Why we need evidence-based practices and why all managers should adopt best-practices guidelines
The key principle underlying all patient experiences, and ultimately what drives customer satisfaction, results from the interaction of two factors:
1) The evidence-based processes imposed by management;
2) The personal interaction that takes place between the patient and the professional.
A motivated patient arrives at your clinic. The fact is that any hearing aid—even one that is not professionally fitted using a rigorous protocol—is better for him than no hearing aid at all. Is it for this reason, as an industry, we remain complacent when it comes to issues of quality practice standards?
The aim of this article is to show how the service-oriented professional executing proven clinical protocols drives long-term patient loyalty, and what one organization is doing to raise the standards of service and professionalism within its own ranks. As our industry tries to meet the ever-demanding needs of today’s savvy consumer, it is ultimately the quality of the professional, and the services and experience they provide—not technology, better retail prices, or more efficient distribution—that will bring more patients to our doors.
Are Modern Hearing Aids a Commodity?
It is tempting to think that all of the advanced features found in modern hearing aids, along with their automated fitting algorithms, would be enough to improve user benefit and satisfaction. The breathtaking pace of changes in hearing aid technology is quickly leveling the playing field. All of us have ready access to high-quality digital hearing aids at a number of price points.
|
| TABLE 1. A random comparison of four leading manufacturers’ high-end products using universal terms to define each advanced feature. |
A random comparison of the available features in four of the leading manufacturers’ high-end products shows that there is very little difference across similar technology tiers (Table 1). Although there are indeed differences in the way each manufacturer’s compression, digital noise reduction, and other advanced features work, to date, there is no peer-reviewed study showing a clear preference for one manufacturer’s advanced features over another’s. In fact, there is limited real-world evidence indicating many of these advanced features are beneficial to patients in everyday listening situations.
Although hearing aid technology has clearly improved, the true difference is in how the hearing aid technology is selected and adjusted to meet the individual needs of each patient. This statement is based on numerous studies showing that both linear and WDRC processing result in high patient outcomes when each type of hearing solution is properly fitted using an established fitting protocol.1,2
Do We Need to Raise the Bar on Quality?
A review of key business indicators would confirm the above. Historically, return for credit rates as measured by manufacturers have hovered around 20% to 25%. The number of hearing aids ending up in the dresser drawer continues to be at 15% to 18%. The number of patients who shop around or decide not to buy hearing aids when it is time to repurchase is over 50%.3 Although recent reports of overall satisfaction have increased, the number of dissatisfied patients has not changed over the past several years.4
There have been many efforts to implement more rigorous clinical standards in dispensing practices. Nearly every decade brings another round of recommended clinical protocols. In 1946, Raymond Carhart published a 12-step fitting protocol based on his work at Deshon General Hospital. ASHA published it’s first “Minimum Requirements for Clinics Evaluating Hearing Aids” in 1952, and followed up by publishing a 70-page monograph on clinical fitting protocols in 1970. In 1981, the Vanderbilt Working Conference addressed the need for a protocol, and in 1994, the Independent Hearing Aid Fitting Forum (IHAFF) published a series of guidelines. Last year, the International Hearing Society published a list of recommended guidelines for the dispensing of hearing instruments. Currently, the American Academy of Audiology (AAA) is about to publish a evidence-based set of fitting guidelines. All these guidelines are well-written documents with a considerable amount of research behind them; the one common theme throughout all of them is very few field professionals consistently execute them.
These efforts to establish a more rigorous protocol are not without merit. There is significant evidence gathered from experienced hearing aid users showing professionals who utilize a systematic clinical protocol in their own practice reap its rewards through higher-than-average patient satisfaction scores.3 It also seems apparent that executing a protocol brings a higher level of uniformity and standardization within an organization. Still the question remains: Why do so few field professionals execute them on a consistent basis?
The Value of Using Evidence-Based Principles
One favorable trend in the hearing care industry is the emergence of evidence-based principles (EBP) into the clinical decision-making process. In short, evidence-based principles is a process by which hearing care professionals make treatment decisions based on the best available evidence. Evidence is classified along a six-level hierarchy in which meta-analysis of randomized controlled clinical trials represent the highest or best level of evidence. EBP requires clinicians to rigorously review and analyze research, and act (or not act) upon the findings when making important clinical decisions. Over the past year, EBP has gained favor as the preferred method for making clinical decisions, and two issues of the Journal of the American Academy of Audiology have been devoted to it. There remains, however, a considerable gap between what the evidence suggests we do, and what actually happens when it comes to dispensing hearing aids.
One example of this disconnect is the use of speech audiometry measures in the hearing aid selection and fitting process. According to recent surveys,6,7 over 90% of all dispensing professionals rely on some type of speech audiometry when making important clinical decisions. With so many professionals relying on a certain procedure, one would think that speech audiometry effectively predicts real-world hearing aid satisfaction and benefit. A review of the evidence, however, shows otherwise; there is a weak relationship between speech audiometry scores and real-world hearing aid benefit.8
But Are Evidence-based Principles Enough?
Following a more rigorous protocol and incorporating EBP into your own routine certainly allows you to make better clinical decisions. The question is, does following an evidence-based protocol address the needs of a savvier consumer?

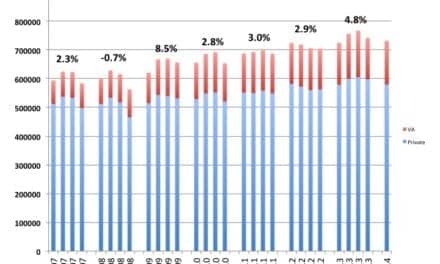
|
| FIGURE 1. Top 12 most important attributes for experienced hearing aid users. |
Recent market research shows what hearing aid users are looking for when making a purchasing decision (Hearing Segmentation Study, Amplifon USA, March 2006). The data in Figure 1 suggests that 6 of the top 12 most important attributes are directly related to the clinical and interpersonal skills of the professional. Also, notice that most of these attributes—particularly trust, reputation, and ability to listen—are directly related to interpersonal ability.
The key principle underlying all patient experiences—and ultimately what drives customer satisfaction—results from the interaction of two factors:
1. The evidence-based processes imposed by management, and
2. The personal interaction that takes place between the patient and the professional.
As practice owners or managers, it is important to embrace both factors in order to meet the rising expectations of today’s patient. One of the largest providers of hearing health services recognizes there is a gap between what is known to work best, and what is actually done in the field, and is trying to improve the way their services are delivered by raising the performance bar for its field professionals.
Instituting a Certification Process
In the best interest of the consumers who rely on our products and services, both hearing instrument specialists and audiologists employed by Sonus are expected to become “Sonus Certified.” The purpose of the certification process is to ensure patients are receiving the best possible care while balancing the long-term business needs of their clinic.

|
| FIGURE 2. The non-negotiable minimum procedures at the pre-fitting and fitting appointments. |

|
| FIGURE 3. The non-negotiable minimum standards during the post-fitting and subsequent follow up appointments. |
The most important aspect of the certification process is the execution of several proven clinical procedures, most of which are supported by evidence. The procedures for four segments of the patient experience are listed in Figures 2 and 3. Providers who have attended several mandatory hours of training and undergone a chart review process are expected to execute these steps.
Best Practices Guidelines: What Do You Want to be Known For?
Hearing health care professionals have unprecedented access to enormous amounts of data on the latest scientific findings that can be extremely helpful when making important clinical decisions. But in reality, most professionals tend to rely on their own experiences and those of their colleagues when making decisions. Once a procedure or test takes root, no matter how antiquated it has become, it is difficult to dislodge. Even the emergence of new and improved practice guidelines seem to have little impact on what procedures are actually conducted in the clinic. Because the majority of professionals are slow to change, forward-thinking organizations and practitioners need to lead the way. Most professionals want to feel good about their work, get compensated for it fairly, and work for an organization they can be proud of. Using EBP to hone a best-practices protocol, along with a caring bedside manner, allows any service-oriented business to set it’s self apart from the competition.
In any world-class organization, managers need to hold field professionals accountable for upholding the values of the organization. In turn, field professionals need to act with integrity and in the patient’s best interest. A quality assurance process can be the key driver of long-term patient satisfaction for an organization willing to embrace a culture of self-improvement and hold it’s professionals accountable.

|
References
1. Humes LE. Modeling and predicting hearing aid outcome. Trends Amplif. 2003;7(2):41-75.
2. Larson VD, et al. Efficacy of 3 commonly used hearing aid circuits: a crossover trial. JAMA. 2000;284(14):1806-1813.
3. Kochkin S. On the issue of value: Hearing aid benefit, price, satisfaction, and brand repurchase rates. The Hearing Review. 2003;10(2):12-25.
4. Kochkin S. MarkeTrak VII: Hearing loss population tops 31 million. The Hearing Review. 2005;12(7):16-29.
5. Cox RM. Evidence-based practice in provision of amplification. J Am Acad Audiol. 2005;16(7):419-438.
6. Kirkwood D. When it comes to hearing aids, “more” was the story in ’04. Hear Jour. 2005;58(5):28-37.
7. Strom KE. The HR 2005 dispenser survey. The Hearing Review. 2005;12(6):31.
8. Killion MC, Gudmundsen GI. Fitting hearing aids using clinical prefitting speech measures: An evidence-based review. J Am Acad Audiol. 2005;16(7):439-447.
Correspondence can be addressed to HR or Brian Taylor, Amplifon USA, 5000 Cheshire Lane, Plymouth, MN 55446; e-mail: [email protected].