Thanks to a new medical imaging device invented by University of Illinois researchers, doctors can now visualize areas behind the eardrum to better diagnose and treat chronic ear infection.
The researchers, led by University of Illinois electrical and computer engineering professor Stephen Boppart, published their findings in Proceedings of the National Academy of Sciences.
Studies have found that patients who suffer from chronic ear infections may have a film of bacteria or other microorganisms that builds up behind the eardrum, very similar to dental plaque on unbrushed teeth. Finding and monitoring these so-called biofilms are important for successfully identifying and treating chronic ear infections.
“We know that antibiotics don’t always work well if you have a biofilm, because the bacteria protect themselves and become resistant,” Boppart said. “In the presence of a chronic ear infection that has a biofilm, the bacteria may not respond to the usual antibiotics, and you need to stop them. But without being able to detect the biofilm, we have no idea whether it’s responding to treatment.”
However, middle-ear biofilms are difficult to diagnose. A doctor looking through a standard otoscope sees only the eardrum’s surface, not the bacteria-seeded biofilm that may develop into an infection. Invasive tests can provide evidence of a biofilm, but are unpleasant for the patient and cannot be used routinely.
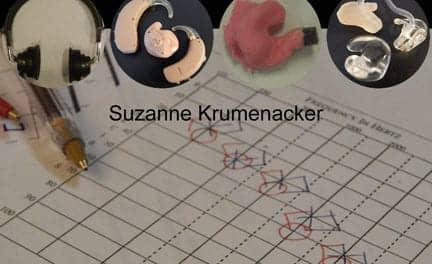
The new device (pictured) is an application of a technique called optical coherence tomography (OCT), a non-invasive imaging system devised by Boppart’s group. It uses beams of light to collect high-resolution, 3-D tissue images, scanning through the eardrum to the biofilm behind it. The concept is similar to ultrasound imaging, but uses light instead of sound.
“We send the light into the ear canal, and it scatters and reflects from the tympanic membrane and the biofilm behind it,” said graduate student Cac Nguyen, the lead author of the paper. “We measure the reflection, and with the reference light, we can get the structure in depth.”
The single scan is performed in a fraction of a second, which is helpful for treating squirming children. The scan will image a few millimeters deep behind the eardrum, allowing doctors to see not only the presence of a biofilm, but also how thick it is and its position against the eardrum.
The paper marks the first demonstration of using the ear OCT device to detect biofilms in human patients. To test their device, the researchers worked with clinicians at Carle Foundation Hospital in Urbana, Ill, to scan patients with diagnosed chronic ear infections, as well as patients with normal ears. The device identified biofilms in all patients with chronic infections, while none of the normal ears showed evidence of biofilms.
“I think this is now a technology that allows physicians to monitor chronic ear infection, and examine better ways to treat the disease,” said Boppart, who is also affiliated with the departments of bioengineering and internal medicine, the Institute for Genomic Biology, and the Beckman Institute for Advanced Science and Technology at the university. “We can use different antibiotics and see how the biofilm responds.”
Next, the researchers plan to investigate different ear pathology, particularly comparing acute and chronic infections, and will examine the relationship between biofilms and hearing loss. They hope that improved diagnostics will lead to better treatment and referral practices.
The device is currently a hand-held prototype. The researchers hope to further develop it to be more compact, easy to use, and low-cost. Welch Allyn is a collaborator on the project, which was funded by the National Institutes of Health.
The paper, “Non-invasive in vivo optical detection of biofilm in the human middle ear,” is available online.
SOURCE: University of Illinois