Tech Topic | June 2021 Hearing Review
By Robert M. Traynor, EdD, MBA
From a practice management and marketing standpoint, 3D-scanning technology has become a no-brainer in terms of convenience, patient comfort, risk and liability, and product quality—truly differentiating premier clinics from those still operating with 20th-century procedures.
Most seasoned hearing healthcare clinicians have seen major procedure changes during their careers. The advent of procedures, such as probe microphone measures, speech-in-noise testing, immittance audiometry, otoacoustic emissions, auditory brainstem response, and the use of state-of-the-art hearing products have all drastically changed practice patterns over the past 30 years. One area of practice that has not changed much is that of obtaining ear impressions. While most clinicians have said “goodbye” to the use of powder and liquid material in favor of silicone and impression guns, they are still mired in 1980’s technology. Although most feel this is the “Best Practice,” there are still major errors and injuries that occur with these outdated procedures, especially for deep canal impressions.
Why Change Impression Technique?
Problems with the traditional technique. There are few published reports of ear impression difficulties and injuries in the literature, but seasoned clinicians have seen significant issues using the silicone impression material with their patients in their own clinics. Wynn et al1 states that when taking an impression of the external ear canal and ear, the audiologist is engaged in an invasive procedure whereby a foreign body is first placed into the ear canal and then removed.
There is always an element of risk for significant medical problems when a clinician is performing an invasive procedure. Beyer and Younkers,2 among others, present that the taking of ear impressions is, by far, the riskiest procedure that audiologists perform. Clinicians must be diligent with ear impressions, as it is an invasive procedure filled with unforeseen problems. In the typical procedure, the ear canal must be conscientiously inspected for debris and other contraindications, as well as confirming the placement of the otoblock to avoid damage to the ear canal or tympanic membrane. For deep canal impressions there is potential for damage to outer, middle, and even inner ear structures.
Even in skilled hands, complications of traditional ear impression techniques may include abrasions, trauma, or lesions to the tympanic membrane, middle-ear ossicles, the removal of a pressure equalization (PE) tube, perilymph fistula with resultant fluctuating progressive or long-standing sensorineural hearing loss, or concussive inner-ear trauma accompanied by temporary or permanent threshold shifts. Additionally, there may be hidden mastoid cavities that can create serious medical issues when filled with impression material.
The legal risks. These injury issues have put clinics in jeopardy since the beginning of hearing care, but especially since 1981 with the advent of silicone material and the use of manual and motorized impression guns. The legal risk to the practitioner is the financial or reputational loss that can result from any of the injuries that may be created by traditional ear impression techniques. As hearing care has become more obvious to consumers, malpractice suits are becoming more common. This can be seen in the rising costs of malpractice insurance for hearing healthcare over the past few years. Malpractice insurance often covers the legal expenses and the eventual settlement, but there is then the case of malpractice insurance premium increases and/or the concern for the insurability of the practitioner. This loss of malpractice insurance makes it almost impossible to obtain licensure and, therefore practice, in most states.
Of course, the outcome of these cases is usually mediated and a fair and just settlement is achieved by the court. When the practitioner meets with their attorney to determine the likelihood that they may lose the malpractice case, it is, of course, too late to consider risk management. Prior to litigation becoming a problem, practitioners need to review potential risk of traditional ear impression procedures compared to scanning the ear as a method of avoiding possible legal action for errors.
As one owner of a large dispensing network stated, “…As a practice owner and manager, I’m very reluctant to ask someone to do a procedure they’re uncomfortable with due to liability issues. Blow-by [silicone material moving around an improperly placed otoblock] may be rare, but we all know that it can and does happen.”3
Scanning Devices Reduce the Risk of Litigation
The use of lasers for 3D imaging has been used by other industries for many years, but only recently has this technology been researched and applied to the replication of the intricacies of the ear. Ear scanning devices such as Otoscan by Natus and Lantos instrumentation use 3D-laser mapping techniques to construct an exact digital image of the ear canal. Just as dentists scan the mouth for dentures, crowns, and other procedures, hearing care now has the capability to reduce the possible legal risk factors caused by the uncertainty of silicone ear impressions by simply scanning the ear canal and ear.
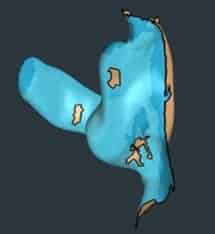
The Otoscan ear scanner (Figure 1) produces pulses of laser light and measures the reflections of this light to establish the distance travelled. It is a similar technique to sonar used by the Navy to detect mines and aid in navigation. Using software, the scanner compiles millions of data points to replicate the shape of the ear to construct the image. The more complete the scan, the more accurate the representation.

In the Otoscan software, the scanned area of the ear (Figures 2 and 3) often changes color as the scan moves around the ear canal. The entire process takes 2-3 minutes. There is no otoblock, no mixing, squirting, or mess—and, therefore, no chance of creating injuries to the patient as might be the case with a traditional impression.

To make the process more efficient, the scanners have three modes of operation:
- Ear canal. Scanning the ear canal is the first component of the process. When inside the ear canal, scanners use a ring laser to focus more light to the side rather than to the front to rapidly map the ear canal walls.
- Flat surfaces. For the outer ear and pinna, the scanner uses a broader front- facing signal that captures the entire shape of this flatter area.
- Curved surfaces. The antihelix and triangular fossa are scanned by the ring laser technology to gather the finer details of this broad area. After completing all three stages, the scan should be complete. The image is then saved and may be uploaded for safe storage at a remote server where the scans are stored (Figure 3).
While a scanner is likely a major differentiator for a hearing care practice, it is much more than a way to take ear impressions. Scanning becomes a method of storing ear scans for later use to fabricate custom earplugs, earmolds, remakes, or a second set of custom hearing aids.
Scanner Costs
Scanner cost is often a concern for the private practice owner that must be justified. However, differentiation of the practice in today’s competitive climate is essential.4 Initially, the scanner will be a differentiator, used to demonstrate a premium practice from others within the community.
After some time, when scanners are in use everywhere, using a traditional ear impression technique will not be best practice. Not using a scanner will reduce the patient’s impression of the skills and capabilities of the hearing care professional. In addition to the marketing capabilities, there are other benefits to scanning:
- High technology. The use of a scanner can be part of the equipment budget that ensures the clinic offers innovative, state-of-the-art capabilities.
- Patient comfort. There is no discomfort from otoblock placement or the ear being plugged during the setup of the impression. Scanning is simple and takes 2-3 minutes for completion.
- Greater sales. A scan for every patient means that when other products are required, the scan is already available, saving patients trips to the clinic and the provider spending time seeing them. Think about the benefits of having the digital scans for snowbirds who leave colder climates for warmer ones for extended periods of time.
- Better fit and fewer remakes and returns. As the manufacturers improve their ability to create products from a digital scan, the fit and comfort will become optimized. Fittings will realize less retention problems and/or occlusion issues with scans as they are more accurate. Consider the number of times earmolds or hearing aids are remade or returned due to fitting issues. The time and material, shipping costs, refitting, and reprogramming that can be saved allows the clinician to concentrate on other revenue producing activities.
Moreover, when a procedure causes an injury, legal action is often taken to seek justice for the injured person. Hearing care malpractice cases are increasing, as many more patients become familiar with hearing care. The newest generation of patients are better educated and are more likely to take legal action for issues. Considering the legal risk of traditional silicone ear impressions, the possible costs of malpractice, and even a professional’s career, the cost of a scanner is minimal compared to the benefits it offers. The equipment will pay for itself, in convenience, patient comfort, reduced risk, and product quality, truly differentiating the premier clinics from those still operating with 20th-century procedures.

Correspondence to Dr Traynor at: [email protected].
Citation for this article: Traynor R. Medico-legal considerations with 3D digital ear scanning. Hearing Review. 2021;28(6):20-22.
References
- Wynn MK, Kahn JM, Abel DJ, Allen RL. External and middle ear trauma resulting from ear impressions. J Am Acad Audiol. 2000;11:351-360.
- Beyer C, Younker S. Preventing medical errors for audiologists-2011 update. AudiologyOnline. https://www.audiologyonline.com/articles/preventing-medical-errors-for-audiologists-806. Published September 26, 2011.
- Strom K. 3DM scans the future of hearing care. Hearing Review. 2012;19(7):28-35.
- Traynor RM. Competing in the new era of hearing healthcare Part 3: Differentiating the practice with product and technology. Hearing Review. 2019;27(2):20-21.