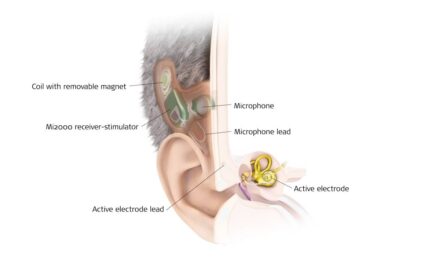
Figure 4 (above). An off-the-ear processor, fit on a 1-day post-surgery incision.
There are steps you can take to ensure same- and next-day CI activation goes smoothly for the patient and your clinic.
By Allison Biever, AuD; Grayson Bishop, AuD; and David Kelsall, MD
Cochlear implants are the treatment of choice for patients who have advanced hearing loss and limited benefit from hearing aids.1 Traditionally, patients wait 3-4 weeks after surgery before having their cochlear implant sound processor activated.2 Enabled by smaller devices, softer surgical techniques, and streamlined fitting practices, earlier device activation has been investigated, with numerous studies demonstrating that same- and next-day activations are both safe and effective.3
Since the Rocky Mountain Ear Center (RMEC) in Englewood, Colo., serves a large geographic area, our clinic began exploring early activation to reduce patients’ travel burden for follow-up care. Early activation also allowed our patients to hear better faster by limiting the gap between surgery and the typical delayed activation. Overall, patients were very satisfied with early activation, and therefore, our clinic has extended the offer of early activation to more patients.
The purpose of this article is to share RMEC’s experience and practical implementation considerations for clinics interested in offering same- or next-day activation.

Clinic Team Considerations
Close collaboration between the surgical and audiology teams is important for successful same- or next-day activations of cochlear implants. Here are some items to work through as a team when discussing early activation.
Should our clinic offer same- or next-day activation?
The logistics needed for same- and next-day activation are slightly different, and it’s important to understand what is involved with each before determining which your clinic might want to offer. You can use the following pro and con lists to help guide your decision.
Same Day:
PROS
- Having surgery and activation on the same day may eliminate the need for an additional trip to the clinic or an additional night in a hotel for out-of-town patients, depending on your set-up.
CONS
- Increased difficulty coordinating audiologic and surgical schedules compared to next day activations.
- May not account for all patients and surgical times due to varying anesthesia recovery duration.
- Patients will need to travel from the surgical center to the audiology center if these are in separate locations.
Next Day:
PROS
- Ease of scheduling: Activation is booked as a typical clinic appointment with an audiologist.
- Patients generally feel better the day after surgery, compared to the day of.
CONS
- Might require an additional trip to the center.
- Could require the need for a hotel and/or additional transportation accommodation.
Further Reading
What decisions, training, and materials are needed to enable early activation?
Team Alignment
As a team, you’ll need to discuss with the patient your center’s typical recommendation for post-op ear dressing with a pressure bandage. Ensure the patient is informed that the audiologist might be removing the head wrap, and coordinate audiologic and surgical appointments when possible.
At RMEC, our typical follow-up schedule varies based on whether the patient is local or travels from out of town. For local patients, we coordinate a medical visit for suture removal with the first audiologic follow-up at the 2-week interval. In the rare instance that a patient cannot be activated early, this appointment serves as the initial activation, maintaining a reasonable activation timeline.
For out-of-town patients, medical and audiologic follow-ups are coordinated at 3 months post-activation. The sutures are removed by a local physician. In these instances, we often use telehealth for an additional audiology touch point between activation and the 3-month follow-up.
Training
Audiology training on headwrap removal and incision management with the surgical team is important. Incision education should include common red flags and how to recognize when it’s necessary to make a referral. It’s also essential to establish an available line of communication across teams to be used should any issues arise.
Materials
If the patient will be wearing the headwrap when presenting to the audiologist, have the following materials available:
- PPE (e.g. gloves)
- Scissors to remove headwrap
- A readily available appropriate disposal bin
- Gauze pads (often called “four by fours”)
- Sanitizing supplies
Audiologic Considerations
How should I program for these patients?
Ensure the programming process is as easy as possible for the patient. RMEC prefers to use template-based programming like population mean for all activations and we find it especially beneficial for early activation to reduce programming fatigue for the patient.
Impedances are typically low, which is advantageous.4 Lower impedances result in higher compliance limits, reducing the need to manipulate parameters to achieve an optimal MAP.
How should I fit these devices for the patient?
Sound Processor Choice
If you are a two-processor center, consider ordering at least one behind-the-ear (BTE) device, as off-the-ear (OTE) sound processors can have more frequent retention issues. If you are a one-processor center, consider having a loaner stock of BTE devices for instances in which a patient selects an OTE and has difficulty with retention.
Our center ultimately did not see any issues with fitting the sound processor directly on the ear, which simplifies the fitting. However, if your center does not feel comfortable fitting a BTE directly on the incision, consider using a long coil cable and a clip, as shown in Figure 2. Note that this equipment is not part of a standard kit, so select the appropriate equipment on the order form or request to have a longer cable for your clinic stock in case this issue arises.
Supplies needed for off-ear fitting include:
- Long coil cable
- Off-the-ear retention device (e.g., Koala clip from Cochlear)

Magnet Options
Provide the patient with two magnets: the clinician-recommended magnet strength and a weaker magnet, usually one step below the clinician-recommended magnet strength. Be sure to select two magnet strengths on the order form if this is not standard. Have a clinic supply of assorted magnet strengths for both BTE and OTE processors.
In discussions with other professionals, we’ve found that retention is often a concern. We find this to be largely infrequent, with retention issue rates at our clinic being similar to that of traditional activations. We feel this may be related to the patient wearing the headwrap, which applies compression to the receiver stimulator area. We then fit the device where the magnet allows for additional compression to the magnet/coil area.

How should I counsel these patients?
Patient counseling should include discussion of device use and what potential issues to monitor for following activation.
Basic device use is what our clinic focuses on, reviewing only necessary skills such as charging the batteries and getting comfortable putting the device on and taking it off. We do not recommend counseling regarding the accessories at the time of activation. Consider counseling on basic use prior to activation, and if possible, utilize manufacturer counseling services.
Empowering the patient is also important. We encourage full time device use of greater than 10 hours per day and use of Master Volume Bass Treble (MVBT) and/or progressive MAPS to ensure appropriate acclimation to electric sound. During counseling you can also provide education about your center’s preferred aural rehabilitation.
We share a one-page handout of what to monitor for regarding the incision (e.g. purulent drainage, signs of infection) as well as potential magnet issues (e.g. redness, soreness at the magnet site). It’s recommended to encourage the attendance of a partner or caregiver for counseling and recruit them to perform monitoring, since the patient does not have visibility to the postauricular incision.
How should I monitor these patients?
Easy! Follow up as usual. You could also consider adding a remote care visit to monitor the magnet site. If fitting the sound processor on the incision, remind the patient to clean the sound processor daily with something like a soft, dry cloth for increased cleanliness.
Additional Considerations
Inclusion of an administrative team member or audiology assistant may be useful to ensure device availability, making sure the order is placed such that the device is shipped in time for a same- or next-day activation.
Further Reading
Surgical Considerations
In general, when it comes to early activation of cochlear implants, follow the principles of least invasive surgical techniques, which may include:
- Performing a mastoidectomy with a small incision (3-4 cms)
- Limit incision and tissue retraction to the extent possible
- Soft technique for round window or cochleostomy
Our center uses sterile adhesive strips to protect the incision and maintain a clean incision site in pediatric patients. In adult patients, removable sutures are used per surgeon preference. Using a topical adhesive like Dermabond to protect the incision is also a good option. It’s also a good idea to limit time under anesthesia as possible to ensure patients are best prepared for their activation.
Conclusion
Our patients have expressed high satisfaction with early activation. They are often relieved to have early access to hearing again and appreciate the reduction in travel burden compared to traditional activations.
If you are interested in piloting early activation at your center, consider patients who would experience maximal benefit: those traveling long distances, are receiving their second implant, or only have hearing in the ear to be implanted. We hope these insights help you seamlessly integrate early activation into your clinical practice to achieve the ultimate goal of helping patients hear better faster.
About the authors: Allison Biever, AuD, received her bachelor’s degree from the University of Alberta in 1989, her master’s degree in Audiology at the University of Colorado in 1992, and her AuD from Central Michigan University in 2005. She currently works at the Rocky Mountain Ear Center, which is a private neurotology practice in Englewood, Colorado. She can be reached at [email protected]. Grayson Bishop, AuD, earned her bachelor’s degree in communication sciences and disorders from the University of Central Florida in 2019. In 2024, she completed her AuD at the University of Florida. Dr Bishop completed her externship at Rocky Mountain Ear Center in conjunction with Cochlear Americas in Lone Tree, Colorado. David C. Kelsall, MD, is co-owner and medical director of the Rocky Mountain Ear Center. Dr Kelsall is an honors graduate of Stanford University and earned his medical degree at the University of Colorado. He is board certified in Otolaryngology, a Fellow in the American Academy of Otolaryngology/Head and Neck Surgery, and a member of the American Neurotology Society and the Colorado Medical Society.
References
- Alahmadi A, Abdelsamad Y, Alothman NI, et al. A Literature Review on Cochlear Implant Activation: From Weeks to Hours. Ear Nose Throat J. Published online August 8, 2023. doi:10.1177/01455613231188294
- Coelho DH, Shiao AS, Li LP. Very early activation of cochlear implants: A review of the literature. J Chin Med Assoc. 2023;86(1):7-10. doi:10.1097/JCMA.0000000000000816
- Alshalan A, Abdelsamad Y, Yousef M, Alahmadi A, Almuhawas F, Hagr A. Early activation after cochlear implantation: a systematic review. Eur Arch Otorhinolaryngol. 2023;280(8):3489-3502. doi:10.1007/s00405-023-07965-3
- Aldhafeeri AM, Saleh S, Almuhawas F, Hagr A. Feasibility of Day Surgery for Cochlear Implantation under Conscious Sedation with Same-Day Fitting. J Int Adv Otol. 2020;16(3):303-308. doi:10.5152/iao.2020.8208