The Audible Contrast Threshold (ACT) test is a new option for measuring functional hearing and listening to help guide the programming of hearing aids.
By Douglas L. Beck, AuD, F-AAA, CCC-A; Ashley Hughes, AuD; and Søren Laugesen, PhD
ACT is a new diagnostic tool which allows hearing care professionals to directly and specifically individualize (i.e., maximize) the help-in-noise features of programmable hearing aids. This can be achieved because ACT has been shown to be an excellent predictor of aided hearing-in-noise performance in complex listening scenarios, without the need for language-specific stimuli. In this article, we explore the foundation of ACT, Spectro-Temporal Modulation (STM), and how ACT compares to traditional speech-in-noise tests.
Importance of Speech in Noise (SIN) Assessment
It is likely that the single most relevant measure of functional hearing and listening is a Speech in Noise (SIN) assessment of good validity. There are many SIN assessment tools available including the QuickSIN1, the Hearing in Noise Test (HINT)2, the AZBio3, the Beck-Benitez4 Two Minute SIN Test, the Words in Noise (WIN) test5, the Bamford-Kowal-Bench Speech-in-Noise Test (BKB-SIN)6, and others.7
The American Academy of Audiology (AAA)8, the American Speech-Language-Hearing Association (ASHA)9, and the International Hearing Society (IHS)10 all recommend SIN assessment in their best practice (BP) statements to assure clinical excellence and a deeper understanding of the patient’s experience, observations, and chief complaint (most often the inability to understand SIN) to better select and provide individual and unique counseling and appropriately programmed technology.
Unfortunately, it appears that fewer than 20% of hearing care professionals (HCPs) perform SIN assessment on every patient.11 Of note, Speech in Quiet (SIQ) scores do not predict or significantly correlate with SIN scores. Wilson12 compared SIQ and SIN scores from more than 3,000 military veterans. Some 70% had Word Recognition Scores (WRS) in quiet which were good or excellent based on NU-6 monosyllabic word lists. However, and of significant clinical importance, when assessed with SIN, only 7% demonstrated normal results. In other words, good-to-excellent WRS in quiet (i.e., SIQ) was not indicative of normal SIN scores for 93% of the subjects.
Real-World Concerns with SIN Assessments
Most SIN tests lack real-world or “ecological validity.” Some SIN tests present speech and noise from the same single loudspeaker (co-located) which rarely happens in the real world, or both speech and noise are delivered to each ear, one ear at a time; also not a common occurrence in the real world. Sometimes the background noise used is a steady-state noise such as white, pink, or speech-shaped noise; all of which is non-linguistic and poses a lesser challenge than actual speech noise with linguistic content might.
Real-life SIN scenarios more likely involve multiple talkers from different directions as well as reverberation, with unique sounds in each ear (with respect to interaural level and timing differences, etc.) which taxes a much broader range of auditory abilities.13 Additionally, many unaided SIN tests are presented at most comfortable level (MCL) which may leave high-frequency (or other) spectral components below the patient’s hearing threshold, such that the measured performance reflects an unknown mix of audibility issues and true SIN ability.
Some SIN measures use sentences, which presumes the patient can recall the exact words in the order presented. Although this may not be a challenging task for a typical 33-year-old patient it may represent a significant issue for an 83-year-old patient, and there are no “age-based” corrections for short-term memory issues within those assessments. Twenty-two percent of people over age 65 years may have mild cognitive impairment (MCI)14 and factors like short-term memory and word order recitation may be problematic. As such, sentence-based SIN assessments should likely take into consideration typical differences in the peripheral and central nervous systems of the populations tested and should likely be normed on those same populations.
Finally, SIN tests suffer from language specificity. Generally, people can be expected to perform best while using their native language. When using SIN assessments offered in a patient’s second or third language, we simply do not know how to interpret the results. SIN tests may be misleading as the first language-to-second language auditory processing (i.e., conversion) the patient must perform, adds uncontrolled variables to the assessment, and may render the assessment of little (or unknown) clinical value.
Further reading: How to Optimize Your Practice Management Software
Why HCPs Typically Do Not Perform SIN Assessment
The reasons for not performing SIN assessment vary and likely include: SIN assessment takes too much time, SIN assessments are expensive, SIN assessments require special hardware and software, SIN assessments are not required, SIN is not deemed necessary, SIN tests not available in the required language, and other assumptions. However, SIN assessments often take less than 5 minutes, there are free SIN assessment tools available, and many SIN assessments do not require special equipment. However, as noted below (see Chart 1), many lack the ecological validity to achieve the potential benefits of SIN testing.

All the potential benefits of SIN assessments (listed in Chart 1, above) must be well-founded on item 1: a realistic understanding of the SIN ability of the patient. Yet, this core principle requires that the SIN test applied has sufficient ecological validity. This problem was discussed above in the “Real World Concerns with SIN Assessments” section, and these concerns remain a huge impediment in 2024. As such, there are many reasons to look for an alternative or supplement to typical clinical SIN tests. The Audible Contrast Threshold (or simply ACT) test is such an alternative. The ACT test offers high predictive power regarding accurately aided speech-in-noise performance in complex ecologically valid conditions, it requires only a few minutes to administer, it offers clinical simplicity and familiarity, and it is not language specific.
SRT/SNR-50/SRT-50
There are three common terms used to quantify and describe the patient’s ability to understand SIN: the Speech Reception Threshold (SRT), the Signal-to-Noise Ratio 50 (SNR-50), and the SRT-50. Although all three terms indicate the same thing, the term “SRT” can be confusing, given the more common spondee-based SRT in quiet which is reported in dB HL. Some HCPs use SRT-50 to help identify the SIN measure being assessed. Each term describes the signal to noise ratio (SNR, in decibels, dB) required for the patient to achieve 50% correct recognition of speech stimuli in a background of noise. The process of obtaining the SRT/SNR-50/SRT-50 is familiar as the HCP seeks the “true” or representative threshold using a protocol like the one used for pure tone threshold identification.15
Although highly variable, people with normal thresholds tend to understand SIN better than people with hearing loss. As the PTA increases, so too, does the general need for an improved SNR. Dillon16 suggested that for every additional 10 dB of hearing loss an additional 3 dB of SNR is needed to maintain intelligibility due to increasing cochlear distortions associated with increasing hearing loss.
Additionally, people with an SRT-50 of 0-3 dB typically are characterized as having normal or near normal SIN ability, whereas someone with an SRT-50 of 9 dB often has a moderate SIN disability, with or without elevated thresholds (see Chart 2).

However, there is considerable variability in SIN performance, which is not accounted for by the audiogram.17-19 Further, people with pure tone thresholds in the normal range may have elevated SRT-50s due to cochlear synaptopathy, auditory neuropathy, attention deficit disorder, mild cognitive impairment, dementia, auditory processing disorders, and more.19 Quantifying an approximate SIN disability is very important. However, it is equally important to use that information pragmatically, such as to maximally program a hearing aid to accommodate SIN disability.
Spectro-Temporal Modulation
The search for a reliable and simple assessment to estimate SIN ability was catapulted by the Spectro-Temporal Modulation (STM) detection tests described by Chi et al.20 and Bernstein et al.21 The latter study demonstrated impressively high correlations between STM detection thresholds and SIN test results in a group of listeners with hearing impairment. Unfortunately, a subsequent study22 indicated severe problems with clinical viability, as roughly one-third of the tested clinical population was unable to complete the proposed STM test as intended. Thus began a seven-year research effort from the Interacoustics Research Unit, the Eriksholm Research Centre, and Oticon’s Centre for Applied Audiology Research, in Denmark. Their research focused on optimizing stimulus attributes and testing procedures, to translate the early STM research tool into a clinically viable assessment tool.
The result of this multi-center, multi-year venture is now known as the Audible Contrast Threshold (ACT) test. The ACT is designed to maintain the all-important high correlations associated with aided SIN ability in real-world scenarios as well as offer clear guidelines on how to use the ACT results for improved individualized hearing-aid fittings. Contemporary evidence indicates ACT results are highly predictive of real-life aided speech-in-noise performance. Regarding Chart 1, ACT satisfies items 1-4. Note that SIN tests still have their role in clinical practice to serve item 5 in Chart 1.
While ACT is a diagnostic test used up-front to guide the hearing-aid fitting process, traditional SIN tests with real speech signals remain the right tool for addressing fitting outcomes, e.g. by comparing SIN performance with and without hearing aids.
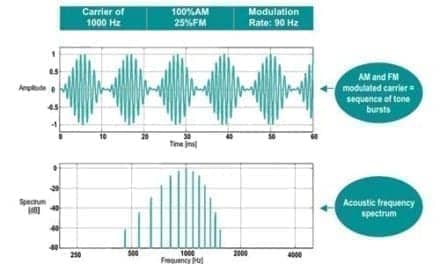
The sound stimuli used for ACT testing is a train of bursts that are either “reference” or “target.” The reference sounds are 1-second-long bursts of band-limited pink noise. The targets are also pink-noise bursts onto which a downward moving (siren-like) spectro-temporal ripple is imposed. This adds a siren-like quality to the target sounds, and the patient’s task is to respond by pressing the response button when they detect the siren sound.
ACT testing starts with clearly detectable (i.e., easy) modulations. The purpose of the test procedure is to pinpoint the threshold at which the patient can just identify the siren sound. This procedure follows the Hughson-Westlake bracketing protocol, familiar from pure-tone audiometry, with a 2 dB nCL step size. Of note, the stimuli are shaped specifically to each ear and frequency, based on the patient’s pure-tone audiogram, to ensure that the stimulus is presented at least 15 dB above the threshold of audibility throughout the frequency range of interest.23
ACT results are referred to as normalized Contrast Level (nCL dB) within the range from -4 to 16 dB. The nCL scale is normalized such that 0 dB nCL corresponds to the median performance of young people with normal thresholds. Sub-zero ACT results indicate better-than-normal performance while positive nCL values indicate increasing degrees of “contrast loss” or increasingly problematic listening ability. See Chart 3 below.

Research Highlights on STM and SIN Testing
Zaar et al. (2023a)24 reported 13 elderly people with hearing loss and their ability to perform a modified STM task, and correlated those results with their SRT-50s. Both STM and SIN testing were done with careful compensation for audibility. All 13 subjects were able to complete the STM tasks. The authors report their STM test was suitable for elderly listeners with moderate-to-severe hearing loss and their STM results successfully predicted SRT-50s within statistical significance.
Notably, participants were tested in two SIN scenarios: One typical clinical setup with target speech and steady-state masking noise from the same loudspeaker (co-located) and another ecologically valid (i.e. more realistic) setup in which the target speech originated from a loudspeaker in front with a noise background of four competing talkers from separate loudspeakers in the rear hemisphere with representative reverberation. Correlations between STM performance and SRT-50 were consistently higher for the ecologically valid condition, indicating that as the SIN test was made more realistic, the relationship to STM was strengthened. The authors stated their results indicate that a clinically applicable STM test would likely be useful to help estimate speech-in-noise performance without the time-consuming and language-specific requirements of a more traditional SIN assessment, all of which should be useful to individualize hearing-aid programming.
In Zaar et al. (2024)25 these results were extended into a new group of 30 hearing-aid users. The 30 subjects listened in the (abovementioned) more ecologically valid SIN test protocol through hearing aids (all advanced features disabled). Participants were specifically recruited who had severe speech-in-noise challenges and it was found that the relationship between STM and SIN performance was maintained for the severely challenged group. STM detection threshold predicted aided SRT-50s (R2 = 0.61) and STM further correlated with the additionally measured benefits of directionality and noise reduction (R2 = 0.51). Overall, the authors state the STM represents a “valuable tool” for detecting and quantifying SIN problems, as well as predicting the need for additional hearing-aid processing.
Zaar/Simonsen et al. (2023)23 took the modified version of the STM test used in the studies above (i.e., the research prototype) and translated that into the clinically viable Audible Contrast Threshold test. Validity was verified by re-testing 28 subjects from Zaar et al. (2024)25 with ACT. Additionally, 25 young participants with normal thresholds were tested with ACT to create the normalized Contrast Level (nCL) scale outlined in Chart 3. High test-retest reliability was also found. The authors concluded that ACT was quick and simple, reliable, and clinically viable, with test times of only two to three minutes following traditional pure-tone threshold testing, which is needed for the audibility compensation used with ACT.
Zaar et al. (2023b)26 report results from two new language populations (N=100 total German and Japanese speakers), adding to the evidence base for the relationship between ACT and aided SIN performance. Further, excellent reliability was observed for ACT used in people with hearing loss. Finally, this study presents the evidence underlying the fitting guidelines related to ACT.
Further reading: Audible Contrast Threshold (ACT) Testing in MedRx Audiometers
Discussion
The applicability of the ACT assessment has been well-researched and documented and has a strong correlation with complex ecologically valid aided SIN assessment. As noted above, best practice guidelines from nationally well-known and respected academies, associations, and societies endorse SIN measures as the status quo. This new alternative (ACT) is particularly good news, because simpler and less informative clinical SIN tests have not been well accepted by professionals—probably due to the cost of additional equipment, clinical time constraints, and challenges with non-native patients.
The simplicity, speed, and language-independence of ACT allows the HCP to assess the patient’s ability to understand speech in noisy and other challenging situations, when appropriately aided to compensate for any audibility-related deficits. This assessment can facilitate unique person and experience-based discussions about reasonable expectations, aural rehabilitation options and strategies, the selection of hearing aids, and individualized programming of appropriate help-in-noise technology. As such, the Interacoustics ACT represents a new opportunity to gather an important clinical measure in an efficient and effective manner with a time-, language-, and financially friendly clinical protocol.
Douglas L. Beck, AuD, F-AAA, CCC-A, is among the most prolific authors in audiology. His publications address a wide variety of audiology, clinical, academic, and professional topics. He can be reached at [email protected] or www.douglaslbeck.com.
Ashley Hughes, AuD, works for Interacoustics US, and is the main point of contact for all audiometry, impedance, OAE, hearing aid fitting, and telehealth solutions. Prior to joining Interacoustics, she first worked clinically and then as a research audiologist.
Søren Laugesen, PhD, is the research manager for the Interacoustics Research Unit. Coming from a background in acoustics and digital signal processing at the Technical University of Denmark, he spent 19 years with the Eriksholm Research Centre as a researcher and project manager before joining the Interacoustics Research Unit in 2016
Original citation for this article: Beck D., Hughes A., Laugesen S. Using the ACT Test for Speech in Noise Ability Assessment. Hearing Review. 2024;31(4):8-14.
References
- Killion MC, Niquette PA, Gudmundsen GI, Revit LJ, Banerjee S. Development of a quick speech-in-noise test for measuring signal-to-noise ratio loss in normal-hearing and hearing-impaired listeners. J Acoust Soc Am. 2004 Oct;116(4 Pt 1):2395-405. doi: 10.1121/1.1784440. Erratum in: J Acoust Soc Am. 2006 Mar;119(3):1888. PMID: 15532670.
- Nilsson M, Soli SD, & Sullivan JA. (1994). Hearing in Noise Test (HINT) [Database record]. APA PsycTests. https://doi.org/10.1037/t71961-000
- Vermiglio AJ, Leclerc L, Thornton M, Osborne H, Bonilla E, Fang X. Diagnostic Accuracy of the AzBio Speech Recognition in Noise Test. (2021): J Speech Lang Hear Res. Aug 9;64(8):3303-3316. doi: 10.1044/2021_JSLHR-20-00453. Epub 2021 Jul 8. PMID: 34236930.
- Beck DL & Benitez L. (2019): A Two Minute Speech in Noise Test. Protocol and Pilot Data. American Academy of Audiology. Audiology Today. May/Jun. https://www.audiology.org/news-and-publications/audiology-today/articles/a-two-minute-speech-in-noise-test-protocol-and-pilot-data/
- Wilson RH, Carnell CS, Cleghorn AL. (2007): The Words-in-Noise (WIN) test with multitalker babble and speech-spectrum noise maskers. J Am Acad Audiol. Jun;18(6):522-9. doi: 10.3766/jaaa.18.6.7. PMID: 17849640.
- Bench J, Kowal A, Bamford J. The BKB (Bamford-Kowal-Bench) sentence lists for partially-hearing children. Br J Audiol. 1979;13(3):108-112. doi:10.3109/03005367909078884
- Wilson RH, McArdle RA, Smith SL. An Evaluation of the BKB-SIN, HINT, QuickSIN, and WIN Materials on Listeners With Normal Hearing and Listeners With Hearing Loss. J Speech Lang Hear Res. 2007 Aug;50(4):844-56. doi: 10.1044/1092-4388(2007/059). PMID: 17675590.
- American Academy of Audiology (AAA): https://www.audiology.org/practice-resources/practice-guidelines-and-standards/
- American Speech-Language-Hearing Association (ASHA): https://www.audiology.org/practice-guideline/american-speech-language-hearing-association-clinical-practice-guideline-on-aural-rehabilitation-for-adults-with-hearing-loss/
- International Hearing Society (IHS): Best Practices Recommendation for Fitting and Dispensing Hearing Aids. https://myhome.ihsinfo.org/Images/IHS%20Best%20Practices%20Recommendation%20for%20Fittting%20and%20Dispensing%20Hearing%20Aids_02052020_FINAL%20updated%202020.pdf
- Beck DL. (2023): Speech in Noise Testing: Pivotal and Rare. The Hearing Journal. December. 76(12). https://journals.lww.com/thehearingjournal/fulltext/2023/12000/speech_in_noise_testing__pivotal_and_rare.1.aspx
- Wilson R. (2011): Clinical experience with the Words-In-Noise Test on 3,430 veterans: Comparisons with PT Thresholds and WRS in Quiet. JAAA
- Neher T, Behrens T, Carlile S, Jin C, Kragelund L, Petersen AS, & Schaik A van. (2009). Benefit from spatial separation of multiple talkers in bilateral hearing-aid users: Effects of hearing loss, age, and cognition. International Journal of Audiology, 48(11), 758–774. https://doi.org/10.3109/14992020903079332
- Manly JJ, Jones RN & Langa KM (2022): Estimating the Prevalence of Dementia and Mild Cognitive Impairment in the US. JAMA Neurol. 79(12), 1242-1249, doi:10.1001/jamaneurol.2022.3543
- Hughson W & Westlake H. (1944): Manual for program outline for rehabilitation of aural casualties both military and civilian. Trans Am Acad Ophthalmol Otolaryngol. 48(Suppl):1–15.
- Dillon H. (2012): Hearing Aids 2nd Edition (text book). Boomerang Press, Thieme
- Plomp R, 1986. A signal-to-noise ratio model for the speech reception threshold of the hearing impaired. J. Speech Hear. Res. 29 (2), 146–154. doi:10.1044/jshr. 2902.146.
- Lopez-Poveda EA, 2014. Why do I hear but not understand? Stochastic undersampling as a model of degraded neural encoding of speech. Front. Neurosci. 8, 348. doi:10.3389/fnins.2014.00348, Article.
- Beck DL, Danhauer JL. (2019): Amplification for adults with hearing difficulty, speech in noise problems – and normal thresholds. J Otolaryngol ENT Res. 2019;11(1):84-88. DOI: 10.15406/joentr.2019.11.00414
- Chi T, Gao Y, Guyron MC, Ru P, Shalla S. (1999): Spectro-temporal modulation transfer functions and speech intelligibility J. Acoust. Soc. Am. 106, 2719–2732 (1999) https://doi.org/10.1121/1.428100
- Bernstein JGW, Mehraei G, Shamma S, Gallun FJ, Theodoroff SM, Leek MR, 2013. Spectrotemporal modulation sensitivity as a predictor of speech intelligibility for hearing-impaired listeners. J. Am. Acad. Audiol. 124 (4), 293–306. doi:10.3766/jaaa.24.4.5.
- Bernstein JGW, Danielsson H, Hällgren M, Stenfelt S, Rönnberg J, Lunner T, 2016. Spectrotemporal modulation sensitivity as a predictor of speech-reception performance in noise with hearing aids. Trends Hear. 20, 1–17. doi:10.1177/ 2331216516670387.
- Zaar J/Simonsen LB, Sanchez-Lopez R, & Laugesen S. (2023). The Audible Contrast Threshold (ACT™) test: A clinical spectro-temporal modulation detection test. MedRXiv. https://doi.org/10.1101/2023.10.12.23296977
- Zaar J, Simonsen LB, Dau T, & Laugesen S. (2023a). Toward a clinically viable spectro-temporal modulation test for predicting supra-threshold speech reception in hearing-impaired listeners. Hearing Research, 427, 108650. https://doi.org/10.1016/j.heares.2022.108650
- Zaar J, Simonsen LB, & Laugesen S. (2024). A spectro-temporal modulation test for predicting speech reception in hearing-impaired listeners with hearing aids. Hearing Research, 108949. https://doi.org/10.1016/j.heares.2024.108949
- Zaar J, Ihly P, Nishiyama T, Laugesen S, Santurette S, Tanaka C, Jones G, Vatti M, Suzuki D, Kitama T, Ogawa K, Tchorz J, Shinden S, & Jürgens T. (2023b). Predicting speech-in-noise reception in hearing-impaired listeners with hearing aids using the Audible Contrast Threshold (ACT™) test [Preprint]. PsyArXiv. https://doi.org/10.31234/osf.io/m9khu
- Gustav Mueller HG, Ricketts T, Hornsby BWY. 20Q: Speech-in-Noise Testing – Too Useful to be Ignored! November 6, 2023. www.audiologyonline.com/articles/20q-speech-in-noise-testing-28760