Summary:
Effective counseling—both educational and personal adjustment—is central to successful audiologic care and becomes even more critical when patients or their communication partners present with concomitant communication disorders.
Key Takeaways:
- Counseling skills are as important as, or more important than, technological advances in ensuring patient success and satisfaction with audiologic care.
- Audiologists must adapt counseling and communication strategies to accommodate patients or families dealing with additional speech, language, voice, or cognitive disorders.
- Direct patient engagement, person-centered care, and appropriate referrals to speech-language pathologists or other providers help preserve patient autonomy and improve outcomes.
By John Greer Clark, PhD; and Kristina M. English, PhD
Portions of this article are excerpted from the text Counseling-Infused Audiologic Care, 4th edition, available through Amazon.
Our Counseling Imperative
Thirty-five years ago, Hawkins (1990) stated that the importance of technological advances in audiology may prove of minor importance to our final success with patients when compared to the counseling and rehabilitative aspects of the care we provide. More recently, Hall (2025) reinforced this statement noting that counseling is more important for audiologists than any current or future technological advance.
When patients and families make appointments, they expect to encounter audiologists who have answers to their questions (patient education, or content counseling) as well as empathy for their circumstances (a key to personal adjustment counseling). Audiologists have long recognized the need to provide proper counseling to their patients and such requirement of the profession is enshrined within audiology scope of practice statements (American Academy of Audiology, 2023; American Speech-Language-Hearing Association, 2018). When provided most effectively, content counseling and personal adjustment counseling both include the precepts of person-centered care with the two types of counseling inextricably intertwined such that the success of one is intimately tied to the success of the other.
In spite of the accepted importance of the delivery of patient counseling during diagnostic and rehabilitative services, audiologists are frequently uncomfortable or perceptually ill-prepared to provide this vital component of patient care (Aslan, Yücel, & Atkins,2018; Gold & Gold, 2021; Woodward & Saunders, 2023). A perceived discomfort with, or lack of preparation to provide, proper counseling during audiologic consultations may be increased when patients with hearing loss, or their primary communication partner, are contending with communication difficulties arising from disorders separate from hearing loss.
When a concomitant communication disorder is present within the audiologic appointment, a familiarity with this disorder can improve reception of the information given within the clinical exchange as well as the personal adjustment support counseling that is provided. The purpose of this article is to provide some basic background in five different disorders that impact patient communication along with suggestions to facilitate more successful patient interactions during clinic visits.
A Historical Context
What is now called the American Speech-Language-Hearing Association sprang from an informal meeting of the National Association of Teachers of Speech (NATS) one hundred years ago in New York City. The NATS was an association for those interested in theater, debate, and rhetoric. Some NATS members were more interested in speech correction and what evolved later that year as the American Academy of Speech Correction, subsequently became the American Society for the Study of Disorders of Speech, the American Speech Correction Association, the American Speech and Hearing Association, and finally in 1978 the American Speech-Language-Hearing Association while maintaining its familiar “ASHA” acronym (American Speech-Language-Hearing Association, n.d.). An informal meeting at an ASHA convention hosted by James Jerger led to the formation of the American Academy of Audiology (AAA) as an association fully “of, by, and for audiology” in 1988.
Before the establishment of AAA and the creation of the professional doctorate in audiology, students seeking to become audiologists came almost exclusively from each year’s pool of undergraduate students in speech-language pathology. While many students enrolled in a doctor of audiology program today still come from a speech-language pathology background, increasingly this is not so. Yet the management of communication disruptions based on the presence of impaired hearing is exacerbated when either the patient or a primary communication partner has a concomitant disorder of speech, language, or vocal production, or cognitive function.
Concomitant Communication Disorders
While attending to hearing, vestibular, or sound tolerance disorders, audiologists frequently see patients or patient communication partners who may have concomitant speech or vocal production difficulties, neurologically based language impairments, and/or cognitive impairments. Any of these disorders can have a negatively synergistic impact on the audiologic treatment provided.
When counseling audiology patients who have concomitant communication disorders, it frequently appears easier to address questions to the accompanying communication partner because the dialogue will flow more smoothly. It is important for us to be aware of the impact this may have on patients who may quickly feel like a third party to their own treatment plan. As much as possible, questions and statements should be directed to the patient. If dialogue is to be directed to the accompanying family member or caregiver, the patient’s permission to redirect the dialogue should always be obtained from the patient.
Although treatment of a non-audiologically-based communication disorder is clearly outside the audiologist’s scope of practice, it is squarely within our scope of practice to assist when hearing loss impacts these disorders. Frequently, this will entail ensuring that appropriate consultation with a speech-language pathologist has been made. This article looks at five conditions that the audiologist should be prepared for when a patient or patient partner presents with a concomitant communication disorder. The discussion here is provided simply as an overview. The interested clinician will find further information within a variety of graduate texts (e.g., Owens & Farinelli, 2019; Roth & Worthington, 2025; Stemple, Roy & Klaben, 2020).
Apraxia of Speech
Apraxia is a motor disorder that interferes with a body part’s reception of motor commands from the brain. Apraxia of speech is a motor disorder arising from damage to the areas of the brain that govern speech production, resulting in difficulty sequencing sounds in syllables and words. Intelligence is unaffected in various forms of apraxia. Those with apraxia are fully aware of their intended message, but the brain fails to coordinate the speech musculature, resulting in a message different from the intended message, frequently with words that might appear to be made up. Naturally, frustration is present for the speaker and the listener and is only exacerbated when one of the communication partners has a hearing loss.
So What Can the Audiologist Do? In spite of the expressive speech difficulties experienced with apraxia of speech, speech understanding is unaffected by the disorder. The delivery of person-centered care necessitates a more balanced talk-time distribution to gain a better appreciation of the patient’s perspective of hearing loss and to better tailor our treatment approach to a patient’s expressed needs and concerns. When counseling the patient with apraxia of speech, to ensure we are understood, we may need to make no further accommodations than we would when talking with any other patient with hearing loss. Rather, the challenge is ensuring that we understand the patient as fully as possible. Toward this end, we should not rush the patient when the patient is speaking; we should avoid finishing sentences for the patient; and we should reduce anxiety and pressure by reassuring the patient that it is okay to take the time they need. Instead of using the normally more appropriate open-ended questions, questions that offer an either/or response or that are phrased to elicit a simple “yes” or “no” can be helpful. More complex questions should be broken down into their component parts. We should offer a pen and paper, as this may be a preferred mode of communication. If available, we should encourage the patient to use their communication board or other alternative augmentative communication (AAC) device, familiarizing ourselves with their system when possible. Even if we are having difficulty understanding the patient’s speech, it is both helpful and appreciated if we verbally acknowledge attempts to communicate.
Communication may be further facilitated by maintaining direct eye contact and displaying body posturing that shows a concerned interest in what the patient is attempting to convey (leaning in toward the patient, nodding as appropriate, uncrossing the arms to appear more open and encouraging). A verbal courtesy known as “signposting” reminds patients of our need to summarize consultations in electronic medical records while reinforcing our efforts to stay patient-focused (English, 2019; Manalastas, Noble, Viney & Griffin, 2020). Once notes are complete, we should clearly turn away from our computers and re-establish eye contact.
We should remain mindful that communication can be tiring for those with apraxia of speech and breaks should be offered as needed. While always addressing the patient directly, if patient consent is obtained, an accompanying communication partner may be able to help interpret what the patient is trying to say.
When the appointment is over, a chart notation of the patient’s preferred communication methods will facilitate the next appointment, especially if the patient is seen by a different provider. Aphasia and dysarthria may be concomitant disorders with apraxia of speech and further accommodations may be needed when these are present.
Dysarthria
As with apraxia, dysarthria is an expressive speech disorder and receptive language is typically intact unless there is a coexisting condition such as aphasia. Dysarthria is a motor speech disorder affecting the muscles of the mouth, face, and respiratory system which may be weakened or may move more slowly or not at all. Like most motor speech disorders, dysarthria is not unique to adults and can be present at any age following a stroke or head injury or as part of the overall symptoms of cerebral palsy or muscular dystrophy. Depending on the extent and location of nervous system damage, dysarthric speech may be slurred and soft; the speech rate may be labored or present as a more rapid mumbling; speech may be hoarse or breathy with an abnormal intonation; and difficulty swallowing may result in drooling. Clearly when a patient has dysarthria, communication success in the clinic is significantly compromised.
So What Can the Audiologist Do? As with apraxia of speech, to ensure that the patient with dysarthria understands what we are saying will likely take no more accommodation than we would make for any other patient with hearing loss. The larger problem in clinical interactions is to ensure the clinician’s understanding of what the patient is saying. In addition to the suggestions noted for communicating with one who has apraxia of speech which would apply to one with dysarthria as well, we should ensure that the patient is sitting upright in a comfortable position which can improve breath support for better articulation.
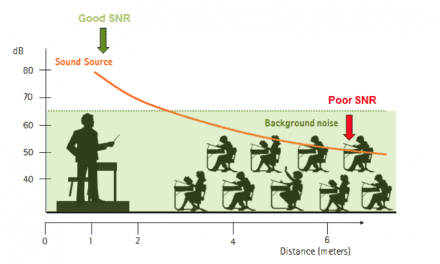
Many of the suggestions to improve our understanding of dysarthric speech (or that of any motor speech disorder) are similar to the suggestions we give to patients with hearing loss. Fortunately, background noise levels and visual distractions are usually at a minimum in a clinical setting; however, watching the patient and increasing attention levels certainly can improve our understanding. And, just as we tell our patients with hearing loss, we need to avoid feigning comprehension and practice asking for the part of the message that was missed or rephrasing what was said. When misunderstanding persists, asking yes/no questions to seek clarification or suggesting patients write their statement may help. As with apraxia, use of a communication board or other AAC when available is important.
Vocal Production Issues
When a person with diminished hearing has a primary communication partner who has diminished capacity for vocal loudness, the couple’s communication difficulties are greatly magnified. Although those with voice pathologies most frequently have been evaluated and treated by a speech-language pathologist, an otolaryngologist, and possibly a neurologist, these professionals may not be aware of, or may not have addressed, the communication breakdowns that occur through a combination of the decreased vocal output of one partner coupled with the decreased hearing of the other.
Vocal cord paralysis arising from either unilateral or bilateral laryngeal nerve damage results in an inability to project the voice or speak loudly accompanied by a hoarseness or breathy voice. Arising from a variety of sources—including trauma, stroke, cancer, tumor, or viral infection—this fairly common condition has clear implications for our patient’s perception of speech as would any vocal abnormality resulting in hoarseness or breathy voice.
In spite of a fairly low incidence, many people are aware of spasmodic dysphonia due to the high profiles of Robert F. Kennedy, Jr. and the (now retired) National Public Radio host, Diane Rehm. Occurring in only one to four people in 100,000, spasmodic dysphonia is a chronic voice disorder in which movement of the vocal cords is forced and strained, resulting in the production of a jerky or quivering voice or a voice that sounds hoarse or tight. Those with spasmodic dysphonia experience interruptions or spasms in which there may be no voice as well as periods when there is a near normal voice.
Laryngeal or hypopharyngeal cancer, which may necessitate a partial or total removal of the larynx, results in partial or total aphonia as the trachea no longer dispels air through the mouth. Research has shown that all three common modes of alaryngeal speech (esophageal speech, tracheal-esophageal puncture speech, and use of an artificial larynx) produce speech signals with enough degradation that audiologic intervention in the form of communication strategies can be beneficial even for spouses with essentially normal hearing (Clark, 1985). Clearly, the difficulties would be even greater when listening to alaryngeal speech when hearing loss is present.
So What Can the Audiologist Do? Communication training, which is beneficial for nearly all with significant hearing loss, becomes an even greater imperative when either the patient or primary communication partner has compromised vocal production. In addition to any hearing aid amplification recommendations that might be given to the patient, discussion of personal voice amplifiers for the one with decreased vocal output will further enhance communication success. Certainly if the patient or communication partner has vocal production issues that have not been evaluated by a speech-language pathologist in the past, a referral for a consultation should be made.
As clinicians, our understanding of the speech of those with vocal production disorders is enhanced by use of all of the communication strategies we might encourage our patients with hearing loss to use.
Aphasias
Arising from damage to portions of the brain responsible for language, aphasia impairs both the expression and the reception of language, both spoken and written. Aphasia may have a sudden onset arising from stroke or a head injury or may be of a more gradual onset secondary to a brain tumor, infection, or the onset of dementia. Patients with aphasia may also have dysarthria or apraxia of speech, both of which also result from brain damage.
Patients with Wernicke’s aphasia resulting from temporal lobe damage may speak in long, meaningless sentences often interjecting unnecessary or made-up words. It can be extremely difficult for others to understand what the person with Wernicke’s aphasia is trying to say. The individual might be unaware of the mistakes made and frequently has great difficulty understanding the speech of others. The damage resulting in Wernicke’s aphasia does not govern motor control, therefore the individual usually has no body weaknesses.
In contrast, Broca’s aphasia arises from damage to the frontal lobe, which is important for motor movement and may produce a right-sided weakness or a paralysis of the arm or leg. Wernicke’s aphasia is classified as a “fluent” aphasia, whereas Broca’s aphasia is classified as “nonfluent,” with those afflicted speaking in short phrases that make sense but may be produced with great effort. Unlike Wernicke’s aphasia, those with Broca’s aphasia may comprehend others’ speech quite well and may be easily frustrated, as they are cognizant of their own difficulties. Global aphasia is another form of nonfluent aphasia arising from more extensive damage to the language centers of the brain and may leave an individual with limited expressive and receptive language.
So What Can the Audiologist Do? When speaking with patients who have any type of aphasia, we should simplify our own language by using shorter and less complicated sentences while speaking slowly and clearly. Important key words should be repeated or written down to help the patient to focus on key concepts. The use of pictures or simple sketches can be similarly beneficial.
We should not speak in the patronizing, over-accommodating speech style known as “elderese” characterized by exaggerated prosody, higher pitch/sing/song voice, and which may be overly directive of overly familiar. Instead, we should maintain a normal conversational style as one would with any adult. We should avoid correcting the person’s speech and encourage any form of expression including gestures and drawing. As with any expressive speech or language problem, a nonrushed conversational manner can facilitate success.
We should encourage and accept any means the patient uses to attempt communication including gestures, pointing, writing, drawing, and vocalizations. It may be both difficult and time consuming for patients with aphasia to find the right word they would like to say. We should schedule accordingly. We should be patient and give them time while not guessing what word they are seeking before asking them if this would be helpful. To aid our own understanding, we should focus on the message and not the production of speech; and as we tell those with hearing loss, we must not feign comprehension, instead asking for a rephrasing or repetition of key phrases that were missed.
Intelligence is not affected with any of the aphasias, but, because the disorder is language based, reading is similarly difficult. Handouts may be helpful for some patients with aphasia but should be clear and concise, and written with short, simple phrases in a larger font with a generous amount of white space. Finally, look back at other communication facilitating suggestions given for apraxia of speech and dysarthria, as these will be helpful when working with patients who have aphasia including use of any available AAC device.
Alzheimer’s Disease
There are several different manifestations of dementia, but Alzheimer’s disease is certainly the most common (Alzheimer’s Association, 2023). First appearing generally after the age of 60, Alzheimer’s is a slowly progressing, irreversible, and eventually fatal brain disorder destroying one’s memory and cognition. Created by an accumulation of beta amyloid plaques and neurofibrillary tangles throughout the brain, Alzheimer’s disease evidences poor transmission of electrochemical signals necessary for information processing and retrieval. Damaged brain tissue eventually suffocates neurons through the inhibition of adequate blood flow.
It is estimated that approximately 33% of the U.S. population over age 85 has Alzheimer’s (Alzheimer’s Association, 2023), which eventually leads to both expressive and receptive aphasia. Memory difficulty is one of the early signs of Alzheimer’s with additional early signs noted by families, including getting lost, difficulty managing money and finances, frequently repeating questions, displaying decreased judgment, difficulty completing what once were common daily tasks, and showing mood or personality changes (National Institute of Aging, n.d.; http://www.alzheimers.gov/).
While the different forms of dementia (Alzheimer’s disease, vascular dementia, Lewy Body Dementia, frontotemporal dementia) may have differences in specific presentation, underlying causes, and progression, they all share problems with memory and cognition which can greatly impact clinical exchanges.
So What Can the Audiologist Do? Audiologists frequently see patients with suspected or “physician-confirmed” dementia. In early stages, these patients can be tested easily through behavioral audiometrics with simple modifications to test procedures. However, the audiologist may need to rely more on physiologic tests for patients in more advanced stages of their disease. Ensuring that confusion is not greater simply because a message was not heard correctly is important for those suffering with dementia. The use of carefully selected and monitored amplification can greatly improve quality of life for many patients with various forms of dementia (Amieva et al., 2015; Lin, et al. 2023; Weinstein & Amsel, 1986).
Third-party involvement in the hearing aid fitting and orientation process is, of course, critical to success. Given the high incidence of Alzheimer’s and other forms of dementia and the low rate of self-reporting of memory loss and confusion, adult patients would be well served if audiologists and other health providers performed screenings of mental status as part of their intake process (Armero, et al., 2017; Beck, Weinstein & Harvey, 2018). This can take the form of a straightforward case history question such as, “Do you or any members of your family have concerns about any possible memory challenges or confusion that you may have?” A follow up question asking about any concerns when the case history question is answered affirmatively can be used to segue into appropriate referral or encouragement to discuss concerns further with the patient’s primary care physician. Direct cognitive screening is within the audiologists’ scope of practice when deemed appropriate (American Academy of Audiology, 2023; American Speech-Language-Hearing Association, 2018). Brief screening tools (the Mini-Mental State Examination [MMSE; Cockrell & Folstein, 2002], the Saint Louis University Mental Status (SLUMS) Examination (Tariq, Tumosa, Chibnall, Perry & Morely, 2006) or the Mini-Cog [Borson, et al. 2000]) can also guide referrals.
Direct communication with a person who has any type of dementia can become increasingly difficult as the disease progresses, but the goal remains to maximize comprehension and participation. While directing statements to the patient, the third party in attendance will benefit from information provided. The audiologist should tell everyone present in the consultation room that questions are encouraged from all parties. Except in quite advanced stages of disease, patient permission should always be sought before directing dialogue to an attending person.
When preparing for the appointment we should review the patient’s history to better understand the type and stage of dementia the patient has and if there are any documented preferences for communication. If possible, an appointment time should be provided when the patient is most alert and rested. When addressing the patient, strive to use familiar vocabulary, using shorter sentences while speaking clearly and slowly. Reduce confusion by not switching between topics and by avoiding jargon. We should check understanding by requesting a brief summary of what was said or by using yes/no questions while recognizing patients may respond “yes” even when they have not fully understood.
When expressive and/or receptive communication is compromised significantly, the presence of an attending significant other is invaluable. Observe how they communicate with the patient and seek their insights on the patient’s usual communication style. Be sure to acknowledge their concerns and encourage their questions. Providing care for one with dementia has its own demands, challenges, and frustrations. We should acknowledge recognition of the importance of this person’s role in the patient’s care.
Conclusion
A variety of disorders impacting expressive and receptive communication can be evidenced in the population, including the population of those who come to the audiology clinic. Other communication disorders that co-exist with a patient’s hearing loss, or that the patient’s communication partner is contending with, can directly impact audiological services. When communication problems in addition to hearing loss are present during an audiology appointment, we should be prepared to modify our services to accommodate patients and their communication partners as fully as possible and to make referrals when necessary.
While this article focuses on a limited number of possible concomitant communication disorders, many of the counseling considerations offered may be applicable to a wider array of disorders which may impact communication. These may include Parkinson’s disease, autism spectrum disorder, amyotrophic lateral sclerosis (ALS, also known as Lou Gehrig’s disease), multiple sclerosis, Huntington’s disease, ischemic and hemorrhagic stroke, traumatic brain injury, and others. Following suggestions for enhancing communication with those who have concomitant communication disorders demonstrates that the patient’s presence and input toward treatment is recognized and appreciated, and serves to support patient autonomy and a sense of self-dignity.
John Greer Clark, PhD, is a professor emeritus at the University of Cincinnati and Kristina M. English,PhD, is a professor emeritus at the University of Akron. Clark and English have just released the fourth edition of their text, Counseling-Infused Audiologic Care (www.audiology-counseling.com), available through Amazon. Author Contact: [email protected]
Featured image: Dreamstime
References
Alzheimer’s Association. (2023). 2023 Alzheimer’s Disease Facts and Figures. https://www.alz.org/alzheimers-dementia/facts-figures
American Academy of Audiology (2023). Scope of practice. https://www.audiology.org/practice-guideline/scope-of-practice/ Accessed April 15, 2025.
American Speech-Language-Hearing Association (n.d.). Making effective communication, a human right, accessible and achievable for all. https://www.asha.org/about/history/?srsltid=AfmBOoqhHC5d5loawBogDjtUiRjJl6ZRPawD3N-Ti-Xg8Em_lkJcAAFR Accessed March 26, 2005.
American Speech‑Language‑Hearing Association. (2018). Scope of practice in audiology [Scope of Practice]. Available from www.asha.org/policy/. Accessed April, 15, 2025.
Amieva, H., Ouvrard, C., Giulioli, C., Meillon, C, Rullier, L., & Dartigues, J.F. (2015). Self-reported hearing loss, hearing aids, and cognitive decline in elderly adults: A 25-year study. Journal of the American Geriatrics Society, 63(10), 2099-2104.
Armero, O, Crosson, S., Kasten, A., Martin, V. & Spandau, C. (2017). Cognitive screening model expands health care delivery. Hearing Journal, 70 (6), 12-13.
Aslan, F., Yücel, E., & Atkins, C. P. (2018). Counseling in audiology: students’ perspectives. Yüksekö¤retim Dergisi, 8(2), 133–139. doi:10.2399/yod.18.005
Beck, D.L., Weinstein, B.E., & Harvey, M. (2018). Dementia Screening: A role for audiologists, Hearing Review. 25(7): 36-39.
Borson, S., Scanlan, J., Brush, M., Vitaliano, P., & Dokmak, A. (2000). The Mini-Cog: A cognitive “vital signs” measure for dementia screening in multi-lingual elderly, International Journal of Geriatric Psychiatry 15, 1021-1027.
Clark, J. G. (1985). Alaryngeal speech intelligibility and the older listener. Journal of Speech and Hearing Disorders, 50, 60-65.
Cockrell, J. R., & Folstein, M. F. (2002). Mini-mental state examination. Principles and practice of geriatric psychiatry, 140-141.
English, K. (2019a). Challenge: Staying patient-centered while taking electronic notes. Solution: Signposting. Accessed 12-9-2024: https://advancingaudcounseling.com/signposting/
Gold, G. & Gold, A. (2021). The experience of speech–language therapists and audiologists when delivering bad news: A qualitative analysis. International Journal of Language & Communication Disorders, 56(2), 402-414.
Hall, J.W. (2025). “Acclaim for Counseling-Infused Audiologic Care, 4th edition” p.v. Inkus Press/Amazon.com.
Hawkins, D.B. (1990) Technology and hearing aids: How does the audiologist fit in? Asha, 32, 42-43.
Lin, F.R., Pike, J.R., Albert, M.S., Arnold, M., Burgard, S., Chisolm, T., Couper, D., Deal, J.A., Goman ,A.M., Glynn, N.W., Gmelin, T., Gravens-Mueller, L., Hayden, K,M,, Huang,A.R., Knopman, D., Mitchell, C.M., Mosley, T. Pankow, .J.S., Reed, .N.S, Sanchez, V., Schrack, J,A, Windham, B.G., Coresh, J. (2023). ACHIEVE Collaborative Research Group. Hearing intervention versus health education control to reduce cognitive decline in older adults with hearing loss in the USA (ACHIEVE): a multicentre, randomised controlled trial. Lancet. 2023 Sep 2;402(10404):786-797. doi: 10.1016/S0140-6736(23)01406-X. Epub 2023 Jul 18. PMID: 37478886; PMCID: PMC10529382.
Manalastas, G., Noble, L. M., Viney, R., & Griffin, A. E. (2020). Patient autonomy in the consultation: How signalling structure can facilitate patient-centred care. Patient Education and Counseling, 103(11), 2269-2279.
Owens, R. E. & Farinella, K.A. (2019). Introduction to communication disorders: A lifespan evidence-based perspective. Boston, MA: Pearson.
Roth, F.P. & Worthington, C.K. (2025). Treatment resource manual for speech-language pathology. San Diego: Plural Publishing, Inc.
Stemple, J.C., Roy, N & Klaben, B.K. (2020). Clinical voice pathology: Theory and management, 5th Ed. San Diego, CA: Plural Publishing.
Tariq, S.H., Tumosa, N., Chibnall, J.T., Perry, M.H., & Morley, J.E. (2006). Comparison of the Saint Louis University Mental Status Examination and the Mini-Mental State Examination for detecting dementia and mild neurocognitive disorder – A pilot study. The American Journal of Geriatric Psychiatry, 14(11), 900-910.
Weinstein, B., & Amsel, L. (1986). Hearing loss and senile dementia in the institutionalized elderly. Clinical Gerontologist, 4, 3-15.
Woodward, E., & Saunders, G. H. (2023). Do UK audiologists feel able to address the hearing, social and emotional needs of their adult patients with hearing loss. International Journal of Audiology, 63(11), 867–874.