Tech Topic | February 2022 Hearing Review
By Drew Dundas, PhD, and Suzanne Carr Levy, PhD
Part 3: What’s the big deal about audibility, and who can benefit from a broader audible bandwidth?
This 3-part series is a high-level review of the data that has accumulated across more than 10 years of clinical research with the technology at the heart of the Earlens system. In Part 1, we dove into the speech understanding data to demonstrate how increasing the audible bandwidth of processed sound results in improved speech understanding performance from several perspectives. In Part 2, we discussed the perceptual benefits to naturalness and overall sound quality. Finally, in Part 3, we’ll deep dive into the restoration of audibility and how the Earlens approach to overall audibility improvement is reliably achieved in fittings via direct drive—as well as who may benefit from this.
Digital acoustic hearing aids have comprised the standard of care for the treatment of up to severe sensorineural hearing loss (SNHL) for more than 20 years. However, despite advances in features and functionality, patients continue to seek better performance and a more natural listening experience. With increasing awareness of the importance of treating hearing impairment early and effectively by maximizing the bandwidth of audibility, we are beginning to see patients actively seeking out technological solutions—and some of these solutions, including Earlens, may challenge the standard of care. In this article we’ll go back to basics regarding audibility, debunk a few clinical myths, and discuss the importance of audibility for long-term cognitive health.
Back to Basics: What Is Audibility?
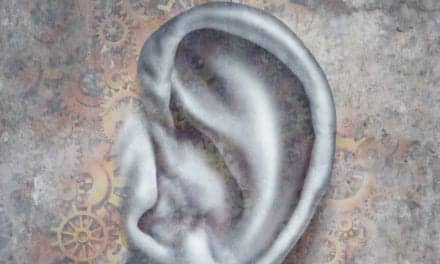
It’s worthwhile to take a moment and discuss what the term “audibility” really means. A sound becomes audible when it is presented at a level that is greater than the threshold of hearing at a particular frequency, triggering neural impulses that travel through the auditory system and upwards to the cortex where it can be interpreted. A sound that is below a listener’s threshold is not “too quiet”—it does not exist! For listeners with normal hearing, speech is audible across the frequency range from below 100 Hz to over 10 kHz even for soft presentation levels. For listeners with a typical sloping SNHL, the lower frequency sounds of speech (eg, vowels) occur at levels that are above the unaided thresholds and are therefore audible, whereas the higher frequency sounds (eg, consonants such as /s/, /f/, /k/, and /sh/) fall below the unaided hearing thresholds and are therefore inaudible. We can visualize the limits of the bandwidth of audibility by determining the frequency at which speech sounds drop below the thresholds of hearing (Figure 1).
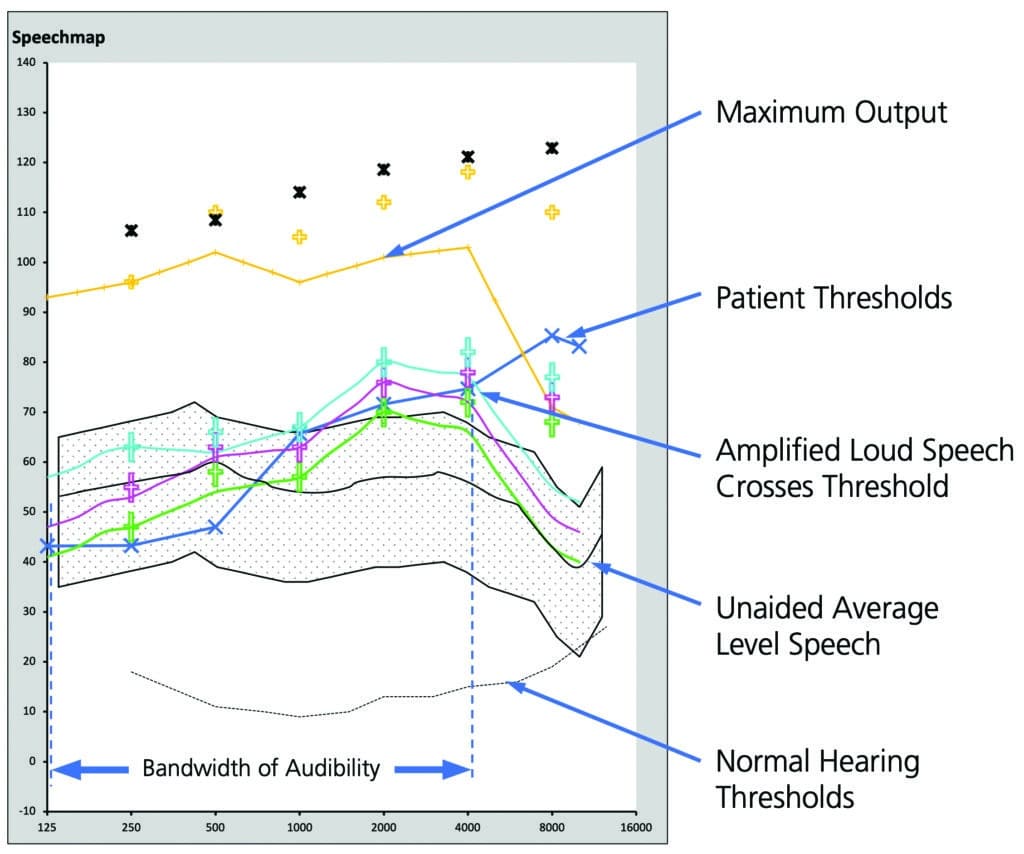
Figure 1. Real ear “Speech Map” plot of acoustic hearing aid fitting for mild sloping to moderate SNHL. Modeled on Audioscan Verifit2 screen.
Revisiting the Purpose of a Hearing Aid
We all understand that the fundamental purpose of any hearing aid fitting is to restore the greatest possible degree of audibility for speech to the hearing-impaired listener. Raising this signal above threshold via the appropriate application of gain makes it possible for the listener’s brain to use the encoded information to understand speech better. Practically speaking, of course, we must attempt to do this while maintaining loudness comfort and balancing performance benefits against perceived sound quality.
Nevertheless, in today’s high-tech, ever-changing clinical world, it’s possible to lose track of audibility when we are selecting and comparing devices based on features. As an industry, we’ve come to use features as differentiators to help make product recommendations, as well as a motivation to “upgrade” a patient’s technology. However, if we look critically at the spec sheets published with each successive release of technology, are there actually significant differences between levels or generations of technology in terms of what we can make audible for patients?
If we can agree that audibility of speech is the most critical requirement for the hearing impaired, it would appear that the answer to the above question is “No, there aren’t many significant differences between technology levels or even generations.” This is because:
- The maximum output and full-on gain specifications have remained relatively consistent from product generation to generation, and
- The maximum output that can be achieved in the ear tends to roll off to such an extent that it falls below the threshold of hearing for many listeners at a disappointingly low frequency (see Yellow Maximum Output curve in Figure 1 for an example).
This second point is especially true in “real world conditions” with open fittings. Wherever the maximum output of the hearing aid falls below the threshold of hearing, it will not be possible to make any sounds audible in that frequency region, regardless of how much gain can be applied or how advanced the sound processing may be. (The skeptical reader is invited to download the specifications sheets for their favorite manufacturer’s current and previous generation products and compare the ANSI S3.22 test specifications for themselves.)
So, Why Is Audibility So Important?
David Pascoe, PhD, succinctly (and amusingly) answered this question 40 years ago:
“Although it is true that mere detection of a sound does not ensure its recognition, it is even more true that without detection the probabilities of correct identification are greatly diminished.”1
Said another way, if sound information in a particular frequency region cannot be brought above the threshold of hearing, the patient is guaranteed to not be able to make use of that information! This is intuitively obvious, and yet we have been “trained” to accept that a narrow bandwidth of audibility improvement is acceptable because, as the standard of care, acoustic hearing aids have been our only treatment option. Despite the many justifications for missed audibility, without the diagnosis of a cochlear dead region via an accepted screening tool such as the TEN Test,2,3 wouldn’t it make sense to instead assume that patients could benefit from an extended bandwidth of audibility if sound quality could be made acceptable, until proven otherwise?
Mounting research, as well as data presented in Parts 1 and 2 of this series, suggest that the answer is an unequivocal “Yes.” Increased audible bandwidth is helpful to listeners due to the increased access to the informational redundancy of speech, which makes it easier to distinguish a target talker from a background of noise.
High-frequency audibility is also helpful because background noise tends to be low-frequency biased, resulting in a more favorable signal-to-noise ratio in the higher frequencies.This occurs, in part, because the shorter wavelengths of high-frequency sounds tend to be better absorbed by common architectural materials, resulting in shorter reverberation times for the consonant sounds and a less “muddled” speech in noise problem for the brain to sort out.4
Additionally, signal processing can only be of benefit in frequency regions where the output of the hearing aid is a) audible, and, b) where the amplified path into the ear dominates the direct unamplified path. When we consider these last requirements, it is not so surprising that many patients with acoustic devices report little benefit from dedicated environmental programs or advanced features when fit with open or vented devices. The venting allows them to listen to the low frequencies through the vent rather than through the hearing aid, negating much of the benefit of advanced signal processing. So really, the opportunity for effective treatment of hearing impairment is not only in terms of maximizing audible bandwidth, but also in maximizing the audible bandwidth that is processed and experienced through the hearing aid!
Audibility and Brain Health
The links between brain health, hearing health, and untreated hearing loss have recently become front-page news. With the average lag time between initial diagnosis and adoption of hearing aids remaining at 7-10 years, clinicians have embraced this compelling information to help motivate patients to act in their own best interests.
Let’s distill this massive amount of information down to a few key points:
- Age-related hearing loss is associated with increased risk of dementia and cognitive decline5;
- The mechanism linking the two is not well understood, but one hypothesis is that auditory deprivation may cause cortical remapping and thereby decrease cognitive reserve6;
- Age-related hearing loss typically begins in the high frequencies and progresses over time;
- Hearing aids that restore audibility and are well fit (verified fit to validated targets) have been shown to reverse compensatory cortical changes7;
- Underfit hearing aids (with reduced provision of audibility) did not reverse the brain changes (as Dr Sharma presented at AAS in 2020),8 and finally,
- It remains to be proven that cognitive decline can be prevented or reversed by improving audibility with hearing aids.
This question is currently being investigated in NIH-funded work; study results from Dr Frank Lin and colleagues are expected in 2023.9 We can’t help but wonder how provision of useful audibility through 10 kHz and broadband audible signal processing might impact the results, rather than the typical 5 kHz audible bandwidth of acoustic hearing aids.
How Does this Relate to Earlens and Who Can Benefit from It?
Part 1 of this series described how the direct-drive mechanism used by Earlens results in an audible bandwidth from below 100 Hz to 10,000 Hz, compared to an average upper limit of audibility of approximately 5 kHz for a well-fit acoustic hearing aid. The broader audible bandwidth beyond 5 kHz achieved with Earlens results in significant improvements in speech understanding in noise. Part 2 of this series described how the direct-drive mechanism of action allows normalization of overall loudness by balancing loudness perception across the cochlear critical bands. This is achieved by delivering audible low frequencies while vented, combined with audible high frequencies without feedback limitations, resulting in a superior sound quality experience.
For the population of listeners with mild to severe SNHL in the Earlens fitting range (Figure 2), clinicians should expect to deliver audible speech from 100-10,000 Hz without compromising the comfort of venting, resulting not only in a superior sound quality experience but also significant performance improvements for speech understanding.
Figure 2. Earlens fitting range
But Don’t I Need an ENT to Dispense Earlens?
Yes. Earlens is a bit different: a trained ENT physician pairs with a skilled audiologist or hearing instrument dispenser to ensure the proper fit and function of this customized device. The patient must maintain the Lens with an application of mineral oil to the ear once or twice a week. The oil also helps to soften cerumen and hydrate the skin, eliminating itchy ears. Because of the need for skilled providers and the custom design this device cannot be sold online and is currently only available at a limited number (but growing!) of forward-thinking clinics around the United States.
Let’s consider the broader implications of being an Earlens provider and partnering with an ENT practice. The Earlens system is completely differentiated from all acoustic hearing aids, PSAPs, and devices sold online or in Big-Box retail. Care can’t be outsourced to a call center. It requires the skills of healthcare providers with the most education in the diagnosis and treatment of hearing loss. Finally, by providing superior audibility, it represents what may be the best opportunity to help stem the coming wave of comorbidities of dementia and declining cognitive health that we have all been reading about.
Different work? Somewhat. Broader restoration of audibility? Definitely. Different than Big Box, OTC, or online? Unquestionably.
Summary
The standard of care for the treatment of up to severe SNHL hasn’t really changed much in 20+ years, and patients are still seeking better performance and a better listening experience. With increasing awareness of the importance of treating hearing impairment early and effectively by maximizing the bandwidth of audibility, patients are more and more likely to investigate their options and make decisions about treatment based on what presents the greatest value to their individual situation. It’s clear, however, that value isn’t just about price. Adding an option to your portfolio—a non-surgical, medical treatment for sensorineural hearing loss—that results in clinically superior speech understanding in challenging situations, produces superior sound quality, and that is strongly preferred by patients might just change that standard of care for the better.
Correspondence can be addressed to Dr Dundas at: [email protected].
Citation for this article: Dundas D, Levy SC. A 10-year review of the Earlens System, Part 3: What’s the big deal about audibility and broader audible bandwidth? Hearing Review. 2022;29(2):24-27.
References
- Pascoe DP. Clinical implications of nonverbal methods of hearing aid selection and fitting. Sem Hear. 1980;1(3):217-228.
- Moore BCJ. Dead regions in the cochlea: Diagnosis, perceptual consequences, and implications for the fitting of hearing aids. Trends Amplif. 2001;5(1):1-34.
- Moore BCJ. Testing for cochlear dead regions: Audiometer implementation of the TEN(HL) Test. Hearing Review. 2010;17(1):10-16,48.
- Schnitta B. Achieving optimal reverberation time in a room, using newly patented tuning tubes. Proc Mtgs Acoust. 2013;19:015105
- Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413-446.
- Beck DL, Bant S, Clarke NA. Hearing loss and cognition: A discussion for audiologists and hearing healthcare professionals. J Otolaryngol-ENT Res. 2020;12(3):72-78.
- Glick HA, Sharma A. Cortical neuroplasticity and cognitive function in early-stage, mild-moderate hearing loss: Evidence of neurocognitive benefit from hearing aid use. Front Neurosci. 2020;14..
- Glick H, Sharma A. The brain on hearing aids: Can treatment with hearing aids improve neurocognitive function in age-related hearing loss? Hearing Review. 2021;28(1):28-32.
- Beck DL. The ACHIEVE study, cognition, amplification, and audition: An interview with Jennifer Deal, PhD. Hearing Review. 2022;29(1):30-31.
Articles in this series:
- A 10-Year Review of the Earlens System, Part 1 (Dec 2021 HR, pgs 14-16)
- A 10-Year Review of the Earlens System, Part 2: Direct Drive: Sound Quality and Preference Evidence (Jan 2022 HR, pgs 14-15)
- A 10-Year Review of the Earlens System, Part 3: What’s the Big Deal about Audibility and Broader Audible Bandwidth? (Feb 2022 HR, pgs 24-27)