Inside Clinical Research | March 2016 Hearing Review
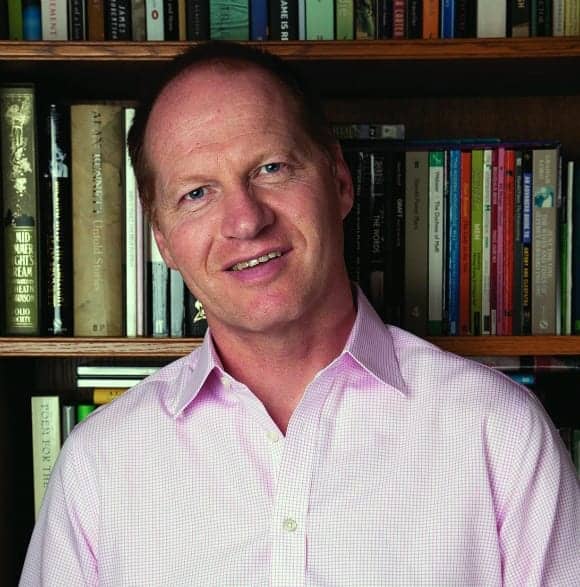
A few weeks ago I had the opportunity to speak with my friend and colleague, Kevin Munro, PhD. Dr Munro is the Ewing Professor of Audiology in the School of Psychological Sciences (SPS) at the University of Manchester in the UK where he leads the SPS Audiology and Research Group and is an Honorary Consultant Clinical Scientist in the Central Manchester University Hospital’s NHS Foundation Trust. His research areas-of-expertise range from aging and neural plasticity of the auditory system, to the selection and verification of hearing aids, off-frequency listening, cochlear “dead regions,” listening effort, fatigue, and more. Because Dr Munro and colleagues recently published several interesting articles about cochlear dead regions (DR), I sought to explore this fascinating subject in greater detail, with an emphasis on applying this knowledge in the clinic.
Beck: Good Morning Kevin. Thanks for your time today.
Munro: Hi Doug. Nice to be with you, as always.
Beck: I’d like to speak with you about cochlear dead regions and how these might impact typical hearing aid fittings. To be clear, when we talk about cochlear DRs, we’re talking about loss or damage to the inner hair cells (IHCs) of the cochlea, is that correct?
Munro: Right, IHCs or the ascending auditory neurons. Cochlear DRs are the focus of our 2016 papers1,2 and it’s an excellent topic for clinicians. That is, it’s a great and meaty topic to discuss as there’s a lot of information to digest.
Beck: I agree. It seems most clinicians are confused as to how to handle DRs due to the various definitions, protocols, publications, and misunderstandings. When I ask audiologists and dispensers across the globe “What do you do if you know the patient has a cochlear DR?” I usually get two answers. The first is to avoid high frequency amplification, and the second is to use frequency lowering technology.
Munro: Yes, I hear these solutions, too. However, I also hear “I match the hearing aid response to a prescription target but I am not sure if I should be doing something different.”
I think the reason for uncertainty is that studies using adults with extensive cochlear DRs have reached a different conclusion from the studies of adults with relatively limited (more common) cochlear DRs.
Beck: Exactly! The implications for amplification are likely different depending on how extensive the cochlear DR is. Let’s step back a bit and review what we know and how we got here. The early papers on DRs were absolutely fascinating, and arguably the most important of them were written by our mutual friend and colleague, Brian CJ Moore, PhD, and his associates.
In 2001, Moore3 noted that, given moderate-to-severe hearing loss, cochlear DRs are “relatively common.” Further, and very importantly, he noted one could not reliably determine a DR based on an audiogram or a description of the quality or noisiness of the sound. He reported that psychophysical tuning curves (PTCs) could be used to identify cochlear DRs, but these can be time consuming and not likely to be used in a clinical setting. As such, Moore introduced a cochlear DR identification protocol called the Threshold Equalizing Noise (TEN).4 He noted that providing amplification well inside an extensive cochlear DR does not improve intelligibility, and in some adults’ performance is actually reduced. As a result, he recommended “there may be some benefit in amplifying frequencies up to 50-100% above the start of a high-frequency dead region.” That was truly a seminal paper in our literature and offered great insight to cochlear DRs.
Munro: Yes, that’s a good summary and, if I may say so, this was one of the few studies that suggested additional psychoacoustics measurements might influence how a hearing aid should be fitted. I believe it’s important to note that the participants in these earlier studies tended to have what we would consider extensive cochlear DRs. The participants without cochlear DRs performed better than those with cochlear DRs, but then again, the participants without DRs didn’t have such a severe hearing loss, either. That’s an important observation because it is pretty hard to find individuals with a severe hearing loss who don’t have a cochlear DR.
Beck: That’s right, once a patient/subject has hearing loss more significant than 65 or 70 dB HL, there is almost certainly IHC involvement and, of note, IHC damage is very often perceived as distortions or noise. Nonetheless, it seems to me the more likely reason the majority of people perceive noise or distortion (given hearing loss and amplification) is the fact that sensorineural hearing loss (SNHL) is characterized by at least four different distortions—threshold, dynamic range, timing, and loudness—and so when a SNHL is amplified, it makes good sense that the patient will report it sounds distorted. Again, for most people with SNHL, the distortion is more likely to come from the SNHL than a true DR.
Munro: That’s a really interesting point. SNHL is indeed characterized by elevated hearing thresholds, reduced dynamic range, and poor frequency and timing resolution, as you noted. And so, yes, arguably the perceptual consequences might be described as distortion, but that doesn’t mean there is, or is not, a cochlear DR present. As Moore said, you cannot determine the existence of a DR based on an audiometric configuration; you’re just as likely to be right or wrong. To identify a DR, it must be tested.
Beck: Right, and if one does not test specifically for DRs (using psychoacoustic tuning curves or the TEN test) there is no way to know. OK then, so back to the early studies…
Munro: Sure…and so my point was that it’s very hard to find people with severe or profound hearing loss who do not have a cochlear DR. If we identify a cochlear DR group, they likely have more hearing loss. In theory, either the DR, or the hearing loss itself, might explain why they perform poorly, yet we cannot say with certainty it was one factor or the other. Doug, in your lectures, you often quote Robyn Cox’s work from 2011 and 2012.5,6 In those very interesting papers, Dr Cox and her colleagues examined hundreds of people with and without cochlear DRs, using a matched control group. They concluded a few rather important findings. First, they agreed that about one-third of the people with sloping moderate-to-severe SNHL had at least one DR. Second, and perhaps more importantly, they found that the best overall hearing aid strategy was fitting the patient with hearing aid amplification to a recognized hearing aid prescription (ie, do not reduce high frequencies).
Beck: And that gets us to your new publications.1,2
Munro: Of course! We were interested in finding out how common are DRs in the typical adult patient presenting at our clinics in the UK. Also, we wanted to assess whether a modification of the hearing aid prescription would be beneficial for people with a cochlear DR. In our third and final study with adults, we took everyone who came through the door, performed the TENS test and PTC measurements, to determine the presence of cochlear DRs.
As Cox found, about one-third of our adult subjects had evidence of cochlear DRs.7 And of interest, yes, the two tests very much resulted in the same finding.8 So, we demonstrated that cochlear DRs are reasonably common, but importantly, they tended to occur over a relatively narrow frequency range—usually around 3000 Hz and 4000 Hz where the hearing loss is most marked. This means the more common hearing aid patients are generally different from those individuals with the more extensive DRs used in the earlier studies.
Beck: That is an excellent point.
Munro: After that, we examined the benefit patients received from their hearing aid fittings, using matched groups. We used control groups with the same/similar audiometric thresholds as the experimental group. I believe we had about 18 controls and 18 experimental participants. We measured benefit using speech in quiet and also speech in noise as outcome measures. Like Dr Cox, we used NAL as prescribed and compared the outcome with NAL and with reduced high frequency amplification. We were keen to test the patients using hearing aids because we wanted to know about the real-world implications with current devices.
Beck: And what did you find?
Munro: Of course it goes without saying that individuals did better in quiet than in noise; that’s pretty much a given. We further observed that, as we reduced high frequency gain, performance decreased. The patients always did better in quiet using the NAL prescription and there was no difference in the two groups. Indeed, both groups performed less well in background noise. However, in noise we got a slightly different pattern of results. Participants did best when we matched NAL across the frequency range, but the group with the cochlear DRs did a little worse in noise than the people without DRs.
Beck: What if you changed the hearing aid protocol to reduce the high frequencies?
Munro: I was just coming to that Doug. This is the most important finding in the study. The DR group did not perform any better if we reduced high frequency amplification, although, admittedly, we didn’t give them an opportunity to acclimatize to the response with reduced high frequency.
Beck: Let me summarize to be clear we’ve represented this as clearly as possible. We know that cochlear DRs exist, and DRs are perhaps present in one-third or more of our typical hearing aid patients. However, in typical hearing aid patients, the DR is usually relatively restricted in bandwidth and the best overall protocol is to fit to the prescription target across the frequency; that is, do not withhold high frequency amplification.
Munro: Yes, that’s a pretty good summary, and that helps support the findings of Cox et al.5,6 Of course, it does not contradict the findings in the earlier studies—it’s just that the earlier studies used patients with more extensive hearing loss and more extensive DRs than your typical adult hearing aid user.
Beck: And it seems to me that, for the less common situation where the patient does have an extensive cochlear DR, it makes sense to focus on increasing the signal-to-noise ratio (SNR) via remote microphones and/or FM systems.
Munro: Absolutely, improving SNR is the primary issue whenever there is a SNHL. In fact, there are times that normal-hearing individuals could benefit from a device that improves SNR in challenging listening environments. Improving the SNR will generally offer more benefit in more situations than will reducing high frequencies and applying frequency lowering.
Another consideration for people with severe-to-profound hearing loss who have terrible word recognition scores is, of course, the cochlear implant (CI). Candidacy for CIs has become much more liberal over the years and the benefits are generally excellent. So, when given a patient who has a severe hearing loss, extensive cochlear DRs, and who receives little benefit from hearing aid amplification, it’s usually worth seriously considering CIs or a combination of acoustic and electrical stimulation.
Beck: I have to agree. Thanks for your knowledge and insight, and thanks for your time today.
Munro: My pleasure Doug. I’ll look forward to the next time our paths cross!
References
-
Pepler A, Lewis K, Munro KJ. Adult hearing aid users with cochlear dead regions restricted to high Frequencies–Implications for amplification. Int J Audiol. 2016;55:1:20-29.
-
Pepler A, Munro KJ, Lewis K, Kluk K. Adult hearing aid users with cochlear dead regions restricted to high frequencies: implications for amplification. Int J Audiol. 2016;55:20-29. PMID: 26460797.
-
Moore BCJ. Dead regions in the cochlea: Diagnosis, perceptual consequences, and implications for the fitting of hearing aids. Trends Amplif. 2001;5(1)[Mar]:1-34. doi: 10.1177/108471380100500102
-
Moore BCJ. Testing for cochlear dead regions: Audiometer implementation of the TEN(HL) test. Hearing Review. 2010;17(1):10-16,48. Available at: https://hearingreview.com/2010/01/testing-for-cochlear-dead-regions-audiometer-implementation-of-the-tenhl-test
-
Cox RM, Alexander GC, Johnson J, Rivera I. Cochlear dead regions in typical hearing aid candidates – Prevalence and implications for use of high frequency speech cues. Ear Hear. 2011;32:339-348.
-
Cox RM, Alexander GC, Johnson J, Rivera I. Implication of High Frequency Cochlear Dead Regions for Fitting Hearing Aids to Adults with Mild to Moderately Severe Hearing Loss. Ear Hear. 2012; 33:573-587.
-
Pepler A. Munro KJ, Lewis K, Kluk K. Prevalence of cochlear dead regions in new and existing adult hearing aid users. Ear Hear. 2014; 35:e99-e109. PMID: 24496291.
-
Pepler A, Munro KJ, Lewis K, Kluk K. Repeatability, agreement and feasibility of using the threshold equalizing noise test and fast psychophysical tuning curves in a clinical setting. Int J Audiol. 2014;53(10)[Oct]:745-52. PMID: 24909593.
Douglas L. Beck, AuD, is Director of Professional Relations at Oticon Inc. Dr Beck’s audiology career began at the House Ear Institute in cochlear implant research and intraoperative cranial nerve monitoring. In 1988, he became Director of Audiology at Saint Louis University, and 8 years later co-founded an audiology practice in St Louis. In 1999, Dr Beck became Editor-in-Chief of AudiologyOnline.com, SpeechPathology.com, and HealthyHearing.com, then joined Oticon in 2005. Since that time he has also served as the Web Content Editor for the American Academy of Audiology (AAA), and is an Adjunct Professor of Audiology at Lamar University and an Adjunct Associate Professor of Audiology at the University of Hawaii.
Correspondence can be addressed to Hearing Review or Dr Beck at: [email protected]
Original citation for this article: Beck DL. Cochlear Dead Regions and Hearing Aid Fittings: An Interview with Kevin Munro, PhD. Hearing Review. 2016;23(3):40.?