Fitting Tips | November 2013 Hearing Review
Foreword. Audioscan recently ran a “The Best Fit Challenge” contest that asked HR readers, “Tell us what you do to get the best fit.” Many excellent articles and tips were submitted, and these were reviewed by contest panelists Gus Mueller, PhD, of Vanderbilt University; Catherine Palmer, PhD, of the University of Pittsburgh; Wayne Staab, PhD, HR editorial advisory board member and editor at HearingHealthMatters.org; Karl Strom, editor in chief of The Hearing Review; and Rebecca Younk, AuD, director of professional development at Amplifon USA. The following article by Leavitt and Knowles is the 1st place winner. Audioscan and HR thank everyone who submitted the many outstanding articles and tips. See the end of this article for more details on the contest.
A Time-efficient Method and Form for Documenting
Hearing Aid Benefit
An evidence-based approach to reporting hearing aid performance
By Ron J. Leavitt, AuD, and Liza R. Knowles, MS, CRC
A form that offers a shorthand system for illuminating hearing aid benefit, counseling needs, and suspected central auditory problems.
The profession of audiology, and hearing healthcare in general, appears to be moving toward a consensus on a number of hearing aid-related issues including:
1) The value of real-ear aided measurement;
2) The value of real-ear verified speech-cue audibility;
3) The value of speech testing in noise; and
4) The value of scientifically validated hearing aid user surveys.
It is our contention that a standardized, time-efficient, single-page form that documents real-ear aided performance, real-ear verified speech cue audibility, speech in noise test results, and user self-report might facilitate this movement toward universal acceptance and use of these measures. Such a form may accomplish several goals:
Standardization. The form provides a standardized method of reporting objective and subjective measures of hearing aid performance/benefit across clinics.
Clear information for all users. By reading the form, physicians, allied health professionals, vocational rehabilitation (VR) counselors, and other third-party payors are able to quickly identify the extent to which hearing aids are benefiting their patients/clients.
Demonstration of value for professional services. The work necessary to achieve scientifically validated hearing aid fittings is demonstrated by the form. It makes clear to third-party payors and to potential hearing aid users what they are getting for their money.
Support and reinforcement of best practices. The form identifies those audiologists who are applying “Best Practices” as detailed by the American Academy of Audiology Task Forces on Adult and Pediatric Amplification.1 This information is at http://www.audiology.org/resources/documentlibrary/Documents/haguidelines.pdf for adults and for pediatric hearing aid fittings at http://www.audiology.org/resources/documentlibrary/Documents/PediatricAmplificationGuidelines.pdf.
Demonstration of user benefit in noise. In the case of successful fittings, there is clear information on this form for all concerned parties that the hearing aid wearer is functioning better with the hearing aids in noisy places than without them. It has been our experience that such a demonstration not only improves outcomes, but stops the user from reporting that he/she removes the hearing aid in noisy places as it provides no benefit.
Addresses CAPD. Some light can be shed by this form on possible central auditory processing problems that exist in conjunction with peripheral hearing loss as noted by Humes et al. 2
Identification of inaccurate patient perceptions. This form identifies those patients/clients whose perception of their hearing problem is inaccurate. For such patients/clients, Saunders and Forsline3 and Saunders4 have developed a counseling program that may facilitate hearing aid acceptance.
To achieve the goals listed above, the first author has completed the form shown in Figure 1 on all VR clients referred by the second author to our clinic in the past 14 months. We also have shared this form with other VR counselors around the state, as well as audiologists at the local Veterans Administration (VA) Hospital. Subsequently, both that VA hospital and the local VR office have formally requested much of this information be provided for all patients/clients seen at our clinic.
|
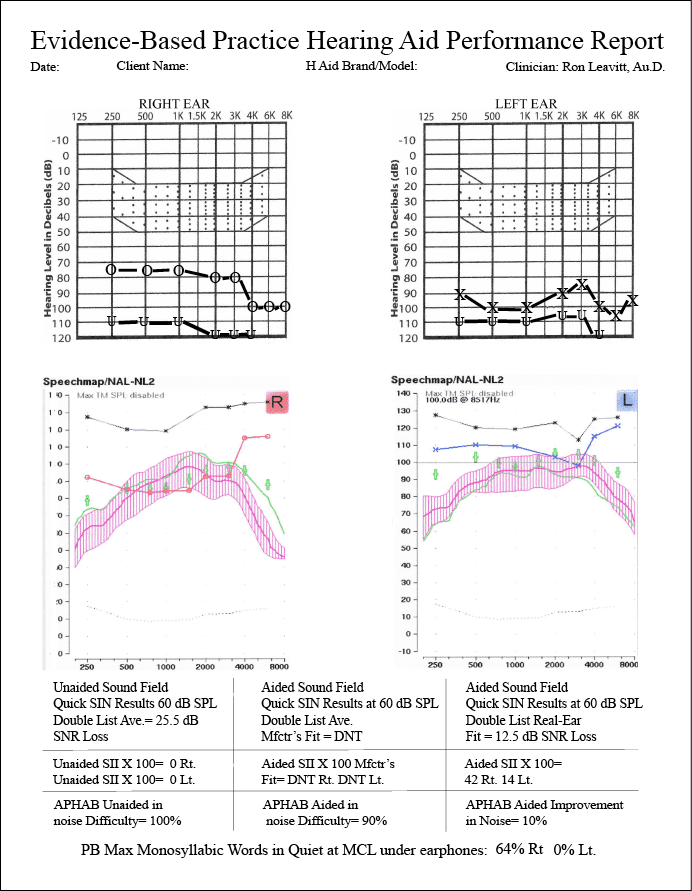
| Figure 1. The form currently used by the authors in their practice to document hearing aid benefit. |
To make this form time efficient, several decisions were made that warrant discussion:
1) The audiogram templates used are based upon the “Count-the-Dots” audiogram of Killion and Mueller.5 We feel this graphic overlay facilitates discussion of the importance of speech cue audibility with our patients/clients and their families. We recognize other clinics may prefer alternate audiogram graphics. For example, audiogram overlays showing the speech sounds positioned on the audiogram are also instructive. However, since the “Count-the-Dots” audiogram is available in the Noah 4 software, it is accessible to most audiologists.
2) The real-ear aided response graphics we use are those obtained from Audioscan Verifit and Axiom systems. We recognize there are other real-ear systems that provide real-ear aided response data. However, we have not found another real-ear system that computes the unaided and aided Speech Intelligibility Index (SII) per ANSI S3.5-1997, R 2007.6 Further, the real-ear-aided-response (REAR) data from the Audioscan systems allow a pictorial representation of the effects of hearing aid compression on the amplified speech signal not present on other real-ear systems used in our clinic. For those wishing to compute SII without the Audioscan system, the website www.sii.to allows SII computation at no charge.
3) We recognize that the SII data for children with hearing loss are not equivalent to the data for adults as noted by the work of Scollie (2008). Those audiologists fitting hearing aids on children should recognize the SII values reported for adults overestimate the predicted speech intelligibility in children with hearing loss.
4) We report the SII value multiplied by 100 and discuss the patient’s hearing loss in terms of percent of speech cues made inaudible by the hearing loss. We find the SII expressed in a percent value more meaningful to patients and their families than the more conventional hearing loss classification designators (mild, moderate, moderately severe, severe and profound), which lack scientific validation.7-10 It also has been shown that these hearing loss classification designators are poorly understood by patients/parents11 and allied professionals12 and suffer from a number of technical errors.10
Further, research suggests the SII correlates better with a child’s lexical abilities than the pure-tone average from which the hearing loss classification designators are derived.13,14 The SII is also useful when selecting appropriate amplification for people with hearing loss.15-17
5) Choosing a 60 dB SPL output for soundfield Quick Speech-in-Noise (QuickSIN) testing is a somewhat arbitrary decision as we recognize this level is at times higher than speech arriving at the ear of the hearing aid user and in other instances lower.18 With the publication of Dr Gifford’s book on cochlear implant evaluation, candidacy, and outcomes,19 we expect this 60 dB SPL soundfield presentation level will become more widespread as will the specific calibration methods noted in this publication.
According to data from McArdle and Wilson,20 only lists 1, 2, 6, 8, 10, 11, 12, 15, and 17 of the Quick SIN should be used. For children, the BKB-SIN test should be substituted for the Q-SIN. Ng et al21 reported successfully using their adapted BKB-SIN on children as young as 5 years of age. However, the authors noted the traditional BKB-SIN norms did not apply and the data should be used only on a case-by-case basis until validated norms become available.
6) We continue to collect data on the performance differences between manufacturer’s best-fit and real-ear aided data in terms of both Q-SIN scores and aided SII values. However, when pressed for time, we omit the manufacturer’s best-fit information on this form as research has shown manufacturer’s best-fit algorithms generally provide lower aided SII values.22-30
7) We recognize numerous speech-in-noise (SIN) tests exist, and several are validated in the literature. We have no financial interest in the QuickSIN Test but find it time-efficient, and as Grant and Walden31 noted, the QuickSIN has some (but not perfect) predictive ability in “identifying a patient’s suprathreshold deficit and its impact on understanding speech-in-noise.” Further, as McCardle and Wilson20 noted, the QuickSIN (and other speech-in-noise tests) “can be useful for selecting amplification strategies…and counseling patients on realistic expectations for hearing-aid performance.” In addition, as Humes and colleagues have pointed out, SIN tests should be used as they may reveal the combined effects of peripheral, brainstem, and central auditory problems2 and suggest the need for aural rehabilitation.32
In our clinic, when an adult hearing aid user’s 2-list averaged QuickSIN scores are 10.5 dB or worse, we recommend hearing aids with remote microphone capabilities as data from Olsen18 show that many listening environments have a 10 dB signal-to-noise ratio (SNR) or worse. For school-aged children, this criterion should be set even lower according to data from several studies33-36 showing classroom SNRs of -6 to -3 dB.
8) We omitted the aversive (AV), reverberation (RV), and ease-of-communication (EC) data from the Abbreviated Profile of Hearing Aid Benefit (APHAB).37 We believe the unaided vs aided background-noise data will suffice as studies continue to show that word recognition in noise is a major concern of people with hearing loss.20,38
While we recognize there are numerous other user-based surveys available, we continue to use the APHAB in part due to its near universal accessibility to clinicians using Noah software. Further, we have found the unaided APHAB gives valuable information about the individual’s perception of hearing difficulty. For example, a person who scores a 25.5 dB SNR loss on the unaided soundfield QuickSIN at 60 dB SPL presentation level, while reporting virtually no unaided listening difficulty in noise on the APHAB, presents a noteworthy counseling challenge to the clinician.
9) We do not expect that the high aided SII values obtained from an NAL NL-1/2 or DSL I/O fitting will consistently result in high aided performance ratings on the APHAB, nor will the hearing aid user consistently report they are satisfied with the hearing aids. As Cox, Alexander, and Gray39 have noted, some hearing aid users may “continue to experience unpleasant emotions, even with effective hearing aid treatments, because (for some individuals) their psychological discomfort is dispositional as well as situational.”
We also do not expect that QuickSIN scores showing excellent aided function in noise will necessarily produce high satisfaction scores on the aided APHAB. As Cox, Alexander, and Xu40 have noted, “There are no existing questionnaires that are known to be primarily device-oriented and relatively free of personality influence.” While we recognize that Cox and co-workers are developing a Device Oriented Subjective Outcome (DOSO) Scale for hearing aid performance that appears relatively free of confounding personality variables, we find the user’s perception of unaided and aided difficulty as measured by the APHAB to be valuable as noted above.
Summary
The one-page, time-efficient form shown in Figure 1 has been administered in our clinic for the past 14 months to all of our VR and VA clients. This form will continue to evolve as published research highlights new areas of relevant data. In the interim, this form has provided important information in several areas including the following:
• Comparison of aided performance in noise and aided SII values with manufacturers’ best-fit algorithms as compared with NAL NL-1 and currently NAL NL-2 hearing aid fittings.
• Perspective on the individual’s perception of unaided and aided hearing difficulty in a variety of quiet, reverberant, and noisy environments compared to the individual’s unaided SII and QuickSIN/BKB-SIN data presented at a typical conversational loudness in soundfield.
• Suggestion of central auditory problems existing in concert with peripheral hearing loss when QuickSIN scores remain poor even when high monosyllabic word scores in quiet and high aided SII scores are obtained.
• Objective evidence supporting the need for a remote microphone when the SNR loss as measured by the Q-SIN is poorer than 10.5 dB for adults and 5.5 dB SNR loss on the BKB-SIN for school-aged children and college students.
• Insight into which hearing aid manufacturers can provide the greatest amount of stable gain in the high frequencies without feedback. We have found these differences quite striking among the “Big 6” hearing aid manufacturers.
• The extent to which high frequency aided audibility at and above 4000 Hz contributes to improved performance on the QuickSIN and BKB-SIN. The interested reader is referred to the work of Stelmachowicz et al41 for a more in-depth discussion of this issue.
We offer this form in its current form to the audiologists, VR counselors, and other hearing care professionals who need a time-efficient method for obtaining results that conform to many of the “Best Amplification Fitting Practices” for children and adults as outlined by the American Academy of Audiology. We have found this form to be a convenient shorthand system for illuminating hearing aid benefit, counseling needs, and suspected central auditory problems.
This form also helps objectively identify those clients/patients who will require a remote microphone and other types of assistance such as a cochlear implant, real-time remote captioning, or other auditory-visual enhancement technology to be functional in the workplace and in family and social environments.
Some comments on this article from the panelists…“When I read this submission, I wanted to immediately implement it in every Amplifon clinical protocol. I believe it will assist both patients and other healthcare providers [to] understand the impact of hearing loss and benefit from hearing instruments.” Verification and validation of hearing aid fittings (required and/or self-imposed) can be expected to hold center stage moving forward in management of the hearing-impaired patient. This will become a significant requirement of third-party payers to ensure that what is being fitted and paid for is performing to some acceptable level. But this expectation should be no less even when third party payment is not involved. The goal is not new, but for a number of reasons, it seems not to have been implemented widely. A variety of verification methods have been developed and are used by clinicians to satisfy specific fitting goals, but a comprehensive, straight-forward program that integrates existing equipment and tests (both objective and subjective) seems to have eluded professionals as a follow-up in the hearing aid fitting process. Additionally, sharing this information with referral facilities, family, colleagues, and for record keeping allows a facility to position itself to achieve maximum efficiency and recognition among cooperating personnel and facilities. An easily-to-understand report that visually summarizes the hearing aid fitting process—not only for the dispenser involved, but for other interested parties (referral and/or family)—is suggested with this article. It is not unique in the measurements made, nor in the interpretation of results, but in the method to meaningfully integrate them, that makes this suggested improvement worthy of consideration. —Wayne Staab, PhD, HR editorial board advisor and editor at HearingHealthMatters.com “With the many issues confronting our industry, proving hearing aid performance and demonstrating the value of professional services has never been more important. Forms that document proven methods and demonstrate an adherence to those protocols shown to increase benefit and customer satisfaction with hearing aids are an excellent step in the process. —Karl E. Strom, editor-in-chief, The Hearing Review A comment from Audioscan “The selected submission shows that you can distill decades of research into a very practical protocol with a single page as the output. We are excited and proud that we could be the catalyst that brought this information to the wider hearing health community. Congratulations, and enjoy your new Axiom fitting system Dr. Leavitt.” |
Acknowledgements
Congratulations to Dr Ron Leavitt and Liza Knowles who submitted this winning entry in the Best Fit Challenge™, a contest run by Audioscan to tap into the collective knowledge of America’s hearing care professionals for the betterment of patient care across the country. This submission was selected by a panel of five industry experts, and the authors will receive a free Audioscan Axiom® hearing instrument fitting system for their practice. Expert panel members included: Gus Mueller, PhD, Vanderbilt University; Catherine Palmer, PhD, University of Pittsburgh; Rebecca Younk, AuD, Amplifon USA; Wayne Staab, PhD, HearingHealthMatters.com; and Karl Strom, The Hearing Review.
References
1. American Academy of Audiology. Pediatric Amplification Protocol. June 2012. Available at: www.audiology.org
2. Humes LE, Dubno JR, Gordon-Salant S, Lister JJ, Cacace AT, Cruickshanks KJ, Gates GA, Wilson RH , Wingfield A. Central presbycusis: a review and evaluation of the evidence. J Am Acad Audiol. 2012; 23(8):635-66.
3. Saunders GH, Forsline A. The Performance-Perceptual Test (PPT) and its application to hearing aid counseling. Hearing Review. 2006;13(13):18-25.
4. Saunders GH. The Performance Perceptual Test (PPT): Clinical applications. AudiologyOnline 2009, Article 889. Available at:www.audiologyonline.com/articles/performance-perceptual-test-ppt-clinical-899
5. Killion MC, Mueller HG. Twenty years later: a new count-the-dots method. Hear Jour. 2010;63(1):10-17.
6. American National Standards Institute (ANSI). American National Standard Methods for Calculation of Speech Intelligibility Index (1997 R2012). Available at: www.webstore.ansi.org
7. Goodman AC. Reference zero levels for pure-tone audiometers. Asha. 1965;7:262–263.
8. Kryter KD. Evaluation of hearing handicap. J Am Acad Audiol. 1998;9:141-146.
9. Blair J, EuDaly M, Benson P. The effectiveness of audiologists’ information sources for classroom teachers. Lang Speech Hear Services in Schools.1999;30:173-182
10. Leavitt RJ, Vossler-Welch CB. An alternative to traditional hearing loss classification systems. Poster Session at the American Academy of Audiology Convention AudiologyNOW!, April 2012, Boston, Mass.
11. Haggard R, Primus M. Parental perceptions of hearing loss classification in children. Am Jour Audiol. 1999;8:83-92.
12. Aguila-Vinson M, Lister J, Hnath-Chisolm T, Blake-Rahter P. Perception of hearing loss by graduate students of speech-language pathology. Contemp Issues Commun Science and Disorders. 2004;31:205-214
13. Gilbertson M, Kamhi AG. Novel word learning in children with hearing impairment. J Sp Hear Res. 1995;38:630-642.
14. Stiles DJ, Bentler RA, McGregor KK. The speech intelligibility index and the pure-tone average as predictors of lexical ability in children fit with hearing aids. J Speech Lang Hear Res. 2012;55(June):764-778.
15. Pavlovic CV. Speech spectrum considerations and speech intelligibility predictions in hearing aid evaluations. J Speech Hear Disorders. 1989;54:3-8.
16. Magnusson L, Karlsson M, Leijon A. Predicted and measured speech recognition performance in noise with linear amplification. Ear Hear. 2001;22:46–57.
17. Amlani AM, Punch JL, Ching TYC. Methods and applications of the audibility index in hearing aid selection and fitting. Trends Amplif. 2002;6:81–129
18. Olsen WO. Average speech levels and spectra in various speaking/listening conditions: a summary of the Pearson, Bennett, & Fidell (1977) report. Am J Audiol. 1998;7(2):21-25.
19. Gifford RH. Cochlear Implant Assessment: Evaluation of Candidacy, Performance and Outcomes. San Diego: Plural Publishing;2013.
20. McArdle RA, Wilson RH. Homogeneity of the 18 QuickSIN™ Lists. J Am Acad Audiol. 2006;17(3):157-167.
21. Ng SL, Meston CN, Scollie SD, Seewald RC. Adaptation of the BKB-SIN test for use as a pediatric aided outcome measure. J Am Acad Audiol. 2011;22(6):375-86.
22. Hawkins DB, Cook JA. Hearing aid software predictive gain values: how accurate are they? Hear Jour. 2003;56:26–34.
23. Bentler R. Advanced hearing aid features: Do they work? Paper presented at the 2004 convention of the American Speech-Language-Hearing Association, November 18-20, 2004, Philadelphia, Pa.
24. Aarts NL, Caffee CS. Manufacturer predicted and measured REAR values in adult hearing aid fitting: accuracy and clinical usefulness. Int J Audiol. 2005;44(5):293-301.
25. Aarts NL, Caffee CS. The accuracy and clinical usefulness of manufacturer-predicted REAR values in adult hearing aid fittings. Hearing Review. 2005;12(12):16-22.
26. Bretz K. A comparison of three hearing aid manufacturers’ recommended first fit to two generic prescriptive targets with the pediatric population. Paper 189. Independent Studies and Capstones. St. Louis: Program in Audiology and Communication Sciences, Washington University School of Medicine, 2006; Available at: http://digitalcommons.wustl.edu/pacs_capstones/189
27. Aazh H, Moore BC. The value of routine real ear measurement of the gain of digital hearing aids. J Am Acad Audiol. 2007;18:653-64.
28. Seewald, R., Mills, J., Bagatto, M., Scollie, S., & Moodie, S. A comparison of manufacturer-specific prescriptive procedures for infants. Hear Jour. 2008; 61(11):26-34.
29. Leavitt RJ, Flexer C. The importance of audibility in successful amplification of hearing loss. Hearing Review. 2012;19(13):20-23. Available at: /continuing-education/21305-the-importance-of-audibility-in-successful-amplification-of-hearing-loss
30. Abrams HB, Chisolm TH, McManus M, McArdle R. Initial fit approach versus verified prescription- comparing self-perceived hearing aid benefit. J Am Acad Audiol. 2012;23:768-778.
31. Grant KW, Walden TC. Understanding Excessive SNR Loss in Hearing Impaired Listeners. J Am Acad Audiol. 2013;24(4):258-273.
32. Gates GA. Central presbycusis: An emerging view. Otolaryngol Head Neck Surg. 2012;147(1):12
33. Blair JC. Effects of amplification, speechreading, and classroom environments on reception of speech. Volta Rev. 1977;79:443-449 .
34. Finitzo-Hieber T. Classroom acoustics. In: Roeser RJ, Downs MP, eds, Auditory Disorders in School Children. New York: Thieme-Stratton Inc;1981:250-262 .
35. Markides A. Speech levels and speech-to-noise ratios . Br J Audiol. 1986;20:115-120 .
36. Crandell CC. Speech recognition in noise by children with minimal degrees of sensorineural hearing loss. Ear Hear. 1993;14:210-216 .
37. Cox RM. Cox RM, Alexander GC. The abbreviated profile of hearing aid benefit. Ear Hear. 1995;16:176-86.
38. Kochkin S. MarkeTrak VIII: Consumer satisfaction with hearing aids is slowly increasing. Hear Jour. 2019;63(1):19-32.
39. Cox RM, Alexander GC, Gray GA. Who wants a hearing aid? Personality profiles of hearing aid seekers. Ear Hear. 2005; Feb;26(1):12-26.
40. Cox R, Alexander G, Xu J. Development of the Device Oriented Subjective Outcome Scale (DOSO). Poster session presented at the 2009 Annual Meeting of the American Auditory Society, Scottsdale, Ariz; March 2009.
41. Stelmachowicz PG, Pittman AL, Hoover BM, Lewis DE, Moeller MP. The importance of high-frequency audibility in the speech and language development of children with hearing loss. Arch Otolaryngol Head Neck Surg. 2004;130(5):556-62.
CORRESPONDENCE can be addressed to Dr Leavitt at: [email protected]





