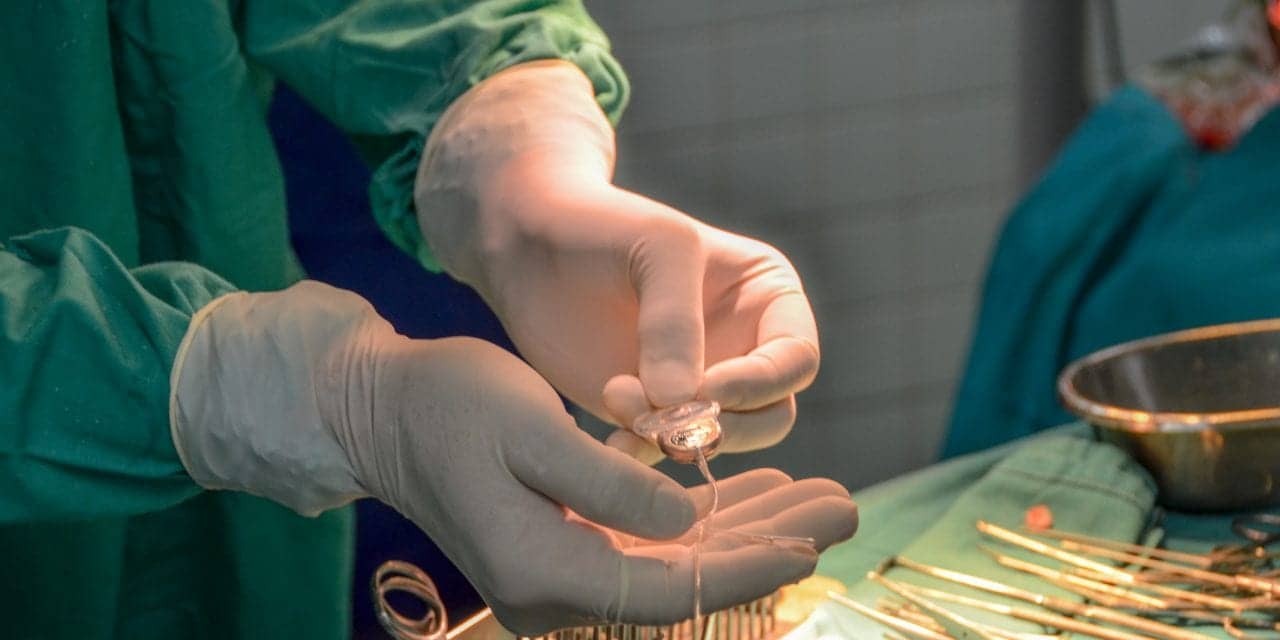
From the impact of COVID-19 on parents, to speech differences between English- and Spanish-learners, and advanced ear surgery techniques, University of Miami Miller School of Medicine hearing professionals presented their latest studies at CI2021, the annual conference of the American Cochlear Implant (ACI) Alliance, from April 28 to May 1, according to an announcement posted on the Newswise website.
Related article: NIH Grant Supports New Cochlear Implant Technique
“Despite the challenges of the past year, the ACI Alliance has pushed forward with new initiatives, research grants, and advocacy opportunities,” said Meredith Holcomb, AuD, director of the Hearing Implant Program in the Department of Otolaryngology, and chair of the ACI Alliance Board of Directors. “Telehealth has allowed us to stay connected to our patients, while creating new opportunities for international training and education.”
Holcomb hosted the four-day virtual conference, themed “Cochlear Implantation: It Takes a Village,” which reportedly drew more than 1,300 attendees from around the world, according to the announcement. It featured a keynote address by US Congresswoman Debbie Dingell (D-Michigan) on the importance of expanding Medicare coverage to include hearing aids for older adults.
Impact of COVID-19
Several UM presentations focused on the impact of COVID-19 on children with hearing loss and their families, including the first study focused on parental mental health and functioning. Ivette Cejas, PhD, associate professor and director of family support services for the Children’s Hearing Program at the University of Miami Ear Institute, presented “Impact and exposure of COVID-19 in Parents of Children with Hearing Loss: Relationship with Mental Health and PTSD,” which received a conference presentation award.
In a survey of 103 families receiving services from the UHealth clinic, Cejas found that parents reported higher levels of stress, including difficulties with sleeping, eating, and mood disorders. However, only 7% were receiving mental health services for these caregiving-related issues.
“This study highlighted the increased need to incorporate mental health screening and treatment particularly for families of children with chronic or developmental conditions,” said Cejas. “As the world continues to identify the post-pandemic effects of COVID-19, pediatric programs need to ensure that family support services are available, including psychology and social work, due to the established relationship between parental mental health and pediatric outcomes.”
In a separate talk, “Parenting in a Pandemic: Associations Between Parenting Strategies and Stress,” Jennifer Coto, PhD, postdoctoral associate, discussed how parents could better address these stressful situations. “We found that parents who took a positive approach when helping children with hearing losses reported less distress than those who did not,” she said. “While cochlear implant clinicians usually focus on the child, we need to be sure that family-centered care is a priority in managing hearing loss.”
Speech outcomes in bilingual patients
Sandra Velandia, AuD, assistant professor and director of clinical operations in the Division of Audiology, gave one of the conference’s most intriguing presentations, “Speech Outcomes in Bilingual Cochlear Implant Patients Using English and Spanish Tests.”
In reviewing speech outcomes over time for 512 UM patients between 2014 and 2018, Velandia found that Spanish speakers fitted with cochlear implants scored higher than English speakers on some measures. “Our study raises a number of questions,” she said. “Are there differences in the languages? Are the Spanish testing materials too easy? We need to understand why when deciding which language to use for testing.”
Another UHealth study looked at the differences between subjective and objective cochlear implant programming methods. In her talk on “Electrical Stapedial Reflex Thresholds in Cochlear Implant Programming and Effects on Speech Perception in Noise,” Diane Martinez, AuD, assistant professor of audiology, found that objective programming may improve speech understanding in noisy settings and may be beneficial for a number of patients.
Other Miller School students and faculty had presentations or posters at the ACI Alliance conference, including the following:
- “Acetylcysteine and Dexamethasone in Combination Provides Otoprotection in a Preclinical Guinea Pig Model of Cochlear Implantation,” by Adrien Eshraghi, MD, MSc, professor of otolaryngology, neurological surgery and biomedical engineering; co-director of the UM Ear Institute; and director of the University of Miami Hearing Research Laboratory.
- “Hearing in Noise: Benefits of FM vs. RM in Children Using Bone Conduction Devices,” by Chrisanda Sanchez, AuD, assistant professor of audiology.
- “Using Clinical Audiologic Measures to Determine Cochlear Implant Candidacy,” by Priyanka Reddy, a trainee in the Department of Otolaryngology (in collaboration with the Medical University of South Carolina).
- “The New Normal in Education: What Parents Had to Say,” by Alexandria Mestres, patient education coordinator.
- “The Effects of Aging on Binaural Hearing in Bilaterally Implanted Adults,” by Molly Smeal, AuD, clinical and research audiologist.
- “Challenges and Considerations with Cochlear Implantations in Patients with Malformed Inner Ear Anatomy: A Systematic Review,” by Jenna Bergman, a medical student who works in Dr Eshragi’s hearing research lab.
- “Speech Outcomes After Cochlear Implantation in Patients with and without Asymmetric Hearing Loss,” by Carly Misztal, MD, Class of 2021.
Ann Geers, PhD, from the University of Texas at Dallas, and Richard Miyamoto, MD, of the Indiana University School of Medicine, received lifetime achievement awards from the ACI Alliance, and Konstantina Stankovic, MD, PhD, of Harvard University Medical School, delivered the keynote lecture, “Degeneration and Regeneration of the Inner Ear.”
The ACI Alliance conference program committee included Sandra Prentiss, PhD, associate professor of clinical audiology, and Cejas. Serving as ACI Alliance board members were Holcomb and Fred Telischi MD, chair of otolaryngology, professor of otolaryngology, neurological surgery, and biomedical engineering, and the James R. Chandler Chair in Otolaryngology. Smeal, Cejas, Prentiss, and Tina Stern, AuD, assistant professor of clinical audiology, are ACI Alliance state champions.
Source: University of Miami Miller School of Medicine