By Brian Taylor, AuD
Get your patients to start listening to their PALDs
|
A two-step protocol for assessing the communication needs of patients and understanding of speech in noise, and how to report this information to the patient relative to their potential need of a personal assistive listening device (PALD).
Over the past few years, several assistive listening devices designed to be used along with conventional hearing aids to improve the signal-to-noise ratio of challenging listening situations have been brought to market. These lower cost and easier-to-use devices have great promise for patients with significant degrees of SNR loss, who desire maximum speech understanding performance in noise. To date, these devices have not been universally embraced by professionals. This article is intended to introduce a simple two-step clinical selection process leading to an informed decision by the patient.
The SNR Loss Problem
A substantial number of hearing-impaired individuals have significant problems understanding speech in the presence of noise. In fact, this is the No. 1 complaint of the majority of hearing aid users.1
An inability to understand speech in noise, commonly referred to as “SNR loss” (signal-to-noise ratio loss), is a quantifiable condition that is often not detected with traditional pure-tone and speech audiometry.2 Fortunately, with proper test procedures, SNR loss can be measured and the appropriate treatment can be recommended. Oftentimes, these treatment recommendations include array microphones and other ALDs that work with existing hearing aids to maximize the SNR of the listening environment of the patient.
Although there is evidence supporting the fact that a patient’s ability to understand speech in quiet is unrelated to their ability to understand speech in noise,3 the majority of clinicians still only perform speech audiometry in quiet during the pre-fitting hearing aid selection process. A survey by Lindley4 showed that approximately 20% of clinical audiologists use speech-in-noise testing routinely during the pre-fitting assessment. According to the recent HR Dispenser Survey, only 2 in 5 (42%) owners of dispensing offices/practices report that their facilities use some form of speech-in-noise testing.5
Why ALDs are Still Important: Limitations of Directional Microphone Systems
There is considerable laboratory and real-world evidence suggesting that directional microphones of all types can effectively improve the signal-to-noise ratio of the listening environment of the patient.6 The amount of directional benefit obtained in everyday listening situations depends on many factors, including venting, microphone port alignment, and proper patient instruction.7
Although many studies conducted in contrived laboratory listening environments show that directional microphones significantly improve the SNR as measured with the Directivity Index (DI), real-world benefit remains limited for all types of directional microphones found on a traditional head-worn hearing aid.8 Ultimately, it is up to the dispensing professional to understand and appreciate the limitations of directional microphone systems, and match the technology that will maximize performance in noise with what the patient needs and is willing to accept.
In an attempt to address the limitations of both fixed and adaptive type directional microphones, several manufacturers have introduced personal assistive listening devices (PALDs) that are designed to work with existing hearing aids to improve the SNR of the listening situation. Only a few examples of these universal PALDs are listed in Figure 1 (an article by Yanz is also included in this edition of HR that shows an example of how Bluetooth technology is being employed in PALDs).
The literature suggests that every 1 dB SNR difference is equivalent to a 7-10 percentage point improvement in the speech intelligibility. Referred to as “close-talking microphones” by some, PALDs can improve the SNR by up to 20 dB, depending on the location of the microphone and the speaker’s mouth. When you compare this with the typical 2-4 dB SNR improvement that a directional system on a hearing instrument can provide, the value of these devices becomes fairly apparent—if not extremely impressive. In fact, ALDs (including PALDs, FM systems, induction loop, and IR systems) are by far the most effective technologies we have for increasing the SNR in patients.
An added feature of the PALDs listed in Figure 1 is they can be used with any existing hearing aid that has a good telecoil. Additionally, no boot needs to be coupled to the hearing aid, making the use of such devices more convenient for the end-user.
Although these lower cost PALDs work in combination with hearing aids, and have been shown to improve the SNR of the listening environment by upwards of 20 dB, they still remain underutilized. A recent field trial conducted in several clinics across the country found that the added cost, inconvenience of use, and unacceptable cosmetics contributed to poor use rates of them (unpublished study, Sonus field trial, June 2006). Indeed, many of the very reasons associated with other ALDs and related FM systems continue to plague their newer cousins.
Another possible reason these devices are underutilized is related to the fact that dispensing professionals lack the proper selection and counseling tools to dispense them. With the proper clinical tools, dispensing professionals can talk about the value of these types of devices in a more compelling manner. The following is a simple two-step selection process intended to help the dispensing professional make a more systematic recommendation of universal PALDs.
A Two-Step Selection Process
Step 1: Communications Needs Assessment. During the initial stage of the initial hearing aid evaluation process, a communication needs assessment is conducted by virtually all dispensing professionals. However, the majority of clinicians, according to one recent survey, fail to systematically record the needs assessment.
There are at least two important reasons the communication needs assessment should be recorded in a systematic fashion.
1) Specific goals for amplification can be targeted for improvement, and
2) During the initial adjustment period, improvement can be documented.
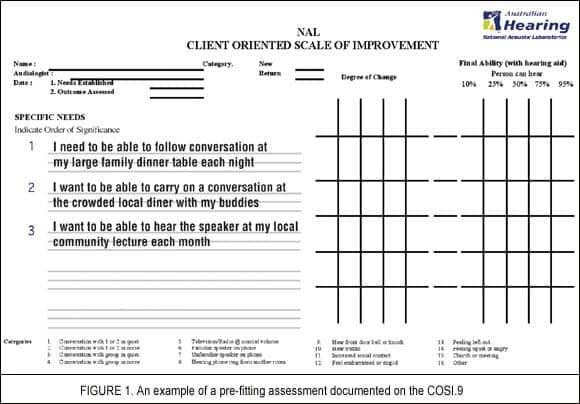
The Client Oriented Scale of Improvement (COSI)9, developed at the National Acoustic Laboratories (NAL) of Australia, is an excellent tool for nominating treatment goals and documenting improvement. The COSI allows the clinician to identify those listening situations that are most important to the patient, and assesses how much more clearly patients hear and rates how well they hear in those situations post-amplification. In this way, with the help of the patient, the clinician can assess if the aural rehabilitation program has been a success (or is completed to satisfaction). Another very useful component of the COSI is that—like several other NAL innovations—it is supported with an exceptionally large pool of normative data to compare your patients’ results against, making it an useful hearing aid benefit verification tool.
Due to the open-ended nature of the COSI, the dispensing professionals and the patient need to work together to devise a list of specific goals for improvement with amplification. Figure 2 is an example of what a pre-fitting communication needs assessment might look like for a patient with very demanding listening needs. In this particular example, the pre-fitting needs assessment has uncovered three challenging listening situations in need of improvement with amplification. Most dispensing professionals would agree that, if these are indeed the top three priorities for the patient, even the best digital hearing aid might fall short of expectations.
Step 2: Quantify SNR loss. The second step in the selection process is to quantify the patient’s SNR loss. As stated earlier in this article, most patients complain of an inability to understand conversations in noise. We know that this problem cannot be readily measured using traditional test battery procedures.
The QuickSIN10 is an excellent test to quantify this problem clinically. It provides a quick and easy tool to administer and score, and the results can be used to make specific treatment recommendations regarding any mode of amplification, including hearing aids, directional microphones, array microphones, FM systems. The results are also useful for counseling patients regarding realistic expectations and often reflect the problems that patients have in the real world.
Published reports suggest that about one-third of all patients have an SNR loss of greater than 7 dB.11 In these cases, first- and second-order directional microphones like those found in traditional hearing aids are likely to fall short of expectations. Although a significant degree of real-world benefit can still be readily obtained with traditional instruments for patients with moderate-to-severe SNR loss, it is the responsibility of the dispensing professional to educate the patient on the potential performance limitations of directional microphones and suggest supplemental devices. Similarly, tools like the QuickSIN can provide additional insight for that patient relative to what they can expect from amplification.
Aligning Expectations to Real World Performance
Using the results of both the COSI and QuickSIN allow the hearing care professional to guide the patient through the hearing aid selection process more effectively. For example, if a patient has a SNR loss of greater than 7 dB, and the COSI suggests that many of the listening situations are extremely challenging, then a universal PALD might be strongly recommended as a supplement to conventional hearing aids.
|
Another example of how the COSI and QuickSIN results compliment each other is when a patient has an SNR loss greater than 15 dB. Regardless of the COSI goals, a supplemental ALD would be recommended at the initial evaluation; in this case, it is apparent that no hearing aid—with or without an advanced directional microphone system—has enough directional capabilities to make up for the patient’s SNR loss.
Patient-Oriented Dispensing: The Power of the Informed Decision
Regardless of the hearing care professional’s experience with ALDs, it is their responsibility to advise each patient as to what would best solve his/her primary communication problems, particularly those objectives that the patient has set out to achieve through the purchase and use of the hearing instrument. Along with this recommendation would be a detailed description of the advantages and limitations of the proposed hearing devices.
Using a two-step selection process incorporating the COSI and QuickSIN allows patients to decide for themselves how they want to go about solving their communication problems.
When it comes to one of the most challenging and prevalent issues we face—the inability of so many patients to hear conversations in noise—many easy-to-use universal PALDs on the market today offer your patients an excellent range of choices. The role of the hearing care professional is to provide comprehensive services and steer patients through these choices in a meaningful way.
References
1. Kochkin S, Rogin C. Quantifying the Obvious: The Impact of Hearing Aids on Quality of Life. The Hearing Review. 2000;7(1):8-34.
2. Killion M, Niquette P. What can the pure-tone audiogram tell us about a patient’s SNR loss. Hear Jour. 2000;53(3):46-52.
3. Wilson R, McArdle R . Speech signals used to evaluate auditory function. J Rehab Res Dev. 2005;42(4):79-84.
4. Lindley G. Current hearing aid fitting protocols: results from an on-line survey. Audiol Today. 2006;18(3):13-20.
5. Strom KE. The HR 2006 dispenser survey. The Hearing Review. 2006;13(6): 16-39.
6. Walden B, Surr R, Cord M. Real-world performance of directional microphone hearing aids. Sem Hear. 2005;26,2,70-77.
7. Ricketts T. Directional hearing aids: then and now. J Rehab Research Dev. 2005; 42(4):133-144.
8. Bentler R, Tubbs J, Egge J, Flamme G, Dittberner A. Evaluation of an adaptive directional system in a DSP hearing aid. Am Jour Audiol. 2004;13,73-79.
9. Dillon H, James A, Ginnis J. Client Oriented Scale of Improvement (COSI) and its relationship to several other measures of benefit and satisfaction provided by hearing aids. J Amer Acad Audiol. 1997;8(1): 27-43.
10. Niquette P, Gudmundsen G, Killion M. QuickSIN Speech-in-Noise Test, Version 1.3. Available at: www.etymotic.com/pro quicksin.aspx. Elk Grove Village, Ill: Etymotic Research; 2001.
11. Killion M. New thinking on hearing in noise: a generalized articulation index. Sem Hear. 2002;23(1):57-75.
Correspondence can be addressed to HR or Brian Taylor, Amplifon USA, 5000 Cheshire Lane, Plymouth, MN 55446; e-mail: [email protected].






