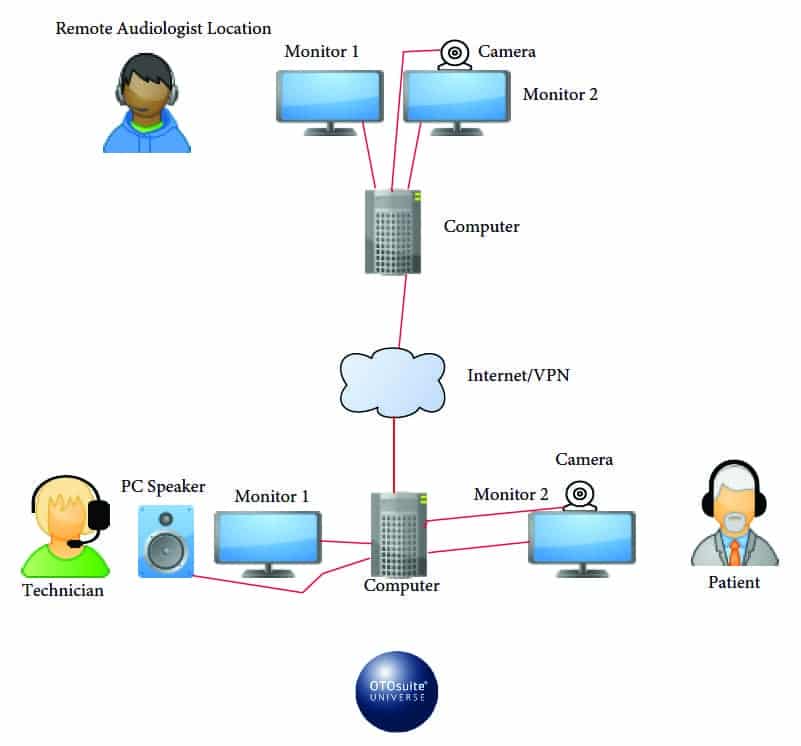

Therefore, Model 1 is essentially an attempt to duplicate the traditional clinic setting, with limited physical encounters by the hearing care professional and with limited number of staff in that clinic. The satellite clinic can be similar to the main clinic in terms of the type and pieces of equipment, and the testing can be performed with or wishout a sound-treated booth (Tables 1 and 2).
Examples for setting up Model 1. For video conferencing and connectivity with the patient, there are currently several options including: Skype for Business/Microsoft Teams, Zoom for Healthcare, Updox, VSee, Doxy.me, Google G Suite Hangouts Meet, Cisco WebEx Meetings, Amazon Chime, and GoToMeeting.com. As mentioned previously, HIPAA-compliance and your own network data privacy/security rules may limit options.
Table 2 provides a quick overview of four popular teleaudiology companies’ systems. Again, these are presented as examples only; there are many more products from these and other companies, all of which offer different advantages and pros/cons. Additionally, where the company may not offer a dedicated solution for a test/procedure (eg, 3D ear canal scanning), other companies’ products can be employed (eg, Lantos).
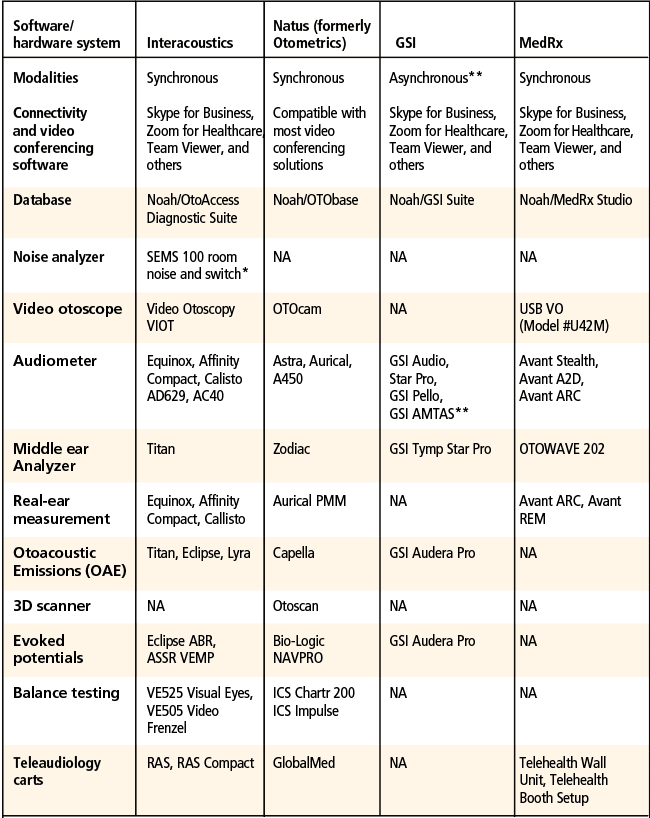
“NA” simply denotes that the author is unaware of a dedicated solution from that company for this particular function; in most cases, a wide variety of alternate products/technologies are available for use.
*A unique advantage that Interacoustics provides is the SEMS100 switch box which allows private communication with the assistant or facilitator when the patient does not need to hear the clinician (eg, for headset changes, video otoscopy instructions and REM tube placement guidance for the technician, etc).
** GSI’s asynchronous method of teleaudiology, GSI AMTAS (Automated Method for Testing Auditory Sensitivity), is a software system that allows a patient to walk him/herself through an automated hearing evaluation. The AMTAS Pro must be used with a GSI AudioStar Pro or Pello and a PC, and AMTAS Flex is a tablet-based program that is air-conduction only and is used with a windows tablet and calibrated headphones. This asynchronous method of teleaudiology is an example of how these systems can allow greater access to audiology services; the HCP does not need to block time in the schedule to perform the test and can instead work on tymps, hearing aid fittings, charting, or prepping for the next patient during this time—which can be advantageous for satellite clinics or on-site at the main clinic. The patient works through the AMTAS evaluation, and then the audiologist interprets the results and meets with the patient via video teleconference to discuss results, additional tests, etc.
Description of a teleaudiology visit using Model 1: The teleaudiology visit can take place using a sound-treated booth or without one using a noise monitor to determine the accuracy of the testing.
Procedures at the satellite clinic or remote location (that need to be connected):Before the patient arrives, the assistant/technician/facilitator prepares the remote location for the audiology testing or follow up care. Usually, the steps that the assistant follows are:
1) Before the patient arrives, the assistant/technician/facilitator prepares the remote location for the audiology testing or follow up care. Usually, the steps that the assistant follows are:
a) Turn on the computer;
b)Determine the noise level (in locations where a sound booth does not exist);
c)Sanitize the equipment (performed before and after each patient visit);
d)Open the patient database using Noah or a database provided by the manufacturer(s);
e)Input the essential patient information into the database; in cases of previous patients, open the patient file.
f)Obtain updated case history from the patient at the clinic or previously obtained through the website.
g) Forward the information to the HCP.
2) At this point, the patient is ready to see the provider. The assistant then activates the HIPAA-compliant conferencing software (eg, Skype for Business, Zoom for Healthcare, etc, as detailed above).
3) Once the provider is online, the audiology assistant hands off the computer control to the provider.
4) The patient is accompanied to the teleaudiology room by the assistant, is seated in front of the monitor, and introduced to the provider.
5) The provider explains test procedures to the patient, and testing begins. (The assistant can use a headset for private/confidential provider instructions not needed to be heard by the patient.)
6) The provider instructs the assistant to assist with various tests. The testing sequences are: video otoscopy, followed by pure-tone audiometry, including bone testing, speech testing, and additional tests, as needed.
7) Counseling using video conferencing tools.
8) Follow-up care based on hearing evaluation—including hearing care recommendations.
9) Ear impression for custom aids or earmolds using 3D scanners.
10) Conclusion of the testing and recommendation(s) for treatment and/or referral to other specialists, as well as follow-up care plans.
Before leaving this section, I should point out that, in response to the Covid-19 pandemic, there has been huge growth in telecare solutions for remote hearing aid programming and adjustment. While this could be the subject of a much larger article or series, several informative reviews of these systems have been published recently.11-15
Model 2: Connecting with Consumers via Mobile Devices for Special Care Situations and Initial Screenings/Assessments
The world isn’t perfect, and all of us have been in situations where patient access to the specialized equipment within our practices is either impossible or at least impractical (especially in today’s Covid-19 crisis). While we can engage in discussions about best practices and standards of professional care, the provision of some professional hearing assistance and guidance is doubtlessly better than none, and there is a growing list of tools that render reliable audiologic data and/or that rely on solid foundational auditory research in their product development—and hopefully lead to more HCP-guided care.
Model 2, unlike Model 1, relies entirely on using a mobile phone, tablet, or computer without the specialized equipment described in Model 1. As a result, limitations exist in identifying and diagnosing hearing and balance problems. The obvious key advantage of Model 2 is accessibility for the general public. The number of smartphone users in the United States is now around 275.7 million, and projected to rise to 290.6 million by 2024.16 Given this exceptional number, it is appealing to the healthcare industry and professionals, including HCPs, to tap quality resources and reach many individuals who, for whatever reason, are not seeking hearing help. (Author’s note: One could reasonably argue that highly compact and mobile systems, like those from MedRx or Shoebox, should be listed in this section; however, I’m limiting devices in Model 2 to those on-the-go devices not typically found/offered in an audiology clinic.)
Otoscopy. Otoscopy is an essential part of best practices in audiology. Otoscopic examination of the ear canal and tympanic membrane helps the HCP to identify blockages, as well as pathological conditions of the ear canal and middle ear. Current mobile options include the Hear Scope, an affordable smartphone attachment that functions as an otoscope, allowing the capture of high-quality images and videos of the eardrum and the ear canal to store and share. Other otoscopes used with a smartphone, tablet, or computer are the Firefly DE550 and DE570 wireless/wired digital video otoscopes (Figure 2) and the Dino-Lite Hi-Resolution Digital Video Otoscope (Model AM4113EUT). These products are highly compact and mobile.

The FDA-recommended red flag questions should be part of all case histories, and are especially important in this model for identifying conditions that require medical attention and medical clearance. Whenever in doubt, ask the patient to see her/his primary care physician or an ENT.
Audiometry via smartphone and headphones. The HearX hearTest clinical smartphone audiometer (Figure 3) was developed by Dewet Swanepoel17 and colleagues at the University of Pretoria in South Africa, and the app can be downloaded to an Android phone. This audiometer uses pre-calibrated headphones (Sennheiser HDA 300), and the noise attenuatation level provided by this headphone is said to be equivalent to a single-walled sound-treated room.18 The most recent version of this test includes extended high-frequency testing capabilities out to 16 kHz for some test conditions. The HearX smartphone audiometer has been shown to provide valid test results.20 Therefore, it can be administered in-home and in other places with reliability, without worrying too much about the effect of ambient noise levels (it also features real-time monitoring of noise). The company also markets an extension of the test for occupational hearing conservation programs.

The newcomer to the line of tests that use calibrated headphones for hearing testing is called Clementine (Figure 4). The company uses kiosks, the internet, home delivery of test boxes, and mobile testing to help HCPs and industry test people in need of remote hearing care assistance. A pair of calibrated headphones in a box is shipped to the person taking the hearing test. The headphone box has the option to connect to the internet then relay the test findings on a real-time basis (eg, with or without a video consult), or it can be used offline so that it doesn’t require 4G or a WiFi connection (ie, people can take the hearing test by themselves and ship the case back to the HCP). Pure-tone air, bone conduction, and speech tests are reportedly performed with excellent reliability via the Clementine app and the headphones.

Home hearing tests. There are at least three well-known at-home hearing tests for purchase by consumers. One of the most venerable and well-researched is the Etymotic Home Hearing Test (HHT) kit designed for home use, community-based testing, and telehealth practice (Figure 5). The test kit contains a calibrated sound card and noise-isolating insert earphones, and can be administered using a personal computer or tablet. The HHT is an automated hearing screening test that measures ear-specific air conduction thresholds at octave frequencies from 0.5 to 8 kHz. It uses the Automated Testing Methods for Auditory Sensitivity (ATMAS), a validated procedure for measuring pure-tone thresholds described by audiologist-researcher Robert Margolis and colleagues.21-24 ATMAS employs a forced-choice adaptive psychophysical procedure with feedback and includes Qualind, which estimates test accuracy by tracking response time, false-alarm rates, test-retest differences, and quality check failures.24 Several research studies examined the validity of this test23,25 and found that HHT thresholds for pure tones were quite close to standard audiometric testing. The HHT is available from Etymotic Research for $149.

The FDA-approved iHEARTest kit26 was developed by Lyric-inventor /engineer Adnan Shennib and colleagues, and includes factory-calibrated earphones and a handheld USB device for connection to a personal computer (Figure 6). The iHEARTest software (downloaded from the website) provides step-by-step instructions for running the test using Microsoft Windows or Mac OS X. After the test, results are stored on a remote HIPAA-compliant server for review at any time by the consumer using secure online access, with results for each ear ranging from 5 (good hearing) to 1 (profound loss). The test system also conducts periodic checks of earphone calibration to ensure continued test signal accuracy. More recently, the company has been offering the iHEARTest free of charge if the consumer returns the device within 30 days and pays a small shipping fee (iHear Medical also markets DTC hearing aids).

The National Hearing Test is probably the most widely-used screening test administered over the telephone (Figure 7).27 This test, developed with funding from the National Institutes of Health (NIH), involves listening to 3-digit sequences presented in white noise (with varying signal-to-noise ratios depending on the responses), and the participant enters the digits using the telephone keypad. The test is quick and convenient, and it costs only $8 (but is free for AARP members).28 Immediately after the test, the results are made available for each ear, which helps the participant make an informed decision about seeing an HCP to have a complete hearing evaluation. The growing popularity of this form of screening test is due in part to its demonstrated validity and reliability. Testing by telephone is also a convenient, discreet, inexpensive way to determine whether a person’s functional hearing is within the normal range.
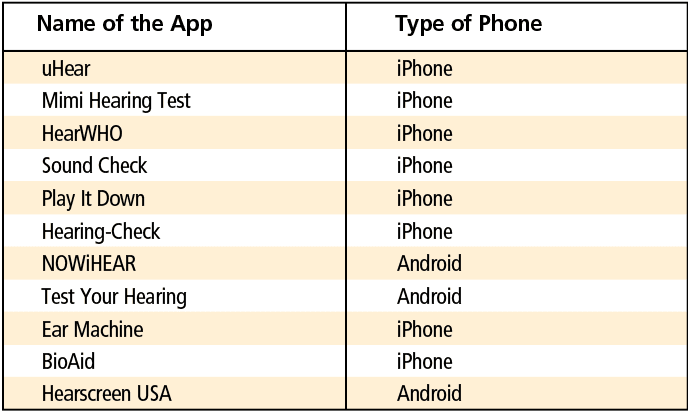
Hearing screening apps. Numerous hearing screening apps exist on the internet, including on hearing aid manufacturer websites, independent practitioner sites, and other online hearing sites (eg, Lively, Eargo, and Audicus). Several online tests are available as part of public education, identification of potential patients for a device manufacturer, and/or as part of a hearing management program (Table 3). Some of these sites are managed by audiologists and provide high quality professional care. Essentially, the tests fall into three categories: 1) Tonal tests using warble or frequency-modulated tones; 2) Digit-in-noise tests; 3) Picture-pointing test for words heard in various background noise levels; and 4) Combined tonal and digit-in-noise tests. In all these tests, the primary concern is the calibration of the earpiece in delivering the sound, as well as the surrounding noise levels. An ideal situation would be to retest the individual at different times—and of course the optimal situation would be to obtain an audiogram from a qualified HCP.
More complex apps attempt to mimic full hearing tests by playing several frequencies at various volume levels under headphones, with some even graphing the results. One has to exercise caution in interpreting the results from these apps. However, if the results from these screening apps show difficulties in hearing, it indicates it is time for the consumer to seek hearing help.
References
1. Northern JL. Extending hearing healthcare: Tele-audiology. Hearing Review. 2012;19(10):12-16.
2. Ravi R, Gunjawate DR, Yerraguntla K, Driscoll C. Knowledge and perceptions of teleaudiology among audiologists: A systematic review. J Audiol Otol. 2018;22(3):120-127.
3. The American Speech-Language-Hearing Association (ASHA). Telepractice. https://www.asha.org/PRPSpecificTopic.aspx?folderid=8589934956§ion=Overview.
4. Freeman BA. The coming crisis in audiology. Audiology Today. 2009;21(6):46-52.
5. Bakke J. What hearing care professionals need to know about today’s healthcare economics. Hearing Review. 2016;23(10):16.
6. Kauffman L. Special report: Hearing care and ‘value-based reimbursement’ in medicine. Hearing Review. 2018;25(3)[Supp1]:S1-8.
7. Ballachanda B. Critical steps in establishing a teleaudiology practice. Part 1: A 10-point checklist when planning for a teleaudiology program. Hearing Review. 2017;24(1)14.
8. Ballachanda B. Critical steps in establishing a teleaudiology practice. Part 2: Preparing for your level of implementation and involvement in telepractice. Hearing Review. 2017;24(4):20-21.
9. Ballachanda B. Telepractice in audiology. Audiology Online. https://www.audiologyonline.com/articles/telepractice-in-audiology-24859-24859. Published May 6, 2019.
10. Ballachanda B, Abrams H, Hal III JW. Tele-audiology in a pandemic and beyond: Flexibility and suitability in audiology practice. Audiology Today. https://www.audiology.org/audiology-today-julyaugust-2020/tele-audiology-pandemic-and-beyond-flexibility-and-suitability. Published July/August 2020.
11. Campbell W. Phonak ABCs of eAudiology #1: 10 steps to licensure & stakeholder support for eAudiology [Part 1 of 10-part series]. Hearing Review. Published August 26, 2019.
12. Fabry D, Groth J. Teleaudiology: Friend or foe in the consumerism of hearing healthcare? Hearing Review. 2017;24(4):16-19.
13. Bailey A. Remote care apps: Comparing the options. ENT & Audiology News. https://www.entandaudiologynews.com/features/audiology-features/post/remote-care-apps-comparing-the-options. Published June 26, 2020.
14. Copithorne D. Hearing aid help at home: Remote hearing care and teleaudiology. Hearing Tracker. https://www.hearingtracker.com/services/remote-care?_ga=2.123743501.624289828.1596818976-931849682.1596818976. Published April 5, 2020.
15. Montano J, Angley G, Ryan-Bane C, et al. eAudiology: Shifting from theory to practice. Hearing Review. 2018;25(9):20-24.
16. Statista. Number of smartphone users in the United States from 2018 to 2024 (in millions). https://www.statista.com/statistics/201182/forecast-ofsmartphone-users-in-the-us. Published 2020.
17. Swanepoel DW. The need for tele-audiometry. Hearing Review. 2012;19(10):18-25.
18. Sandström J, Swanepoel DW, Myburgh HC, Laurent C. Smartphone threshold audiometry in underserved primary health-care contexts. Int J Audiol. 2016;55(4):232-238.
19. Bornman M, Swanepoel DW, De Jager LB,Eikelboom RH. Extended high-frequency smartphone audiometry: Validity and reliability. J Am Acad Audiol. 2019;30(3):217-226.
20. Etymotic. Home Hearing Test. https://www.etymotic.com/consumer/home-hearing-test/home-hearing-test.html.
21. Margolis RH, Moore BCJ. AMTAS: Automated method for testing auditory sensitivity: III. Sensorineural hearing loss and air-bone gaps. Int J Audiol. 2011; 50(7:440-447.
22. Margolis RH, Frisina R, Walton JP. AMTAS: Automated method for testing auditory sensitivity: II. Air conduction audiograms in children and adults. Int J Audiol. 2011;50(7):434-439.
23. Margolis RH, Glasberg BR, Creeke S, Moore BCJ. AMTAS: Automated method for testing auditory sensitivity: Validation studies. Int J Audiol. 2010;49(3):185-194.
24. Margolis RH, Saly GL, Le C, Laurence J. Qualind: A method for assessing the accuracy of automated tests. J Amer Acad Audiol. 2007;18:78-89.
25. Mosley CL, Langley LM, Davis A, McMahon CM,Tremblay KL. Reliability of the Home Hearing Test: Implications for public health. J Am Acad Audiol. 2019;30(3): 208-216.
26. iHear Medical. iHEARtest. https://store.ihearmedical.com/ihear-test-kit-rx.html.
27. Watson CS, Kidd GR, Miller JD, Smits C, Humes LE. Telephone screening tests for functionally impaired hearing: Current use in seven countries and development of a US version. J Am Acad Audiol. 2012;23(10):757-67.
28. National Hearing Test (NHT) website. The National Hearing Test. https://www.nationalhearingtest.org/wordpress/?page_id=2730.
Correspondence can be addressed to Dr Ballachanda at: [email protected].
Citation for this article: Ballachanda B. How to use teleaudiology technologies in a new setup or in an existing office. Hearing Review. 2020;27(8):10-32.