Practice Management | April 2017 Hearing Review
Part 2: Preparing for your level of implementation and involvement in telepractice
By Bopanna Ballachanda, PhD
Interested in building a teleaudiology program into your existing hearing care practice or organization? Part 1 of this series offered some practical advice, as well as 10 items to consider in your planning. Part 2 provides an overview of the equipment, location, and remote staffing requirements depending on your level of implementation and involvement in telepractice.
Part 1 of this series, published in the January 2017 Hearing Review, provided a 10-point checklist to consider when planning a teleaudiology program. It also looked at some basic facts about the global hearing market and how teleaudiology appears to be poised to take on a major role in many countries, including North America. Part 2 provides a basic overview of some of the considerations for establishing a teleaudiology practice. This is certainly not a comprehensive description, as the practice of teleaudiology depends on many factors, such as the type of services being offered and the skill level of the personnel at both ends of the teleaudiology clinics.
First and foremost, factors for starting a teleaudiology program are the identification and successful implementation of software, hardware (technical support from qualified and well-versed personnel and IT support), the appropriate physical environment, and the trained staff at the remote location. Teleaudiology requires highly specialized technology, software, and information networks.
Software Requirements
Careful consideration should be given to the availability of the bandwidth of the Internet and speed of connectivity. Ample bandwidth and ease of connectivity minimizes delays in interactions between locations. It is recommended that the speed remain at a higher level and the bandwidth supports such activities as video conferencing (e.g. video otoscopy, counseling), as well as diagnostic testing.
The software used for patient conferences, testing, and diagnostics must be encrypted and secure. Video conferencing should be secure and HIPAA compliant, and there are several commercially available software for such use (Skype is not secure and, therefore, is not HIPAA compliant). The software used for connectivity should be able to access the remote computer and be compatible for peripheral devices, such as audiometers, immittance devices, video otoscopes, and any hearing aid programming devices. One should pay close attention to avoiding any cross talk and interference between peripheral devices.
Equipment Needs
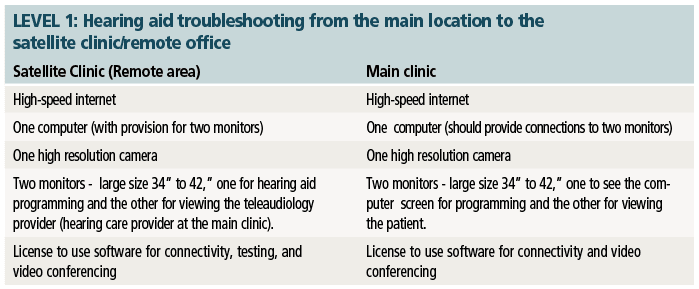
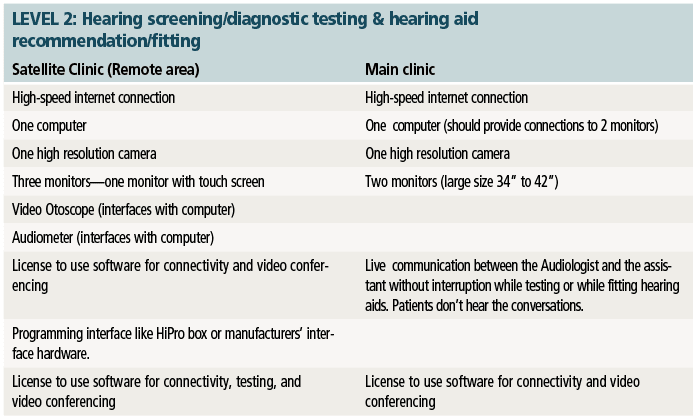
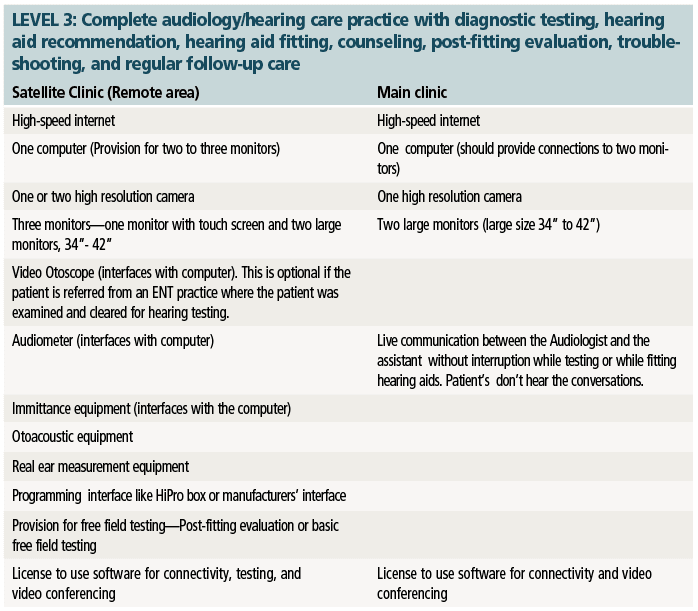
For this paper, the teleaudiology practice will use the Point-to-Point connection and the equipment requirements will be based on the needs of each clinic and the direction that clinic takes in providing the services. Therefore, in the tables shown on the next page, Levels 1-3 have been identified as possible audiology care levels, with Level 1 being very basic and Level 3 as comprehensive services similar to that of a face-to-face encounter.
Physical Environment
The teleaudiology team must determine the space that will provide acceptable levels of privacy, lack of distractions, and very minimal background noise. Other environmental conditions that may affect the quality of the encounter—in particular when video-based services are offered—should also be considered. The provider’s and the patient’s room/environment should ensure privacy to prevent unauthorized access. Seating and lighting should be designed for both comfort and professional interaction.
Although it may be apparent, accommodations for vision and hearing impairment need to be taken into account. Both provider and patient cameras should be placed on a secure, stable platform to avoid wobbling and shaking during the videoconferencing session. The provider and patient should be readily visible and easily heard. To the extent possible, the patient/provider cameras should be placed eye-level with the face clearly visible.
The testing room should be adequately large to accommodate the test equipment, monitor, and the camera. The main location should also maintain a professional look by minimizing clutter and poor lighting.
Selection of Staff at Remote Location
Traditional delivery of hearing care involves patient and hearing care provider communication and interaction in a real-time, in-person encounter. At this encounter, the clinician obtains the patient history, performs an otoscopic inspection, and conducts a hearing evaluation. From the information collected, the provider then carefully plans a course of action to mitigate the patient’s communication problems. The course of action may involve referring to an ENT consult or recommending hearing aids. In any case, the process during the face-to-face encounter should be easy and effective, as this method has been reviewed and refined over the years in hearing care practice.
The use of teleaudiology has extended the reach of the provider, but also may create situations in which assistance is needed in facilitating clinical data transfer from the remote patient setting. A qualified, well-trained person is frequently used as a facilitor (remote staff) to address the challenges that the consulting provider faces when conducting an audiologic examination using teleaudiology and to ensure efficient information exchange.
The remote staff is typically one individual, located at a remote site to support the patient and main-location provider interaction in completing the needed work. Some of the personnel suggested as remote staff are audiology assistants and technicians, registered nurses, licensed practical nurses, and trained telehealth clinicians.
Patient Requests for Records & Billing
The provider should establish an explicit process for patients to request copies of their teleaudiology encounters at their request and to facilitate specialty care, where indicated.
Prior to providing patient services, the patient should be made aware of the cost of the services provided, if any. Arrangement for payment should be completed prior to the delivery of the service. Special consideration must be made for Medicare patients participating in teleaudiology care. Providers need to follow Medicare rules for billing patients outside of standard Medicare reimbursement.
CORRESPONDENCE can be addressed to HR or Dr Ballachanda at: [email protected]
Citation for this article: Ballanchanda B. Critical steps in establishing a teleaudiology practice, Part 2: Preparing for your level of implementation and involvement in telepractice. Hearing Review. 2017;24(4):20-21.

About the author: Bopanna B. Ballachanda, PhD, holds a doctoral degree in auditory neurophysiology and was the founder and CEO of a large multi-state practice with offices in Arizona, New Mexico, and Texas. He is a board member of the American Academy of Audiology (AAA), and has worked as an Assistant Professor of Audiology at Purdue University and an Associate Professor in Speech and Hearing Sciences and an adjunct Associate Professor in the Department of Otolaryngology at the University of New Mexico. He currently is retired from private practice and serves as a consultant to practice owners who wish to delve into the area of teleaudiology.