There is little to debate about the usefulness of knowing a patient’s thresholds, most comfortable listening level (MCL), and loudness discomfort level (LDL or UCL). Yet, loudness continues to be a major reason for consumer dissatisfaction with hearing aids: in hearing aids less than 1 year old, the current satisfaction rate for making “loud sounds comfortable” is only 44%.1 In spite of all of our advanced digital and compression technology, comfort with loud sounds remains the third most common complaint of hearing aid users.
Here’s what we need to do…
In the event that threshold and supra-threshold abilities are not clearly defined during a hearing aid fitting, it would be an accurate statement to say that no one can determine how to modify all of the electroacoustic parameters available when fitting that hearing instrument. About one-fifth (17%) of dispensing offices do not conduct threshold (speech MCL/UCL) testing on a routine basis and only two-thirds (69%) own a real-ear analyzer.2
Suprathreshold information is designed into the algorithms and the electronics that exist in high-end analog programmable and digital hearing instruments. We know that it is in the best interests of the patient to thoroughly understand and delineate thresholds and suprathresholds.2 As described in countless articles, the determination of hearing thresholds by discrete frequencies alone simply cannot provide the custom fitting process with enough data to establish kneepoints, compression ratios, crossover frequencies, and output with any accuracy.
And, worse, these problems apply to each of the frequency bands that are available for manipulation. We propose that, if you do not have test data to support the modification of a hearing instrument’s electroacoustic response, you should not change that parameter. Consider this to be in the spirit of “if it ain’t broke, don’t fix it.” However, in this case, the unfortunate truth is that it’s difficult to assess whether something is broke or functioning properly unless one takes the time to examine it.
The Need for Determining LDLs
Gain formulae and targets are extremely useful items in the audiological tool-belt; however, gain targets only present one aspect of the electroacoustic fitting. Many times, the rest of the formula is based on normative data, which has been clinically proven to be off by as much as 17 dB. A patient will reject a hearing instrument fitting if you exceed their LDL by even a single decibel! Yet, it would appear that some people—including some manufacturers of today’s digital technology— are encouraging us to believe that you can achieve appropriate gain targets without exceeding each ear’s measured LDL by (even) that 1 dB. While few manufacturers would advocate against taking suprathreshold measurements, their software lulls one into believing that these measurements are superfluous. On the merits of their advanced software features and the brilliant research of people like David Pascoe et al., they become implicated in denying the value of making suprathreshold measurements. (It should be noted that all recent digital hearing instrument clinical studies regarding hearing in noise have involved frequency-specific LDLs entered into the initial fitting of the hearing instrument for each test subject.)
The result? Many patients are not being tested for LDLs! But, as stated earlier, the literature is replete with evidence for the usefulness of data on a patient’s threshold, most comfortable listening level, and LDL. How can this be? Because, in the authors’ opinion, we don’t really know what we are doing with these tests—or worse, why we are doing them. In many cases, we do them because “we always have.”
More often, even when we might guess at what we are doing, we frequently never knew, or have simply forgotten, why we were doing a specific test. The tests have become a rote task. Digital technology no longer requires gain to be directly tied to the output in the instrument’s electroacoustic response. But the “targets” are still unforgiving and will only work if the patient is a perfect example of the statistics upon which the target is based.
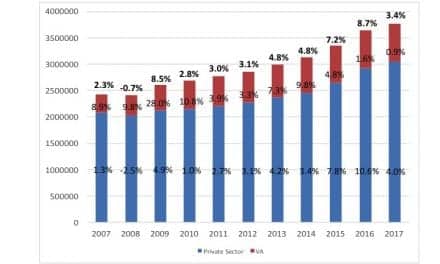
Mueller4 recently added to the body of evidence supporting the necessity for LDL measurements, and the first author of this article has conducted educational seminars detailing methods for suprathreshold measures. Many of our colleagues are now taking those “extra few minutes” to fully define the dimensions of each ear’s residual auditory capacity and dynamic range. In fact, some new age-related normative data is currently being collected by the VA in Portland, Ore, which seeks to identify each ear’s ability to discriminate acoustic signals in noise. This will give us (when combined with existing technology) one more clinical tool to confidently and appropriately recommend directional microphone technology to our patients.
LDL Data and Your Patient
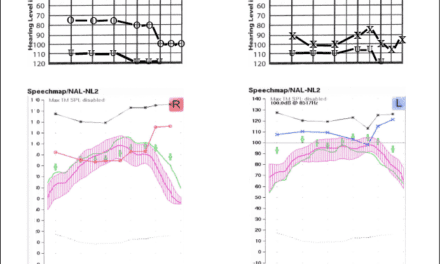
In one of our recent articles,5 we suggested a counseling method for achieving realistic expectations by the patient relative to their residual communication capabilities. In that article, we described a method using a “shaded” audiogram. A “normal hearing box” is diagrammed with horizontal lines drawn at 0 dBHL and 100 dBHL, and attached to vertical lines running from 200 Hz and 6000 Hz. The patient’s frequency-specific SRTs and LDLs are then plotted within this box. The areas between 0 dBHL and the SRT line, and the 100 dBHL and the LDL line, are then shaded. The non-shaded area within the box represents the patient’s residual hearing ability (the hearing that the patient has left and can utilize effectively).
More recently, we have had attendees of our educational seminars draw this shaded audiogram on a sheet of paper. It is important to understand that this “shaded” audiogram can only be accurately described for any patient after supra-threshold test data have been plotted onto it. Many of our colleagues become excited about the visual image created by the shaded audiogram for several reasons:
1. A truly custom picture of each ear’s residual capacity clearly emerges.
2. Appropriate crossover frequency settings, kneepoints, and compression ratios are much easier to see, as well as gain and frequency response.
3. With speech mapping software, a patient immediately becomes aware of their limited capabilities. Therefore, counseling on realistic expectations becomes much easier.
With the new data coming regarding speech-in-noise capabilities, we would encourage the evaluation of the patient’s residual ability in a noisy environment. Current research should soon define normative values for hearing in noise. This will give us a benchmark to use for this ability. It will be similar to the normative data gathered to establish 0 dbHL threshold. We will soon have a benchmark for hearing in noise—and perhaps even age-related data for an even more defined parameter (it is interesting to note that age-related data has not been clinically established for 0 db HL threshold).
It is true that it will take additional time to define your patient’s residual auditory capabilities. If it significantly increases customer satisfaction, we all have that time. In fact, we have whatever time it takes to do this work—correctly—the first time. What we don’t have is the time it would take to do it over.
Working Smarter
We need to fully utilize the incredible digital technology available to us for the benefit of our patients. Sergei Kochkin recently wrote, “A customer is not an audiogram; meeting gain targets does not guarantee that the customer’s quality of life will improve.”5 Taking the extra time at the beginning of your custom fitting will save you and the manufacturer hours of grief later. We tell people who are new to the field that they will spend 60% of their time with 5% of their patients. They don’t quite understand this statement at first, but they soon come to agree.
To deliver the “most” from a hearing instrument requires us to achieve the delivered perception of a “full” sound to the patient. We have never bothered to define just what that sentence means. “Full sound” is a bit like defining the color “yellow.” Our poverty-stricken language allows us only to say, “I can’t define it, but I can point to an example of it when it occurs.” Likewise, we struggle to define what full sound really means to the patient. Defining the patient’s residual auditory capabilities is the key.
In the early days of what was then called “speech and hearing” (now termed “speech-language pathology and audiology”), one of this field’s founders, Charles Van Riper, made a statement that characterizes what we are trying to do with hearing instruments. He said, “A difference, to be a difference, must make a difference.” Relative to loudness, the assessment of LDLs, and the fullness of sound in advanced hearing instruments, that is precisely where we stand at present—either deliberately or by accident. If the patient’s perception is that hearing aids make a significant difference in a variety of situations with minimal side effects, then hearing aids will eventually sell themselves.
In our view, we need to follow the line of questioning posed by Dr. Van Riper concerning our auditory perceptions. And we need to strive for better answers than, “I can’t define it, but I can point to an example of it when it occurs.”


|
References
1. Kochkin S. On the issue of value: Hearing aid benefit, price, satisfaction, and brand repurchase rates. Hearing Review. 2003; 10(2):12-26.
2. Strom KE. The HR 2003 dispenser survey. Hearing Review. 2003; 10(6):22-38.
3. McSpaden JB, Brethower L. Suprathreshold testing: The nuts and bolts of modern fittings. Hearing Review. 2003; 10(11):22.
4. Mueller HG. Fitting test protocols are “more honored in the breach than the observance.” Hear Jour. 2003; 56(10):26.
5. McSpaden JB, Brethower L. Fitting from the other side of the fence. Hearing Review. 2003; 10(7):16-18.
6. Kochkin S. On the issue of value: Hearing aid benefit, price, satisfaction, and brand repurchase rates. Hearing Review. 2003; 10(2):12-26.
Correspondence can be addressed to HR or Jay B. McSpaden, PhD, PO Box 1043, Jefferson, OR 97352; email: [email protected].