Tele-health in Brazil: Strategic action to enhance the provision of services
Therapeutic patient education (TPE) is a process designed to help individuals gain or refine their knowledge and necessary skills to cope with an illness in the best way possible. It is a patient-centered ongoing process, and it includes attention, information, self-care teaching, and psychosocial support. This article describes some TPE initiatives that are being employed within Brazil’s tele-audiology program.
The Brazilian Unified Health System (known as the SUS), created in 1988, is one of the largest public health care systems in the world. Currently, 80% of the Brazilian population relies exclusively on SUS services.
SUS activities must be governed by its doctrinarian (universality, equitability, and comprehensiveness of care) and organizational principles (decentralization, network’s regionalization and hierarchization and social participation). The SUS network is organized by region and with increasing levels of complexity: primary health care is the preferential and first contact point in the system, encompassing individual and/or collective interventions, from health promotion to rehabilitation; secondary and tertiary care are provided by a network of public clinics/hospitals, as well as private and university hospitals under SUS contract.1
Brazil`s ethnically and culturally diversified population of 192 million is sparsely distributed in an area of 8.5 million km2 (by comparison, this would be analogous to about 60% of the US population living in 90% of the USA’s area). Despite its growing economy, Brazil has one of the world’s most unequal distributions of income, leading to major socioeconomic contrasts. The infrastructure and qualified human resources distribution are also very heterogeneous. Given such a scenario, assuring health care equity, comprehensiveness, and universality remains a challenge. Therefore, inequalities are also part of the SUS system: world-class health programs coexist with poor service conditions and only 1.9% of the population lives in cities with high IDSUS—an index based on the offering and effectiveness of services provided.2
Approximately 13 million (6.8%) Brazilians have a disabling hearing impairment.3 Since the 90s, SUS has invested in hearing healthcare, yet, only in 2004, when the “National Hearing Healthcare Policy” was published, was integral care guaranteed. Free-of-charge services from prevention to treatment—including hearing aids (HA) dispensing and cochlear implant (CI) surgeries —must be provided. Currently, there are 66 secondary and 82 tertiary hearing healthcare centers, as well as 25 CI services accredited by SUS. However, the hearing healthcare network is still in development: 64% of services are in or around urban centers in the South and Southeast of the country.4 Patient transportation for treatment in other regions burdens the health system with travel costs, and patients with wages and time lost.
Manpower constraints also pose an important obstacle. Only 5.3% of the nearly 36,000 dual-certified professionals (Speech Language Pathologists/Audiologists) are audiology experts, and 70% of them are located in the Southeast region.5
In 2011, the Federal Government launched the “National Plan on the Rights of People with Disabilities,” with investments in education, health, social inclusion, and accessibility, aiming to intensify actions already in place and implement new initiatives.6 Therefore, improvements in public hearing healthcare are expected in the near future.
Tele-health has had an important development and consolidation in Brazil, thanks to grants offered by research funding agencies and governmental actions, as well. Of particular importance was the creation of the “Permanent Tele-health Commission” by the Ministry of Health, in 2006, bringing together various ministries, governmental agencies, university researchers, and other entities to share knowledge and plan a cooperative strategy for the implementation and development of Brazilian tele-health. In 2007, the “Tele-health Brazil Program” was launched with the general aim of improving the quality of primary health care countrywide. In addition to other goals in education and assistance was the assembling of information and telecommunications technology (ICT) infrastructure for the development of tele-health actions.7
In 2010, this program was redefined and expanded, yielding the “Tele-health Brazil Networks,” with the aim of improving the quality of services in all levels of care, integrating educational institutions and services by means of ICTs to conduct synchronous and asynchronous tele-education, teleconsultation, and formative second opinions.8 This program encompasses:
- Technical-Scientific Tele-health Nuclei comprised of educational institutions and/or health care units/managers responsible for the formulation and management of tele-health services.
- Tele-health Points, service locations through which community health workers and professionals access/demand tele-health services.
Currently, there are 11 Tele-health Nuclei and more than 1,500 Tele-health Points, the majority at the primary care level, distributed in 950 cities in Brazil (Figure 1).
Our department is part of the “São Paulo Tele-health Nuclei,” and our tele-audiology actions began with tele-education in the late 1990s. Although the incorporation of tele-health in the SLP-Audiologist’s practice was legalized in Brazil in 2009, its role for hearing aid services in the public system has been one of our research subjects since 2004. Some of our experiences concerning the provision of patient education are described below.
Teleaudiology and Therapeutic Patient Education
The socio-cultural transformations occurring in the last decades changed the expected patient role from passivity to active involvement, sharing with the health care professional the responsibilities for the treatment process and outcomes. In this context, a key element is therapeutic patient education (TPE)—a process designed to help individuals gain or refine their knowledge and necessary skills to cope with an illness in the best way possible. It is a patient-centered ongoing process and includes attention, information, self-care teaching, and psychosocial support.
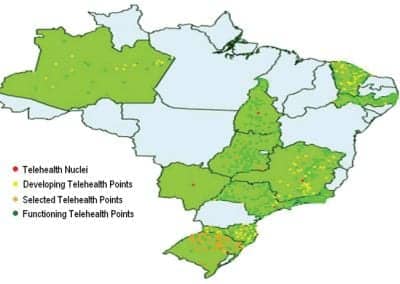
Figure 1. In Brazil’s Unified Health System, there are 11 Tele-health Nuclei and more than 1,500 Tele-health Points located in 950 cities.
TPE benefits include better patient-professional communication and understanding of the disease and its treatment, greater information retention and patient improvement on self-management and coping skills, improved quality of life, greater adherence to treatment and better use of time and resources, reducing treatment costs for patients and society.9 Informational and personal adjustment counseling used in audiology is part of therapeutic patient education.
Patients with a chronic disease, such as sensorineural hearing loss, usually require treatment based on self-management (eg, appropriate hearing aid use) and continuity of care, because the disease might progress and/or patient needs might change. Studies of individuals enrolled in the SUS hearing healthcare system showed that, in 52% to 80% of cases, hearing aid use difficulties and complaints could be solved with patient education.10,11 Also, the number of follow-up visits conducted in the system is still lower than expected—probably the result of difficulties in access to services and/or reduced treatment adherence.12 This data is alarming when considering that, in 2010, considering hearing aid dispensing only, SUS spent about US$60 million.4

Figure 2. A patient and study participant during a teleconsultation that included the issue of insertion/removal of the hearing aid. Rarely does the patient ask for the teleconsultation facilitator’s help.
Teleaudiology can be an advantageous means to replace or supplement traditional services to facilitate TPE. Regarding adults, daily e-mails were convenient for patients and useful for the audiologist to explore new hearing aid users’ everyday experiences, allowing for the observation in changing initial behavior and perceptions after fittings.13
We conducted a randomized controlled blind study where topics such as hearing aid/earmold care, maintenance, and use, as well as hearing aid expectations and communication strategies were discussed/presented to 50 new hearing aid users assigned to control (face-to-face) or experimental (teleconsultation) groups. The participants were active during teleconsultations, striving to accomplish the tasks (eg, hearing aid insertion/removal) demonstrated via videoconference (Figure 2) and rarely asking for the teleconsultation facilitator’s help. At the follow-up, there was no difference between the groups on what related to hearing aid usage, care, and handling.14
This data supports teleconsultation as a viable vehicle for TPE delivery, for example, in primary health care, thus avoiding unnecessary referrals and supporting adherence to treatment at the same time. Appropriate ICT infrastructure and bandwidth are already available at Tele-health Points (Figure 1) and will be expanded in the future.
Nevertheless, there are challenges in communicating with hearing-impaired individuals via teleconsultations, such as the need for high-quality audio and video transmission at all times. Nonverbal communication that conveys important affective messages might be prevented (eg, touch) or hindered (eg, eye contact), possibly causing an impact in patient sheltering. Also, since Brazilian culture emphasizes personal relationships, teleconsultations might not always be accepted, especially when socio-emotional issues are to be addressed in a session. These and other aspects are currently under investigation by our group.
Therapeutic education must also be provided to families of hearing-impaired children. The presence of a hearing-impaired child raises a number of issues in a family, and their members often need to redefine their roles and learn new values, skills, and behavior patterns to cope with the situation. Parents need support and information throughout the process, from diagnosis to intervention, enabling them to make informed choices.15,16 Participation in support groups is also of great value since insights and inter-group relations contribute to better coping and empowerment of families.
Internet-based videoconferencing has been used to provide coaching to over 170 families of hearing-impaired children in rural areas. Participants considered it an effective method for service delivery. Early-intervention providers found that, since parents are the primary participants of such consultations, they acquire educational skills more rapidly than in traditional sessions.17

Figure 3. The Babies’ Portal Web site is designed to provide families with convenient access to information about hearing aid characteristics, use, and trouble-shooting.
Internet features also make it a unique medium for TPE provision. The possibilities of using multimedia in an interactive environment allow for the production of educational materials with a multisensory appeal and potential for improving information understanding and retention. Parents of deaf children look for both hearing loss information and social support on the Internet, and approximately 50% of them participate in online support groups or e-mail listings.18 Although not always easily understandable, Internet information influences parental decisions regarding their child’s treatment.19 However, it must be emphasized that the quality of information available online cannot be guaranteed, and many times parents find sources that are incomplete, inaccurate, or even fraudulent.
With this in mind, we developed the “Babies’ Portal” (http://portaldosbebes.fob.usp.br), an interactive Web site for parents of children with communication disorders. The Web site’s hearing aid section provides families with convenient access to information regarding hearing aid characteristics, care, use, and trouble-shooting (Figure 3).
Accessing this Web site significantly improved parents’ information retention by 17% in comparison to reading hearing aid manuals.20 Technical and content quality evaluation of the Web site`s hearing aid section showed that content, accuracy, author, currency, audience, navigation, external links, and structure were rated as “excellent” by at least 67% of audiologists. Approximately 65% of parents rated contents as “good” or “very good” and stated the Web site helped them solve their main doubts concerning HA use.21
An ongoing randomized controlled study is evaluating the effect of participation in the Babies’ Portal online social network in stress reduction in parents of children CI candidates (Figure 4). At the time of this writing, the data was still insufficient for statistical analysis; however, it was already possible to observe messages conveying feelings of identification, empathy, and encouragement between participants.

Figure 4. A section of the Web site provides a social-media experience for parents of children with hearing loss to share their experiences with other parents, including those parents of children with cochlear implants.
Summary and Conclusions
In Brazil there are still barriers for the widespread use of the Internet for TPE. One is the digital divide: more than 65% of Brazilians over 10 years old do not access the Web, mostly for lack of access or knowledge in computer use. Internet penetration is still greater in classes with higher educational and economic levels.22 Another barrier is illiteracy, since most of the contents are presented in written format. Last, but not least, is broadband connection, which is not available countrywide, despite its 74% growth in the last year (mainly due to mobile access). Also, these services are expensive when compared to income and the average connection speed is still low.
However, the future is promising: the federal government is focusing on boosting broadband and reducing its costs. The goal is to achieve, by 2014, 30 million fixed lines and 60 million mobile users. Also, there’s a constant increase in smartphone sales, thanks to more affordable devices and data packages. Mobile device usage is already redefining tele-health’s shape and will expand the possibilities for creative and affordable solutions for TPE delivery. Stay tuned.
Under the light of public hearing healthcare, tele-audiology must be seen as a strategic action that can enhance the coordination, organization, rationalization, and provision of services. On those issues that relate to therapeutic patient education, tele-audiology allows for maximizing efficiency, access, and support, as well as tailoring of specific programs to meet patient/family needs.
Acknowledgments
The author thanks the colleagues and graduate students of SLP-Audiology Department and São Paulo Tele-health Nuclei who contributed for the projects’ development.
CORRESPONDENCE can be addressed to:
References
- Portal da Saúde. Entendendo o SUS. Available at: portal.saude.gov.br/portal/saude/cidadao/area.cfm?id_area=1395
- Ministério da Saúde. Índice de desempenho do Sistema Único de Saúde. Available at: portal.saude.gov.br/portal/saude/area.cfm?id_area=1080
- Béria JU, Raymann BC, Gigante LP, et al. Hearing impairment and socioeconomic factors: a population-based survey of an urban locality in southern Brazil. Rev Panam Salud Publica. 2007;21(6):381-7.
- Ministério da Saúde. Departamento de Informática do SUS. Available at: www2.datasus.gov.br/DATASUS/index.php
- Conselho Federal de Fonoaudiologia. Número de fonoaudiólogos do Brasil por estado. Available at: www.fonoaudiologia.org.br
- Secretaria Nacional de Promoção dos Direitos da Pessoa com Deficiência. Viver sem Limite. Available at: www.pessoacomdeficiencia.gov.br/app/viver-sem-limite-0
- Campos FE, Haddad AE, Wen CL, Alkmin MBM, Cury PM. The national tele-health program in Brazil: an instrument of support for primary health care. Latin-Am J Tele-health, Belo Horizonte. 2009;1(1):39-66. Available at: cetes.medicina.ufmg.br/revista/index.php/rlat/article/view/11/3
- Telessaúde Brasil Redes. Nova fase marca expansão para a Telessaúde no Brasil. Available at: www.telessaudebrasil.org.br
- World Health Organization (WHO). The therapeutic patient education: Continuing education programmes for health care providers in the field of prevention of chronic diseases. Copenhagen, Denmark: WHO; 1998.
- Oliveira JRM, et al. Dificuldades encontradas pelos deficientes auditivos adultos, após a adaptação do aparelho de amplificação sonora individual. Acta AWHO. 2001;20(4):201-5.
- Araujo TM, Mendes BCA, Novaes BCAC. Pronto atendimento a usuários de dispositivos de amplificação sonora. Rev Soc Bras Fonoaudiol. 2011; 16(4):466-73.
- Bevilacqua MC, Morettin M, Melo TM, Amantini RCB, Martinez MANS. Contribuições para análise da política de saúde auditiva no Brasil. Rev Soc Bras Fonoaudiol. 2011;16(3):252-9.
- Laplante-Lévesque A, Pichora-Fuller MK, Gagné JP. Providing an Internet-based audiological counselling programme to new hearing aid users: A qualitative study. Int J Audiol. 2006;45(12):697-706.
- Campos PD, Ferrari DV. Tele-audiololgy: Evaluation of teleconsultation efficacy for hearing aid fitting. J Soc Bras Fonoaudiol. 2012 [in press]
- Fitzpatrick E, Angus D, Durieux-Smith A, Graham ID, Coyle D. Parents’ needs following identification of childhood hearing loss. Am J Audiol. 2008;17(1):38-49.
- Van Der Spuy T, Pottas L. Infant hearing loss in South Africa: Age of intervention and parental needs for support. Int J Audiol. 2008;47(Suppl 1):S30-35.
- McCarthy M, Munoz K, White KR. Teleintervention for infants and young children who are deaf or hard-of-hearing. Pediatrics. 2010;126:S52-S58.
- Porter A, Edirippulige S. Parents of deaf children seeking hearing loss-related information on the Internet: the Australian experience. J Deaf Stud Deaf Educ. 2007;12(4):518-29.
- Nogueira JF Jr, et al. Is the information available on the Web influencing the way parents see ENT surgical procedures? Braz J Otorhinolaryngol. 2009;75(4):517-23.
- Ferrari DV, Tomé T, Bastos BG. Internet based hearing aid orientation. Poster presented at: British Academy of Audiology Convention; 2008; Liverpool.
- Bastos BG. Tele-health: Evaluation of a Website as a Counseling Support Tool for Parents of Children Fitted with Hearing Aids [dissertation]. Faculdade de Odontologia de Bauru, Universidade de São Paulo, 2011. Available at: www.teses.usp.br/teses/disponiveis/25/25143/tde-23082011-145543/en.php
- Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa Nacional por Amostra de Domicilio. Available at: www.ibge.gov.br/home/estatistica/populacao/trabalhoerendimento/pnad2009/default.shtm
More on hearing healthcare and tele-audiology in Brazil:
- The Lancet special series titled Health in Brazil. Lancet, Volume 377, Issue 9779, May 2011.
- Bevilacqua MC, Novaes BC, Morata TC. Audiology in Brazil. Int J Audiol. 2008;47(2):45-50.
ALSO IN THIS SPECIAL ISSUE (OCTOBER 2012) ON TELEAUDIOLOGY:
- Extending Hearing Healthcare: Tele-audiology, by Jerry Northern, PhD
- The Need for Tele-audiometry, by De Wet Swanepoel, PhD
- Are You Ready for Remote Hearing Aid Programming? By Jason Galster, PhD, and Harvey Abrams, PhD
- Infant Diagnostic Evaluations Using Tele-audiology, by Deborah Hayes, PhD
- Online Global Education and Training, by Richard E. Gans, PhD
- Therapeutic Patient Education via Tele-audiology: Brazilian Experiences, Deborah Viviane Ferrari, PhD
- Telepractice in the Department of Veterans Affairs, by Kyle C. Dennis, PhD, Chad F. Gladden, AuD, and Colleen M. Noe, PhD
Citation for this article:
Ferrari D. Therapeutic Patient Education via Tele-audiology: Brazilian Experiences Hearing Review. 2012;19(10):40-43.