A routine hearing test at birth could be used as a screener for neurodevelopmental differences inclusive of autism
Brain-wave data collected during a hearing test routinely given to newborns could help clinicians spot neurodevelopmental disorders such as autism in early infancy, according to a new Rutgers-led study.
Researchers found that newborns who later received an autism spectrum disorder (ASD) diagnosis had pronounced delays in their brainstem’s responses to sounds. On average, these newborns had a 1.76-millisecond lag – in a system that operates at a microsecond time scale – compared to newborns who developed neurotypically.
These newborns may have difficulty integrating sound with other sensory streams like vision, movement, and pain because of limited access to sound frequency. Furthermore, they may have difficulty communicating socially and learning languages.
The research, published by Proceedings of the National Academy of Sciences (PNAS Nexus) and led by Rutgers School of Arts and Sciences psychology professor Elizabeth Torres, suggests a possible approach for developing a universal screening tool for neurodevelopmental disorders with new avenues for targeted personalized treatments.
“With very little effort and cost, we could build a universal screening test to eliminate disparities in infant neurodevelopment and establish normative scales of such a dynamic process,” said Torres. “This will give us the ability to measure individual departures from these neurotypical ranges, as early as possible, when the nervous system is rapidly changing and adapting to its environment, and the brain-body circuitry is forming.”
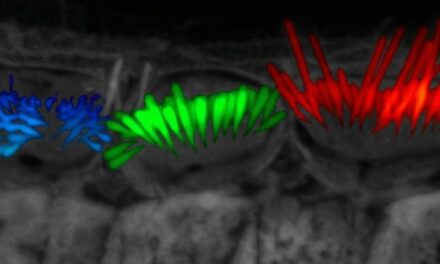
In the study, the researchers examined fluctuations in waveforms – which are often discarded across repetitions – recorded by the Auditory Brainstem Response test that assesses hearing. In this test, clinicians play clicks to sleeping babies, whose brain response is recorded using soft electrodes.
“At birth, the brainstem is already critical for survival functions like breathing, swallowing and excreting, but also serves as a conduit to the neocortex, subcortical regions, the cerebellum and the spinal cord, where emergent control and coordination of actions give rise to basic building blocks of social behaviors,” said Torres. “As a result of the extreme plasticity of an infant’s brain, the earlier the therapeutic intervention, the more effective the treatment will be.”
The results may explain differences in language acquisition, sensory processing, and motor control, which are all fundamental to social interactions and communication as the baby grows and matures. It also explains why young autistic children have excess noise in their movements, with repetitions of actions, or “stimming,” and unexpected responses to various sensory stimuli.
In the experiment, the team first standardized the waveforms to remove anatomical differences, such as head circumference, as a source of variability. They then compared waveforms from infants who were later diagnosed with an autism spectrum disorder to a similar number of babies who were not.
The babies who would go on to receive an ASD diagnosis showed consistently delayed responses to the clicks and reduced access to sound frequencies.
Torres, who leads the Sensory Motor Integration Lab and the New Jersey Autism Center of Excellence, said by the time those with ASD receive their diagnosis in the U.S., and even later abroad, their nervous systems developed compensatory coping mechanisms and circuitry different from neurotypical babies.
Researchers can catch these differences early enough to support the system to process sensory signals within the ranges and timescales that will coincide with those of neurotypical individuals, thus enabling information processing and communication between two systems.
“Research shows that the so-called “repetitive, ritualistic behaviors” are an adaptation of a system that is operating on different hardware and nevertheless, attempting to communicate with us,” said Torres. “Our results call us to rethink what autism really is.”
Rutgers doctoral student Joe Vero and Hannah Varkey, a pre med research assistant at the Sensory Motor Integration Lab, co-authored the study, which was conducted in collaboration with the New York State Institute for Basic Research and the University of Miami.
Source: Rutgers University
Images: Photo 111569260 © Vetre Antanaviciute-meskauskiene | Dreamstime.com