Business Development| November 2019 Hearing Review
A differentiation strategy does not occur by accident. This discussion focuses on differentiating a practice with screening for comorbid conditions related to hearing loss, using close and regular monitoring of your patients’ status, and the use of an up-to-date and evidence-based approach to diagnostic assessment.
Recently, a case was made for developing a business strategy based upon detailed competitive intelligence and practice analysis.1,2 In other words, hearing care practice owners need effective methods that consider current and potential global market risks, while reviewing and analyzing the market within their own specific locale. Similarly, Part 1 of this series3 presented some generic competitive strategies that were described by Porter.4 To summarize briefly, some practitioners will attempt a cost leadership strategy, others will focus on specific populations or niche markets, but most will be required to differentiate themselves from the myriad of hearing healthcare practices that, to consumers, all look the same.
Compounding the competitive problem is the false commoditization of hearing aids perpetuated by big box, manufacturer-owned stores, the Internet, insurance companies, and personal sound amplification product (PSAP) companies, as well as the upcoming onslaught of over-the-counter (OTC) hearing devices. Commoditization, which occurs in virtually all successful industries as they mature, happens when consumers feel that they can purchase virtually the same product and/or service from any business anywhere. In this atmosphere, price becomes the only distinguishing factor.
As more and more hearing-impaired patients are convinced there is no significant difference among providers in quality, performance, or service, they will simply shop for the lowest price. In commoditized markets, practices cannot raise prices because consumers shop competitive offerings for what is perceived as the same or similar products at lower prices. If practices are not different—offering value and unexpected positive experiences to their treatment regimen—they will not survive in this environment.
Currently, consumers seem to be expressing that many practices, as well as retailers in general, are on par with an old Chrysler K-Car: presenting old styling, technology, with minimal comfort, convenience, and performance. An appropriate differentiation strategy takes that old K-Car orientation and turns it into a sportscar of unexpected experiences with high performance and technology (Figure 1).

Figure 1. The Tesla (above) offers significant differentiation from rival models and is generations removed from the old Chysler K-car in terms of efficiency, functionality, and performance. Can we say the same about our audiometric testing methods and objectives?
A differentiation strategy does not occur by accident. It is based upon intelligence gathered from the market that is used to develop an introspective analysis and possible reorganization of current goals and objectives allowing this practice to stand out in the marketplace. Differentiation creates that unexpected, “clued-in,” state-of-the-art experience for patients.5
One of many components of a new differentiation strategy reconsiders how hearing healthcare providers practice. At a special session during the 2019 American Academy of Audiology convention, Windmill et al6 proposed two distinct changes in the approach to each new patient:
1) History taking should extend beyond a patient’s hearing loss to include a review of comorbidities—diseases and medical conditions that may occur and possibly interact with hearing loss and related disorders, such as tinnitus and vestibular/balance problems.7
2) The field of audiology might be wise to re-evaluate and update the diagnostic hearing evaluation with a combination of behavioral and objective auditory tests selected specifically to provide maximum diagnostic value while minimizing test time.8
Hall states that hearing healthcare providers “must move beyond product focused evaluations and provide a full scope of diagnostic, management, treatment, and preventative services for Medicare beneficiaries.” 9
Evaluation of Comorbidities
Most of our patients who are 60 years and older are at considerable risk for one or more comorbidities that occur simultaneous with their hearing impairment. These disorders are frequently observed in hearing healthcare practices. However, in most clinics, the diseases and disorders are simply noted in the patient record. The implications of the comorbid conditions for hearing are not further considered, and the patients are not monitored to document the relationship to auditory status.
Windmill and colleagues6,10 documented a rather surprising number of comorbidities that should be taken into account in patients with hearing loss and/or tinnitus (Figure 2). These are common medical conditions noted each day in patient histories, but we typically do not monitor them, as their diagnosis and management is outside of our scope of practice.

Figure 2. Co-morbidity conditions routinely seen by hearing care professionals. From Windmill et al, 2019.6
In fact, it is well within the scope of practice of hearing healthcare providers to identify which conditions might be associated with auditory dysfunction and to make referrals to the appropriate physicians and other health professionals when concerns are noted. For example, Windmill et al6 specifically noted that almost 65% of our patients experience hypertension, 55% have hyperlipidemia or high cholesterol, and over 25% have rheumatoid arthritis, ischemic heart disease, and/or diabetes (see Figure 2).
It is reasonable and good clinical policy to screen via patient history or perhaps using more formal approaches for these and other comorbid conditions, such as kidney disease, depression, and dementia. Adding comorbidity screening differentiates a practice and simultaneously establishes the clinic as a monitoring resource for other healthcare providers.
Although the screening for comorbidities adds some extra time for the office visit, it provides a significant benefit to patients and referral sources while also contributing to a truly different patient experience. An additional important benefit is the development of closer and more productive working relationships with local physicians who are more likely to refer their hearing-impaired patients with comorbid conditions.
Changing Best Practices in Audiology Diagnostics
Most practices are overdue for an update or “makeover” in the approach taken for diagnostic hearing evaluation. Currently, the majority of providers merely conduct the traditional “basic comprehensive, 92557” hearing assessment that was first introduced back in the 1940s. At the time, hearing assessment with air and bone conduction pure-tone testing, and simple speech recognition tests was state-of-the-art. Given the knowledge, technology, and equipment of the time and the brilliance of audiology forefathers like Harvey Fletcher, Ira Hirsh, and Raymond Carhart, these “air, bone, and speech” measures were scientifically proven to provide the best available audiological assessment. However, these basic tests do not offer as much clinically useful information about hearing loss as in combination with more recently developed techniques. Yet, based on Medicare billing data,6 almost all hearing healthcare providers conduct only pure-tone air and bone conduction audiometry, while less than 20% regularly perform acoustic reflex or otoacoustic emissions (OAE) measurements.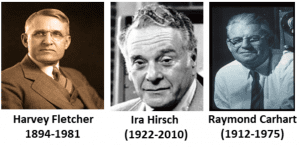
A question that could be asked by consumers (if they knew) could be, “Why are you still testing me with techniques as old as a Buck Rogers movie?” (Figure 3). It could be argued that, while still useful, these old tests have more in common with a Buck Rogers spaceship than a 21st-century flight to Mars. The archaic basic comprehensive battery of tests offers relatively little diagnostic information and only provides an incomplete glimpse at what could really be happening within the auditory system. Further, traditional air-bone-speech testing doesn’t indicate the site of dysfunction within the auditory system and provides no information about hearing and hearing aid performance in noise.

Figure 3. Our basic comprehensive battery of audology tests were created primarily in the 1930-40s, about the same time as the creation of Buck Rogers.
A more efficient, effective, and evidence-based approach to diagnostic hearing assessment should include the routine application of objective auditory techniques like tympanometry, acoustic reflexes, distortion product otoacoustic emissions, plus measurement of speech perception in quiet and noise. Of course, test time would be increased considerably if these procedures were added to the typical comprehensive basic hearing assessment. But we also know that certain traditional hearing tests, such as bone conduction/pure-tone audiometry and speech reception threshold, do not always add value. In practical terms, these traditional tests need not be performed with all patients but, rather, only when they are likely to provide useful information (note: state and/or other entities may mandate them).8
For example, there is little or no diagnostic value for bone conduction pure tone audiometry in a patient who has no history of middle ear disease in combination with normal tympanometry,11 normal acoustic reflexes, and normal DPOAE findings for low frequency stimuli.12 Each of these latter objective tests is much more likely to detect a problem with middle-ear function than a gap between air versus bone conduction hearing thresholds.
Speech-in-Noise Testing
Speech perception in noise should be addressed separately because it is so important for the assessment of older patients complaining of communication problems. Evidence and advocacy for speech-in-noise testing has been present for many years,13-16and is now reaching a point of consensus.17 Communication in the presence of background noise remains one of the thorniest and most persistent problems in hearing aid fitting. According to Taylor,13-15 there are many good reasons why speech-in-noise testing can be beneficial when used routinely in the clinic:
- Speech-in-noise tests can directly address the most common complaint of patients: the inability to hear well in background noise.
- Since it is the common complaint for all age ranges, the results of speech-in-noise tests provide valuable insight into the most appropriate amplification strategy.
- The results of these tests may indicate clearly a patient needs directional microphones, stronger noise reduction programming, extra signal processing to manage background noise—or that they are, in fact, doing so well that we need not emphasize these technologies.
- It offers clinicians more precision in the methods used to counsel patients about realistic expectations.
Amplification options such as hearing aids, cochlear implants, and assistive listening devices do improve hearing abilities, but most hearing-impaired listeners still find it difficult to understand conversation in background noise.18 Taylor13 notes that, despite our best efforts, many patients still cannot hear well in noise even when fitted with hearing devices. Sentence-type speech-in-noise tests will identify these patients during the initial diagnostic evaluation. Once they are identified they can be counseled on what type of hearing aid technology is most appropriate for their hearing impairment. Simply stated, measurement of signal-to-noise ratio (SNR) loss should be part of the routine diagnostic battery. The information it provides is essential throughout the entire hearing aid selection, fitting, and verification process.
By routinely using speech-in-noise tests, a dispensing professional can effectively counsel patients about what can be realistically expected of their hearing aids. Patients with speech-in-noise difficulties may be ideal candidates for aural rehabilitation and should also consider array microphones or FM systems. Such patients will appreciate a candid assessment of their communication problems and knowledge of the limited benefits they can receive from hearing aids when in noisy environments.
Conclusions
There are many ways you can differentiate your practice from the competition in the current era of hearing healthcare. This discussion has focused on differentiating a practice with screening for comorbid conditions related to hearing loss, using close and regular monitoring of your patients’ status, and the use of an up-to-date and evidence-based approach to diagnostic assessment. Each of these strategies for practice differentiation are likely to yield dividends in practice reputation and revenue. Most importantly, however, these strategies will enhance the diagnostic accuracy of your hearing assessments and the effectiveness of management to improve patient outcome.
Robert (Bob) Traynor, EdD, MBA, FNAP, is an audiologist and former private practice owner, and has recently established Robert Traynor Audiology, LLC, based in Fort Collins, Colo, a consulting and expert witness firm. Dr Traynor and Robert G. Glaser, PhD, have recently published the 3rd edition of their book, Strategic Practice Management (Plural Publishing, 2018). James (Jay) Hall, III, PhD, is an internationally recognized audiologist who has held clinical and academic audiology positions at major medical centers, and has served in leadership roles in the American Academy of Audiology. Dr Hall is the recipient of numerous professional awards and the author of over 190 peer-reviewed publications, invited articles, book chapters, and 10 textbooks. He currently holds several part-time and adjunct academic appointments in the USA and abroad, and serves as Chair of the Board of Directors of the Accreditation Commission for Audiology Education (ACAE).
Correspondence can be addressed to Dr Traynor at: [email protected]
Citation for this article: Traynor R, Hall III J. Competing in the new era of hearing healthcare Part 2: Differentiating a practice with comorbidity screening, monitoring, and diagnostics. Hearing Review. 2019;26(11):16-19.
References
1. Traynor RM. Survival strategies in a competitive hearing healthcare market: Part I. Hearing Review. 2018;25(6):14-19.
2. Traynor RM. Survival strategies in a competitive hearing healthcare market: Part II. Hearing Review. 2018;25(8):14-18.
3. Traynor RM. Competing in the new era of hearing healthcare: Part 1: Developing a sound competitive strategy. Hearing Review. 2019;26(9):20-23.
4. Porter ME. On Competition, Updated and Expanded Edition. 2nd ed. Brighton, MA: Harvard Business Review Press;2008.
5. Traynor RM. Are you “clued-in” to offer the ultimate patient experience? Hearing Review. 2019;26(7):25-27.
6. Windmill I, Freeman J, Hall III J, Freeman B. Audiology and Medicare: Where economic reality collides with hearing care. Paper presented at: American Academy of Audiology (AAA) 2019 Convention; March 27-30, 2019; Columbus, OH. https://www.eaudiology.org/products/aaa-2019-audiology-and-medicare-where-economic-reality-collides-with-hearing-care-03-tier-1aaa-ceus.
7. Hall JW III. ACAE Corner: Comorbid conditions associated with hearing loss: Another challenge in educating AuD students. Audiology Today. 2019(May/June). https://www.audiology.org/audiology-today-mayjune-2019/acae-corner-comorbid-conditions-associated-hearing-loss-another.
8. Hall JW III. Rethinking your diagnostic audiology battery: Using value added tests. AudiologyOnline. September 18, 2017. https://www.audiologyonline.com/articles/rethinking-your-diagnostic-audiology-battery-20463.
9. Hall JW III. Rethinking best practices. Paper presented at: American Academy of Audiology (AAA) 2019 Convention; March 27-30, 2019; Columbus, OH.
10. Windmill IM, Freeman BA. Medicare, hearing care, and audiology: Data-driven perspectives. Audiology Today. 2019. https://www.audiology.org/audiology-today-marchapril-2019/medicare-hearing-care-and-audiology-data-driven-perspectives.
11. McSpaden JB. Basic tympanometry in the dispensing office. Hearing Review. 2006;13(12):16-28.
12. Dhar S, Hall, JW III. Otoacoustic Emissions: Principles, Procedures, and Protocols. 2nd ed. San Diego,CA:Plural Publishing;2018.
13. Taylor B. Speech-in-noise tests: How and why to include them in your basic test battery. Hearing Review. 2003;56(1).
14. Taylor B. Using speech-in-noise tests to make better hearing aid selection decisions. AudiologyOnline. April 25, 2011. https://www.audiologyonline.com/articles/using-speech-in-noise-tests-832.
15. Taylor B. Consultative Selling Skills for Audiologists. 2nd ed. San Diego, CA: Plural Publishing;2012.
16. Beck DL, Nilsson M. Speech-in-noise testing: A pragmatic addendum to hearing aid fittings. Hearing Review. 2013;20(5):24-26.
17. Beck DL, Danhauer JL, Abrams HB, et al. Audiologic considerations for people with normal hearing sensitivity yet hearing difficulty and/or speech-in-noise problems.Why do so many people with “normal hearing” report that they have hearing problems? Hearing Review. 2018;25(10)[Oct]:28-38.
18. Smits C, Goverts ST, Festen JM. The digits-in-noise test: Assessing auditory speech recognition abilities in noise. J Acoust Soc Am. 2013;133(3):1693.







