Tech Topic | September 2019 Hearing Review
The RRT is an integrated speech test that provides a platform for individualized counseling. The goal is to provide a better understanding of each patient’s communication difficulties, then use that understanding to set realistic expectations. We believe the use of this tool, along with other tools that allow individualized fine-tuning, could help promote greater patient satisfaction for hearing aids.
In a previous paper, we introduced the Repeat-Recall Test (RRT) as an integrated validation tool that combines speech-in-noise (SIN) testing at realistic signal-to-noise ratios (SNR), estimation of auditory working memory capacity, ratings of listening effort and tolerable time (or willingness to stay in noise).1 The test has been useful in demonstrating the efficacy of a variable speed compressor2 and of a directional microphone and noise reduction algorithm.3 More recently, we collected norms for the RRT from normal-hearing listeners tested under 4 noise configurations.4 These normative data could be useful during patient counseling in setting realistic expectations for their hearing aids. We believe that setting a realistic expectation could enhance the patient’s real-world satisfaction with the recommended hearing aids.
Of course, patients may have many needs and different levels of expectations for each need. In this discussion, we focus only on speech understanding.
How Can Data on Normal-hearing Listeners Promote Satisfaction?
Satisfaction depends on meeting expectations. Kochkin5 showed that satisfaction with hearing aids (HAs) depends on the noted performance benefit to hearing, sound quality, and their value. The Expectancy-Disconfirmation model,6 borrowed from consumer research, states that consumers are satisfied with their purchase if the performance of the product (in this case, hearing aids) meets or exceeds their expectations. This is called positive disconfirmation. Otherwise, they will be dissatisfied with the purchase or negative disconfirmation.7
Having the “right” expectation is key to satisfaction. It has been reported that higher pre-fitting expectations lead to higher reports of satisfaction.8 However, too high an expectation could lead to negative disconfirmation.9 While one may purposely lower a patient’s expectations to increase the likelihood of satisfaction (eg under-promise and over-deliver),10 how to do so without the negative consequence of demotivating the patient is unclear. Indeed, various researchers have attempted to set the right amount of expectations during pre-fitting to ensure post-fitting satisfaction with conflicting findings.11-14 Recently, Grimmelikhuijsen and Porumbescu15 from public opinion research showed that satisfaction is enhanced when information on performance is revealed before setting the final expectation. That is, expectation is dynamic and can be realigned from knowledge of the performance.
Expectations need to be realistic. It is reasonable for new hearing aid candidates to desire normal-hearing performance from their hearing aids. As hearing care professionals, we recognize that such an expectation is unrealistic. We are aware that not all current hearing aids have the same requisite level of technology, and not all candidates have the cognitive, physical, and psychophysical ability to fully utilize the benefits afforded by the devices. For example, if a wearer expects to hear well in noise, the hearing aid must have algorithms that can improve SNRs. In addition, since all algorithms that attempt to improve SNRs perform optimally under specific conditions, the wearers must know what these conditions are so they can rightly expect improvement in those conditions and not experience dissatisfaction when there is no improvement in others. Finally, if individuals have poor speech understanding ability even in quiet (which would be a prerequisite for speech understanding in noise), then it is not realistic to expect good speech understanding in noise, despite algorithms that may enhance SNRs.
To ensure that the patients’ expectations for their hearing aids are realistic, one must understand if the patients have the potential (cognitive, physical, and financial etc) to achieve such expectations. One must also select hearing aids that have the documented technology that meets the patients’ expressed needs and to make sure that the patients know when and how to use the technology correctly. To achieve these objectives, the clinician must gather insights about the patients’ abilities, such as speech understanding ability in quiet and in noise, working memory, auditory processing skills, etc. The information on the hearing aid and the patients’ abilities should be discussed with them in order to set realistic expectations.
But there may be more. Some patients may continue to be dissatisfied with their hearing aids despite reasonably good SIN test results in the clinic. This observation is frequently reported in new hearing aid wearers rather than in experienced wearers (eg, see Cox and Alexander16), and may reflect the unrealistic expectation that hearing aids should restore hearing in a way that is free of difficulties with speech understanding. Experienced hearing aid wearers know that this is not the case and are more realistic in their expectations. Thus, if one were able to help patients realize that even normal-hearing listeners have difficulties with understanding speech in noise, and that their performance with the recommended hearing aids is comparable to normal-hearing listeners, then these wearers may be more willing to accept (and be satisfied with) their hearing aids.
Having normative data on a speech-in-noise test may help to set realistic expectations. To achieve that, we need to have relatable data on normal-hearing listeners for the speech tests that we use. If the patients’ performance with their hearing aids is similar or better than that of normal-hearing listeners, they may understand that any difficulties they experience in real life are not the fault of the device, but rather typical of normal-hearing listeners. This may convince patients into accepting their hearing aids.
On the other hand, if the comparison shows that the patients’ performance is poorer than their normal-hearing peers, this alerts the clinician to seek alternative strategies (such as use of more advanced technology, assistive devices, use of communication strategies, etc) to improve the fitting. This could enhance the ultimate performance of the device which benefits both the clinician and the patients. If nothing can be done to further improve performance because of the patients’ limitations (such as cognitive issues, etc), then the clinician can use the opportunity to explain why no further enhancement is possible.
This directed counseling could deepen the patients’ understanding of their limitation. Both actions could help the patients realign their expectations and improve satisfaction. This approach is in line with Grimmelikhuijsen and Porumbescu’s observation that having performance information could realign a respondent’s expectations to yield higher satisfaction.15
Desired Features of a Normative Speech in Noise Test
Covers a range of real-life situations. Normative data should be available over a range of realistic SNRs17collected with different amounts of contextual cues under different noise configurations. This would allow the test to approximate many of the various real-life situations likely to be experienced by the patients. This may also help explain why a patient has difficulties in some situations but not others, and provides a goal for both the dispensers and the patients to achieve “normal” performance in problematic areas.
Measures more than speech in noise. In order to gain a deeper understanding of the possible factors affecting performance, the test should include other measures that are known to affect speech in noise ability. This includes speech in quiet score, working memory, listening effort rating, tolerance for noise, communication needs, etc. Indeed, the more integrated information one can convey to the patient during the counseling session, the more realistic their expectations may become.
Offers a platform for patient counseling. The results of the test must be summarized and presented in a clear manner for patient counseling. Patients should understand how their performance compares to their normal-hearing peers. However, it must be made clear that “normal performance” is only specific to the particular test, under that specific test condition. It does not mean “normal hearing” in the strictest sense and the results may not be generalized to all other life situations.
For example, assume a patient’s performance with a directional microphone is similar to how normal-hearing listeners perform with a speech-front, noise-back configuration. The patient should be informed of the findings and be encouraged to structure his/her communication environments to result in such a configuration as much as possible. This instruction not only provides the patient with a realistic expectation for the hearing aids, but also offers a strategy for dealing with communication in noise. In the process, the patient may also appreciate the benefits that technology offers.
How to Use RRT as a Tool to Help Set Realistic Expectations
The following outlines how the RRT may help set realistic expectations. For a more detailed description on the RRT development and validation, please see Slugocki et al.1
RRT is a sentence test using everyday speech materials. Briefly, the RRT draws speech materials from five sets of thematically related sentences. The themes include Food & Cooking, Books & Movies, Music, Shopping, and Sports. Under each theme, 7 lists of 6 sentences (in a list) are available, so that a unique list may be used for each SNR. Each sentence contains 3 to 4 target words (mostly nouns, adjectives, and verbs) so that 20 target words are scored for every list. All sentences are targeted at a 4th-grade reading level.
RRT assesses how listeners use context. There are two versions of the test that differ in the degree of available contextual information. High context (HC) sentences are meaningful sentences that are related to the same theme (or topic), such that listeners can draw upon within-sentence and between-sentence cues to word identity. Low context (LC) sentences are generated by randomizing target words among the HC sentences in a list. This process results in six sentences that are syntactically valid, but semantically meaningless. Both versions of the test must be administered if one is interested in assessing the use of context.
RRT tests over a range of realistic SNRs in 4 noise configurations. The RRT is conducted with the sentence materials presented from the front at a level of 75 dB SPL in quiet, and with background noise at SNRs of 0, 5, 10, and 15 dB. These SNRs are reported by Smeds et al18 and Wu et al19 to be frequently encountered by hearing-impaired listeners in their real-life situations. The test also features four noise configurations: 2-talker babble noise and speech-shaped continuous noise presented either from the front or the back.
RRT produces 4 outcome measures. To recap, the RRT measures:
1) Repeat: Speech understanding at each SNR;
2) Recall: Evaluates the listeners’ recall ability of the repeated sentences to yield an estimate of their working memory capacity20
3) Effort:Surveys the amount of listening effort required to understand speech at the particular SNR, and
4) Tolerance time: Assesses how much time the patients are willing to spend listening under that condition.
During each trial (one SNR and one context), the patients repeat each of the 6 sentences after they have heard them (repeat stage). After all 6 sentences are repeated, they recall as many of them as possible (recall stage). Afterwards, they rate how effortful it is to listen in the specific SNR condition (listening effort score) on a scale from 0 to 10. They then estimate how much time they are willing to spend communicating in the specific SNR condition (tolerable time).
Repeat performance across tested SNRs provides information on the patients’ speech-in-noise ability. Reported listening effort gives an indication of how patients perceive their ease of communication and could reflect their real-life perception of communication difficulty.21 Recall performance provides an estimate of the patient’s working memory capacity; we have shown recall scores to be correlated with performance on the Reading Span test (RST).1,22
Various researchers21,23-27 have suggested that working memory capacity may help to explain a person’s speech-in-noise ability. Knowing the patients’ working memory capacity may also help in selecting the best form of signal processing.28,29 Tolerable time reflects the patients’ willingness to listen in the specific noisy environment. One would expect that tolerable time to increase as SNR improves. On the other hand, if a patient’s tolerable time does not improve with increasing SNR, or if this tolerable time is extremely short (relative to normal-hearing people), then it could suggest that the individual may have a general dislike for communication in noise. This could alert the clinician that the patient may likely be dissatisfied with the hearing aids unless all traces of noise can be removed.
Thus, all four outcome measures can be useful as validation tools and profiling measures to gather insights into the patient’s communication performance.
The test can be administered quickly and has a Quick RRT option. Each SNR by context trial takes approximately 2 minutes to complete. Thus, a complete test that covers both contexts each at 5 SNRs (or 10 trials) takes approximately 20-25 minutes. This will provide a complete performance intensity function (from SNR = 0 dB to 15 dB and quiet) for both types (HC and LC) of speech materials under all four outcome measures in one noise configuration.
An abbreviated version, the Quick RRT, requires speech in noise (Repeat) testing of only the LC materials at SNRs of 5, 10, and 15 dB, and Recall testing only for HC materials at SNR = 15 dB. This shortens the test time to 6-8 minutes while providing an estimate of the patient’s speech in noise ability, and the associated effort and tolerable time ratings at the critical SNRs, as well as an estimation of the listener’s working memory capacity.
Norms on normal-hearing listeners are available for the RRT. The RRT includes normative data collected on 21 normal-hearing listeners between 51 and 78 years of age (average age: 61.7 years) in 4 noise configurations. All scored higher than 23 on the Montreal Cognitive Assessment (MoCA),30 suggesting no cognitive impairment. Their scores were used to establish the percentile distribution on each outcome measure. Briefly, the percentile score reflects an individual’s performance relative to the normative sample. For example, a percentile score of 20 suggests that the individual’s performance is better than 20% of the normative sample.
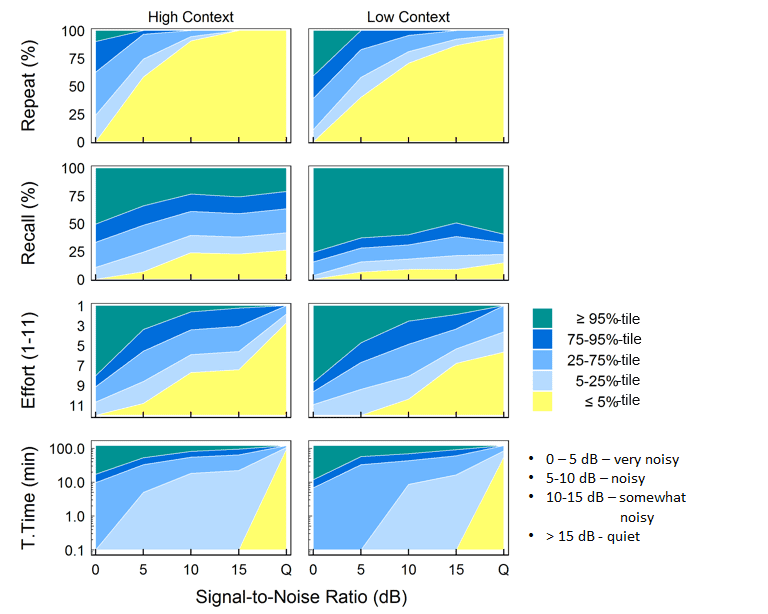
For ease of comparison, we used different shades of blue to color code scores between the 5th and 95th percentiles (Figure 1), which shows an example of the normative template displayed in the RRT software for continuous noise presented from the back. Scores that are poorer than the 5th percentile are displayed in the yellow region while those better than the 95th percentile are in the green region. Scores in the medium blue zones would suggest performance comparable to the average normal-hearing listeners. This template is available for all 4 noise configurations and for each outcome measure. In addition to showing the actual SNRs that are tested, the test levels are also labeled with consumer-friendly terms adapted from Wu et al19 to make them easier to understand.

Figure 1. An example of the normative template for a speech front, continuous speech-shaped noise from the back configuration. In the graphic display of the RRT, different shades of blue signify scores between the 5th and 95th percentiles. Scores that are poorer than the 5th percentile are displayed in the yellow region while those better than the 95th percentile are in the green region. Scores in the medium blue zones suggest performance comparable to the average normal-hearing listener. This template is available for all 4 noise configurations (0, 5, 10, 15 dB SNR) and for each of the 4 outcome measures (Repeat, Recall, Effort, and Tolerance Time).
RRT provides a platform for individualized counseling. Research on realistic expectations suggests that generic counseling does not improve satisfaction.11 Instead, to be effective, counseling must be relevant to the patient. A comparison of the patient’s performance on the RRT to that of normal-hearing listeners allows the clinician to pinpoint specific problem areas where additional fine tuning, selection of alternative devices, or focused counseling may be provided.
Examples of How the RRT is Used to Enhance Customer Satisfaction
When a patient’s scores on the four outcome measures of the RRT are compared to those of normal hearing listeners, it helps provide insights into the patient’s communication difficulties and allows the clinician to plan for the next step of intervention. In addition, it allows a comparison of product/feature efficacy.
The following case examples illustrate these potential uses.
Case 1: Convincing the benefits of hearing aids. An active 80-year-old female with a flat 40 dB hearing loss in both ears reported “normal” hearing while admitting occasional problems with speech understanding in quiet and in noise (Figure 2). Unaided testing with the RRT showed that her speech in noise ability and her working memory capacity were in the 25th percentile of normal-hearing listeners. Her listening effort was similar to that of average normal-hearing listeners. Her tolerable time was around 10 minutes at all realistic SNRs (5 to 15 dB), suggesting that she may not like to communicate in noise over any extended period. The unaided RRT scores showed that she was not as “normal” as she thought she was in her speech understanding ability. It also explained why her speech understanding problem was not consistent (ie, changes with SNRs). It confirmed that her speech in noise ability may be improved.
The patient reported no noticeable difference between the aided and unaided conditions while she was conversing with the test administrator in quiet. Despite this, her performance on all measures of the RRT improved from the bottom 25th percentile to the 50th percentile at the lower SNRs (Case 2: Demonstration of feature benefits in a patient with good working memory. Figure 3 shows the aided performance of a 70-year-old male retired air traffic controller at two hearing aid settings. On the left is the performance with an omnidirectional microphone, while on the right is that with a directional microphone.

Figure 3. Example of the aided RRT with omnidirectional microphone (on left) and directional microphone (on right) for Case 2.
With an omnidirectional microphone, this patient’s repeat performance was in the 25th percentile, but his recall ability was in the top 75th percentile. This suggests that his working memory capacity is most likely above average. Furthermore, his rating of listening effort and tolerable time improved as SNR improved. These observations suggest that despite the hearing loss, this person can likely appreciate changes in SNR. Conveying this information to the patient and noting the optimistic reasons for improved performance with technology could be motivating to the patient to set higher, yet realistic expectations.
With a directional microphone, this patient’s performance on all measures of the RRT is at least as good as, if not better than, the average normal-hearing listener at most SNRs.
It was pointed out earlier that for expectations to be realistic, the patient needs to understand when and how to use the technology properly. In our evaluation, the test setup was with noise that originates from the back. This point should be explained to the patient, followed with instructions on how the patient can control his listening environment. He should face the speaker and have noise from his side/back in order to optimally use the directional microphone. Here the RRT provides an opportunity to educate the patient on how his device may be used to obtain maximum benefit.
Case 3: Limited feature benefits for people with poorer working memory. Figure 4 shows the RRT results for an 84-year old male who wore the same hearing aid as used by the patient in Case 2. While his repeat performance with the omnidirectional microphone (left) was also in the 25th percentile category, he differed from Case 2 in that his listening effort was in the bottom 25th percentile, and at the lowest 5th percentile at SNR = 15 dB for LC materials. Additionally, his tolerable time rating showed that he did not want to spend more than 2 minutes under any of the SNRs tested. This suggests that this listener may be aversive to communicating in noise, even when the SNR is relatively favorable. Furthermore, the patient’s recall score was in the bottom 25th percentile, suggesting that working memory may be a limiting factor for improvement from technology.

Figure 4. Example of the aided RRT with omnidirectional microphone (on left) and directional microphone (on right) for Case 3.
A directional microphone was recommended to improve speech-in-noise performance, especially at the poorer SNRs. This technology could also alleviate listening effort. However, because the patient reported no change in tolerable time even with SNR improvement, it may not be optimistic to think that he would find the use of a directional microphone to improve his willingness to stay in noise. Despite the patient’s poorer-than-average working memory capacity, he could still benefit from the use of a directional microphone and noise reduction.3 However, it should be cautioned that performance may still be below that of normal-hearing listeners.
The figure on the right is the patient’s performance with a directional microphone. Repeat scores were improved at all SNRs bringing performance to above the 80th percentile with corresponding improvements to listening effort ratings. Directional microphones benefit people of all working memory capacities.3 However, listening effort scores were still around the 25th percentile, which means that the patient might find listening more effortful than most normal-hearing listeners. As reflected on his tolerable time estimates, the patient was still not motivated to engage in noisy situations for longer than 2 minutes (still in the lower 25th percentile). This may be a result of the patient’s limited working memory, wherein recall scores with the directional microphone also did not improve.
One may question if the news of the patient’s performance in the lower 25th percentile may discourage the patient from trying amplification. An important aspect in adjusting for realistic expectations is a balance between the “good” and the “bad” news. Sometimes letting patients know why they have fallen into the “poor” performance category may help to tone down their expectations and improve satisfaction because the lower expectation can be met.10
Conclusions
The RRT is an integrated speech test that provides a platform for individualized counseling. The goal is to provide a better understanding of each patient’s communication difficulties and using that understanding to set realistic expectations. We believe the use of this tool, along with other tools that allow individualized fine-tuning, could help promote greater patient satisfaction for hearing aids.
Getting Started
If you are interested in using this tool in your clinic, please email the author ([email protected]) for the free link to the test.
Francis Kuk, PhD, is Director; Petri Korhonen, MSc, is a Senior Research Scientist; Christopher Slugocki, PhD, is a Research Scientist, and Neal Ruperto, AuD, is a Research Audiologist at the Widex Office of Research in Clinical Amplification (ORCA) in Lisle, Ill.
Correspondence can be addressed to Dr Kuk at: [email protected]
Citation for this article: Kuk F, Korhonen P, Slugocki C, Ruperto N. How to use the Repeat-Recall Test (RRT) to increase hearing aid satisfaction. Hearing Review. 2019;26(9):32-40.
References
1. Slugocki C, Kuk F, Korhonen P. Development and clinical applications of the ORCA Repeat and Recall Test (RRT). Hearing Review. 2018;25(12):22-26.
2. Kuk F, Slugocki C, Korhonen P. Seper E, Hau O. Evaluation of the efficacy of a dual variable speed compressor over a single fixed speed compressor. J Am Acad Audiol.2019;30(7):590-606.
3. Kuk F, Slugocki C, Korhonen P. An integrative evaluation of the efficacy of a directional microphone and noise reduction algorithm under realistic signal-to-noise ratios. J Am Acad Audiol. 2019; in press.
4. Kuk F, Slugocki C, Ruperto N, Korhonen P. (2019c). Performance of normal hearing listeners on RRT with different noise configurations. Submitted paper.
5. Kochkin S. MarkeTrak VIII: Consumer satisfaction with hearing aids is slowly increasing. Hear Jour.2010;63(1):19-32.
6. Oliver RL, Bearden WO. Disconfirmation processes and consumer evaluations in product usage. J Bus Res. 1985;13(3):235-246.
7. Meyer CJ, Hickson L, Khan A, Walker D. What is important for hearing aid satisfaction? Application of the expectancy-disconfirmation model. J Am Acad Audiol.2014;25(7):644-655.
8. Schum DJ. Perceived hearing aid benefit in relation to perceived needs. J Am Acad Audiol.1999;10:40-45.
9. Garstecki DC, Erler SF. Hearing loss, control, and demographic factors influencing hearing aid use among older adults. J Speech Lang Hear Res.1998;41(3):527-537.
10. Sweetow R. Counseling Strategies for Hearing Aid Fittings. 1st ed. Boston, MA: Cengage Learning;1999.
11. Norman M, George CR, McCarthy D. The effect of pre-fitting counselling on the outcome of hearing aid fittings. Scand Audiol.1994;23(4):257-263.
12. Öberg M, Andersson G, Wänström G, Lunner T. The effects of a pre-fitting intervention on hearing aid benefit: A randomized controlled trial. Audiol Med.2009;7(4):211-225.
13. Saunders GH, Lewis MS, Forsline A. Expectations, prefitting counseling, and hearing aid outcome. J Am Acad Audiol. 2009;20:320-334.
14. Wong LLN, Hickson L, McPherson B. Satisfaction with hearing aids: A consumer research perspective. Int J Audiol.2009;48(7):405-427.
15. Grimmelikhuijsen S, Porumbescu GA. Reconsidering the expectancy disconfirmation model. Three experimental replications. Public Management Review. 2017;19(9):1272-1292.
16. Cox RM, Alexander GC. Expectations about hearing aids and their relationship to fitting outcome. J Am Acad Audiol.2000;11:368-382.
17. Kuk F, Slugocki C, Korhonen P. Better speech-in-noise testing: Demonstration with dual variable speed compression. Hearing Review.2018;25(8):24-28.
18. Smeds K, Wolters F, Rung M. Estimation of signal-to-noise ratios in realistic sound scenarios. J Am Acad Audiol.2015;26(2):183-196.
19. Wu Y-H, Stangl E, Chipara O, Hasan S, Welhaven A, Oleson J. Characteristics of real-world signal to noise ratios and speech listening situations of older adults with mild to moderate hearing loss. Ear Hear. 2018;39(2):293-304.
20. Baddeley A, Hitch G. Working memory. In: Bower GH, ed. The Psychology of Learning and Motivation: Advances in Research and Theory, Vol 8. 1st ed. New York, NY: Academic Press;1974:47-89.
21. Pichora-Fuller KM, Kramer SE, Eckert MA, et al. Hearing impairment and cognitive energy: The Framework for Understanding Effortful Listening (FUEL). Ear Hear.2016;37[Supp]:5S-27S.
22. Van den Noort M, Bosch P, Haverkort M, Hugdahl K. A standard computerized version of the Reading Span Test in different languages. Eur J Psychol Assess. 2008;24(1):35-42.
23. Lunner T. Cognitive function in relation to hearing aid use. Int J Audiol. 2003;42[Supp 1]:S49-S58.
24. Akeroyd MA. Are individual differences in speech reception related to individual differences in cognitive ability? A survey of twenty experimental studies with normal and hearing-impaired adults. Int J Audiol. 2008;47[Supp 2]:S53-S71.
25. Rönnberg J, Rudner M, Foo C, Lunner T. Cognition counts: A working memory system for Ease of Language Understanding (ELU). Int J Audiol. 2008;47[Supp 2]:S99-S105.
26. Rudner M, Rönnberg J, Lunner T. Working memory supports listening in noise for persons with hearing impairment. J Am Acad Audiol.2011;22(3):156-167.
27. Besser J, Koelewijn T, Zekveld AA, Kramer SE, Festen JM. How linguistic closure and verbal working memory relate to speech recognition in noise–A review. Trends Amplif. 2013;17(2):75-93.
28. Ng EHN, Rudner M, Lunner T, Pedersen MS, Rönnberg J. Effects of noise and working memory capacity on memory processing of speech for hearing-aid users. Int J Audiol. 2013;52(7):433-441.
29. Souza P, Arehart K, Neher T. Working memory and hearing aid processing: Literature findings, future directions, and clinical applications. Front Psychol.2015;6:1-12.
30. Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc.2005;53(4):695-699.