Summary:
A scalable cochlear implant (CI) program in South Carolina has demonstrated how strategic workflow design, data-driven efficiency measures, and team-based care can dramatically expand access, improve patient satisfaction, and sustain rapid program growth in an underserved region.
Key Takeaways:
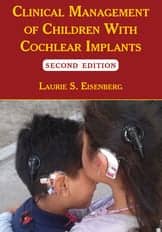
- Efficiency-Driven Growth: Through workflow optimization and staffing expansion, annual implant volume increased from 38 in 2022 to 142 in 2024, improving access across adult and pediatric populations.
- Innovative Care Model: Key initiatives—including a Patient Care Navigator role, CI-specific tracking within Epic, streamlined follow-up protocols, and group counseling sessions—reduced administrative burden and enhanced patient throughput.
- Sustainable Scalability: Collaborative care partnerships and ongoing quality improvement efforts have extended CI access to remote communities, establishing a replicable framework for scalable, high-quality implant programs nationwide.
By Heather Strader, AuD, and Brent Wilkerson, MD
Introduction
Despite compelling evidence supporting the benefits of cochlear implantation, CI utilization remains strikingly low with fewer than 10% of eligible adults in the U.S. receiving cochlear implants.1 This underutilization stems from a combination of systemic barriers, including low referral rates, geographic limitations, and inefficiencies in care delivery.2 In 2021, our team launched a new CI program in South Carolina, targeting a region previously underserved in implant services. From inception, our program’s priorities were scalability, patient-centered care, and high clinical efficiency. Based on principles gained from participation in the Institute for Cochlear Implant Training (ICIT) Team Efficiency Course, we established and applied a set of workflow strategies that are continually refined through ongoing quality improvements.
Program Structure and Development
Our objective was to create a flexible, scalable CI program capable of meeting rising demand without compromising quality of care. Early development involved evaluating clinical capacity, completing time studies, building and expansion of referral networks, and training staff to develop a streamlined CI pathway. Our team committed to a culture of continuous quality improvement, with data driving refinements at each stage. Below, we outline our program growth and six key initiatives that have substantially refined our workflow.
In our first year, 2022, we performed 38 implants with 0.4 FTE CI-specific audiology support and one neurotologist. By 2023, surgical volume rose to 112 implants, driven primarily by expanded audiology support (1.0 FTE) and growth in neurotology practice; a pediatric otolaryngologist joined mid-year, contributing to long-term program development and overall volume. In 2024, with 1.5 FTE audiology support and two CI surgeons—one neurotologist performing both adult and pediatric implants and one pediatric otolaryngologist performing pediatric implants—the program implanted 142 ears (Figure 1, Table 1).
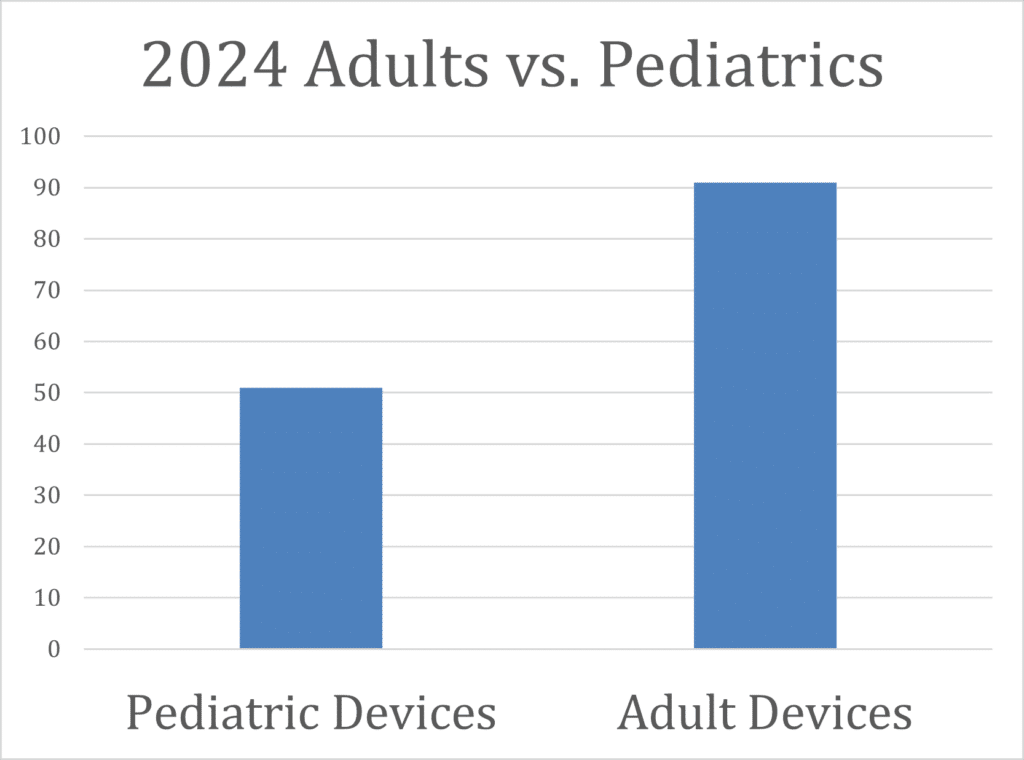
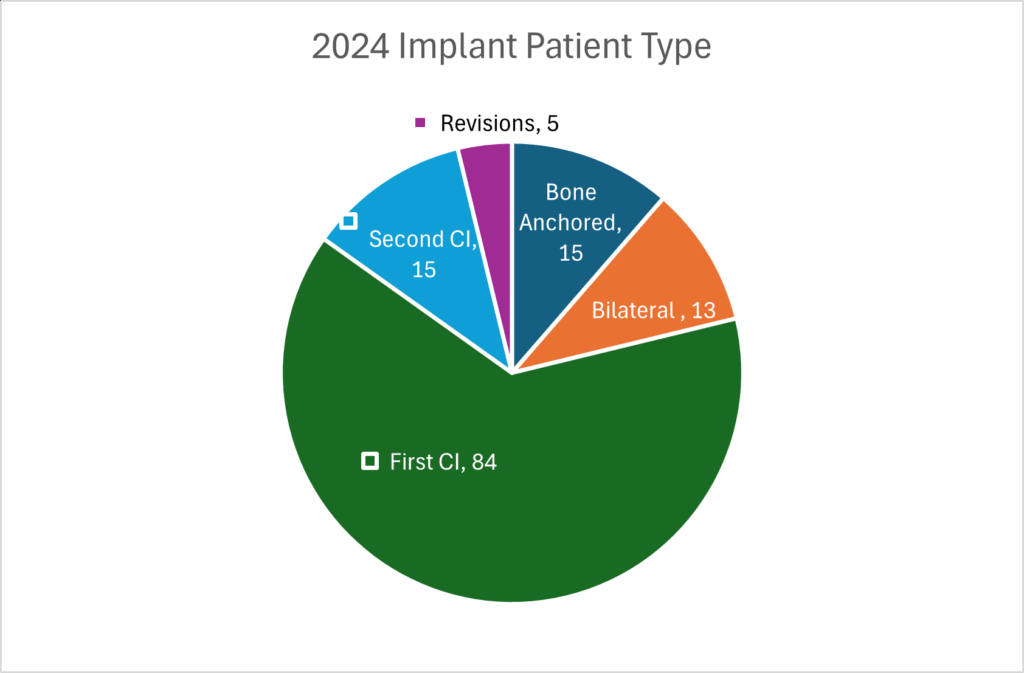
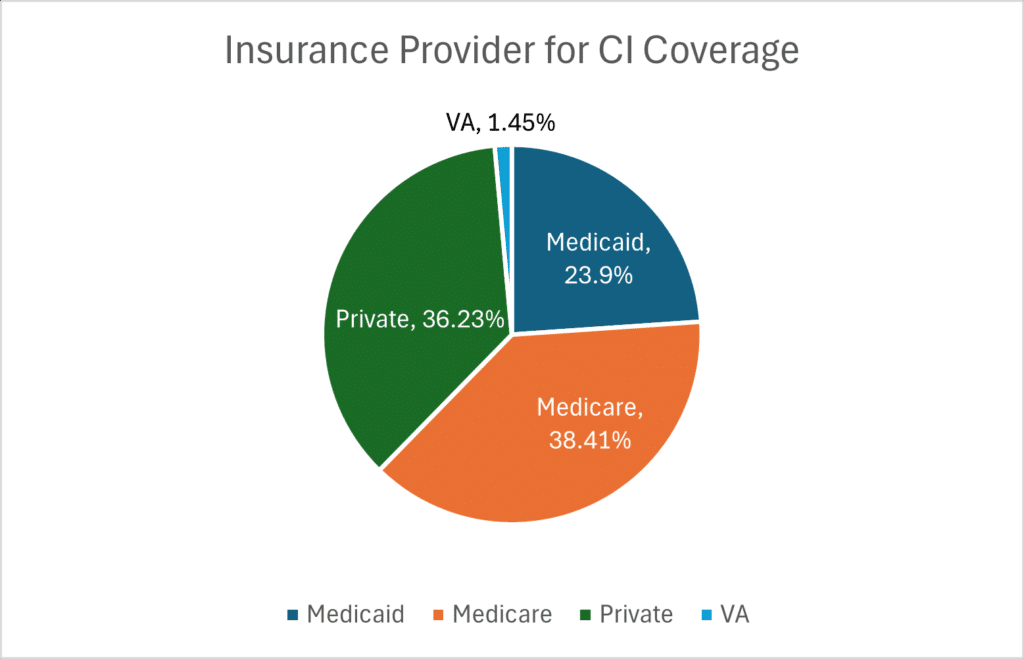
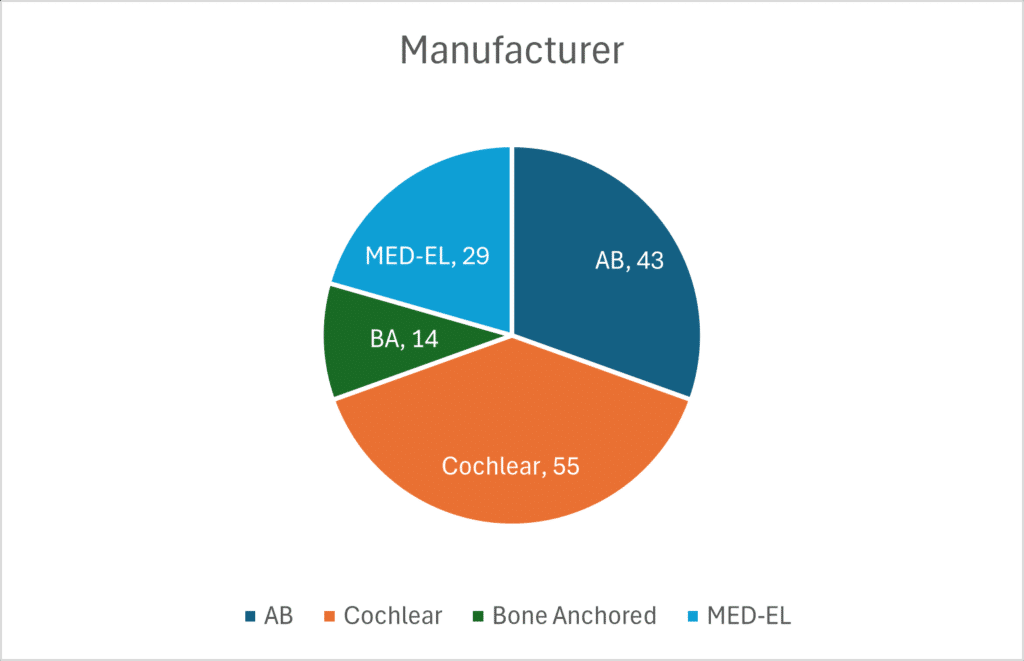
A further breakdown of our 2024 data shows we performed implants on 91 adult and 51 pediatric ears, showing growing access and demand across the lifespan (Figure 2). This accounts for 84 first ears, 15 second ears, 13 bilateral implants, 15 bone-anchored devices, and 5 revisions (Figure 3). Device selection included 55 implants with Cochlear, 43 with Advanced Bionics, and 29 with Med-El (Figure 4). The distribution highlights balanced access to all major manufacturers, supporting patient-centered choice in CI technology. Payer mix included 36% private insurance, 23% Medicaid, 38% Medicare, and 1% Veterans Affairs (Figure 5). The growth and success of our program is largely attributed to the efficiency initiatives described below.
Initiative 1: Patient Care Navigator Role
Time studies and patient feedback revealed that administrative tasks—such as triaging clinical inquiries, completing forms, managing software issues, and retrieving mapping files—were a major bottleneck. Early on, a CI coordinator focused primarily on surgery scheduling, with limited time to assist clinical operations.
We created a Patient Care Navigator (PCN) role modeled after a nurse navigator framework. The PCN coordinates scheduling, manages communications, and handles documentation across the CI pathway. Crucially, this clinical position requires familiarity with electronic health record (EHR) systems, interdisciplinary scheduling, and workflow systems. The role has significantly increased provider capacity by reducing time spent on non-clinical tasks and improving responsiveness to patients and referral sources.
Prior to implementation, CI audiologists were spending 43% of their time performing non-billable tasks. Six months after implementing this position, the time spent on nonbillable tasks was reduced to 27%. Additionally, referral-to-surgery intervals shortened by approximately 10%. The audiologists’ and PCN’s workloads are continually monitored for optimization.
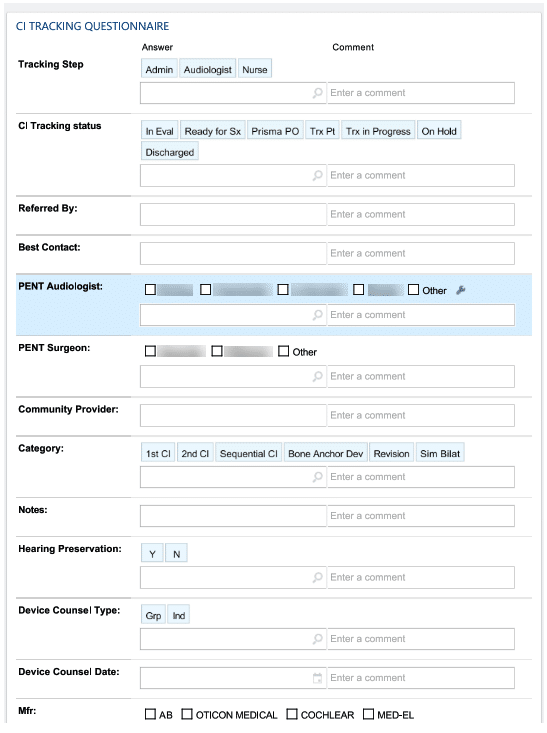
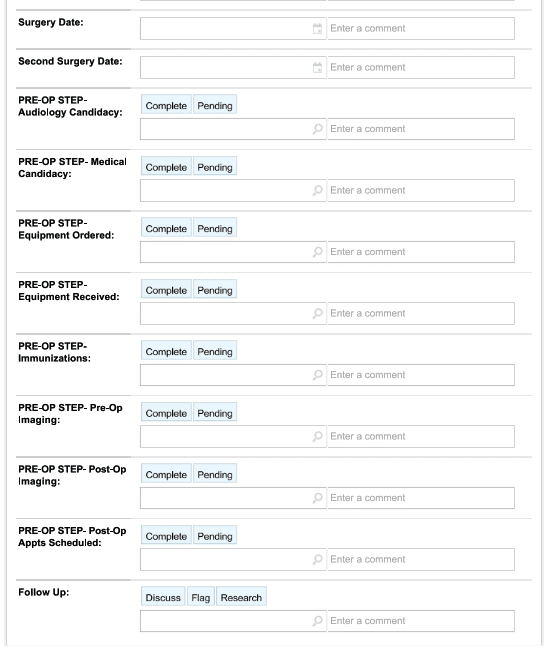
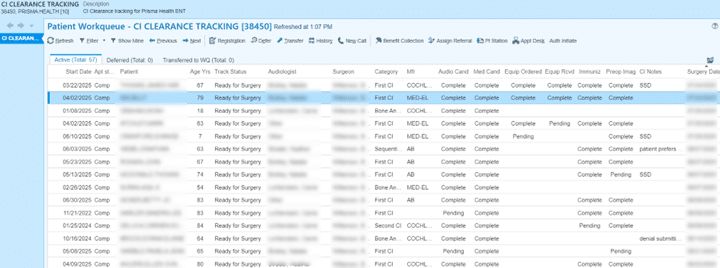
Initiative 2: Patient Tracking System
In collaboration with our internal Epic Optimization Team, we adapted our EHR to support CI-specific care pathways. A standardized questionnaire was embedded within each CI referral, capturing essential preoperative data. A work queue system displays data with status tracking for each patient. The PCN inputs data, monitors the queue, and flags delays or issues for resolution. This system has improved scheduling timelines and allows for data-driven decision-making. Continued refinement is planned to better track outcomes and support metrics-based program evaluation (Figure 6 and Figure 7).
Table 1
| Total Implants | Audiology FTE | Surgeons | |
| 2022 Total | 38 | 0.5 | 1 |
| 2023 Total | 112 | 1.0 | 1.3 |
| 2024 Total | 142 | 1.5 | 2 |
Table 1. Growth in total implants from 2022 to 2024 aligns with strategic increases in Audiology FTEs and surgical capacity. As audiology staffing tripled and surgical support nearly doubled, implant volume increased nearly four-fold—highlighting the direct impact of resource investment on patient care access.
Initiative 3: Streamlined Follow-Up Scheduling
Traditionally, CI protocols involved up to seven follow-up visits within the first post-implant year.3 We reduced this to four routine visits for adults, aligning with MSTB-3 guidelines.4 Additionally, we follow the recommendations of Holder et al.5,6 and incorporate standardized ESRT at the one-month follow-up visit, which allows for more efficient optimization of programming. These changes have eliminated up to 273 appointments annually based on our 2024 volume, increasing our capacity for spending time with new and complex patients. Future efforts include integration of remote monitoring and programming visits and expanded PCN troubleshooting to triage visits more effectively.
Initiative 4: Group Device Counseling Sessions
To further improve efficiency and education, we launched monthly group device counseling sessions. At the end of their CI evaluation, all adult candidates receive educational materials and are given the option to contact representatives for all three device manufacturers. Patients then attend a group session (up to six patients plus support persons), which consists of a 60-minute audiologist-led presentation describing devices, followed by hands-on demonstrations and time for individual questions.
Held in an accessible space with real-time captioning, these sessions are supported by the PCN, who assists with answering questions and completing order forms. Patients select their device and accessories during the appointment and are instructed on how to set up their app prior to initial activation. This model saves approximately 450 appointment minutes per month and promotes peer interaction and learning. While not suitable for pediatric or complex cases, we plan to pilot a modified version for children with support from our newly hired auditory verbal therapist (AVT) in the coming year.
Initiative 5: Strengthening Manufacturer Partnerships
From evaluation through post-op follow-up, patients receive targeted information and support from device manufacturers. Roles and expectations are clearly communicated, both verbally and in writing throughout the patient experience. Pre-operatively, patients are encouraged to meet with a manufacturer representative to learn about devices. Post-operatively, patients are encouraged to contact manufacturers first if they experience device issues. We avoid processing RMAs unless related to clinic error or magnet replacement. If needed, the PCN helps patients navigate these interactions to foster independence. This approach has reduced non-billable tasks and improved patient satisfaction. Ongoing collaboration with manufacturers continues to enhance patient support and clinic efficiency.
Initiative 6: Expanding Collaborative Care
To extend reach into underserved areas, we partner with regional audiologists who now participate in evaluation, activation, and follow-up under shared-care protocols. Our CI team hosts bi-monthly training meetings to build collaborative partnerships. In 2024, six collaborative providers facilitated 12 additional surgeries for our team through this model. This expands care access to remote communities while maintaining continuity and quality of care. We are actively working to support continued education on expanded candidacy to help collaborative clinics build confidence in referrals for borderline CI candidates, which we believe will further extend this program and the referrals made through it.
Program Impact and Results
Since its inception in 2021, our CI program has experienced substantial growth in both surgical volume and geographic reach thanks in large part to these efficiency improvements. The Epic based tracking system has been instrumental in tracking status and metrics for continued growth. Implementation of the PCN role, structured group counseling, streamlined follow up schedules, and robust manufacturer partnerships have all reduced provider workload while increasing patient throughput and satisfaction. Our collaborative care model has expanded service reach and referrals. Together, these strategies have positioned the program for continued scalability.
Future Directions
Next steps include expanding remote programming capabilities to further streamline follow up appointments and triage urgent patient issues. With the addition of an LSLS-certified AVT on our team this year, we aim to enhance pediatric services and better support adults with cognitive concerns or additional rehabilitative needs. We also plan to improve pathways for hearing aid users and grow our network of CI collaborating providers. Continuous evaluation of program data will help us identify key growth areas and prioritize future efficiency improvements.
Conclusion
Scalable cochlear implant programs are critical to addressing care gaps, particularly in underserved regions. Our experience demonstrates that strategic planning, team-based care, and targeted efficiency measures can yield sustainable, high-quality services. This framework may serve as a replicable model for other institutions seeking to expand CI access and improve hearing health outcomes on a regional or national scale.
Acknowledgments:
We would like to thank our Prisma CI Team members, our ICIT course mentors, and our collaborative care partners for their contributions to program development.
About the Authors:
Heather L. Strader, AuD, CCC-A, is a cochlear implant audiologist with Prisma Health Upstate ENT in Greenville, SC, serving pediatric and adult populations. She received her Bachelor of Science from Purdue University and her Doctorate of Audiology from Wayne State University in Detroit, MI. She completed her fellowship with the University of North Carolina Pediatric Cochlear Implant Team and previously worked with the St. Louis Children’s Hospital Pediatric Cochlear Implant Team. Strader leads the Prisma Health CI team toward developing and implementing innovative and efficient care delivery models, facilitating expanded access to care for CI patients in the Upstate and beyond. Heather L. Strader is a consultant for Cochlear Corporation, Advanced Bionics, and Med-El. Correspondence: Heather Strader- [email protected]
Brent Wilkerson, MD, is a fellowship-trained neurotologist and otologist/skull base surgeon at Prisma Health–Upstate and clinical assistant professor of Surgery at the University of South Carolina School of Medicine Greenville. He specializes in complex ear and lateral skull base disorders, directs Prisma’s expanding cochlear implant program, and is dedicated to advancing hearing health access, education, and innovation in the Upstate region.
References
- Nassiri AM, Sorkin DL, Carlson ML. Current Estimates of Cochlear Implant Utilization in the United States. Otol Neurotol. 2022;43(5):e558-e562. doi:10.1097/MAO.0000000000003513
- Neukam JD, Kunnath AJ, Patro A, et al. Barriers to Cochlear Implant Uptake in Adults: A Scoping Review. Otol Neurotol. 2024;45(10):e679-e686. doi:10.1097/MAO.0000000000004340
- Vaerenberg B, Smits C, De Ceulaer G, et al. Cochlear implant programming: a global survey on the state of the art. ScientificWorldJournal. 2014;2014:501738. Published 2014 Feb 4. doi:10.1155/2014/501738
- Dunn CC, Zwolan TA, Balkany TJ, et al. A Consensus to Revise the Minimum Speech Test Battery-Version 3. Am J Audiol. 2024;33(3):624-647. doi:10.1044/2024_AJA-24-00008
- Holder JT, Henry MR, MacDonald AE, Gifford RH. Cochlear Implant Upper Stimulation Levels: eSRT vs. Loudness Scaling. Otol Neurotol. 2023;44(9):e667-e672. doi:10.1097/MAO.0000000000003988
- Holder JT, Hoffman J, Williams H, Gifford RH. The Relationship Between eSRTs and Upper Stimulation Levels in a Large Cohort of Adult Cochlear Implant Recipients. Otol Neurotol. 2024;45(10):e756-e762. doi:10.1097/MAO.0000000000004329