In the end, the failure of hearing conservation programs (HCPs) to prevent hearing loss can be attributed to one thing: the effectiveness of personal hearing protection while on-the-job is completely unknown. Detailed here is a system designed to provide real-time information for HCP managers so they can intervene before occupational noise-induced hearing loss occurs.
When faced with a persistent problem in any hearing conservation program, such as extreme noise exposures or excessive OSHA standard threshold shifts (STS), hearing conservation professionals often run through the same cycle of tactics and interventions to solve the problem. Too much noise? The prescription is to reduce noise through engineering and administrative controls: install acoustical enclosures, baffles, and dampeners; increase frequency of machine maintenance; and rotate workers in noisy areas on shorter shifts.
Unfortunately, these efforts rarely reduce the exposure to an acceptable level. Therefore, hearing protective devices (HPDs) are still required—namely, providing workers with highly rated earplugs or earmuffs—with the possibility of resorting to dual protection (ie, earplugs and earmuffs). Then, one remeasures the ambient noise with sound level meters and personal noise dosimeters. If the problem persists, one repeats the process: increase the hearing protection attenuation and reinvest in the same practices, perhaps ad infinitum.
Note that the final step in calculating personal exposure is to guess at hearing protector attenuation. Grossly inaccurate estimates of hearing protector performance in the field may be responsible for the prevalence of noise-induced hearing loss (NIHL) in industry.
This is a frustrating problem. Without quantification of HPD performance, hearing conservation efforts often result in no tangible progress toward protecting workers. The only feedback the industrial hygienist gets is an audiogram, which can only document the damage after it is too late.
At Dixie Industries, one manager introduced new technology to obtain precise information about individual worker noise exposure and to create new HCP tactics. The decision resulted in the abatement of an OSHA citation, as described below, and helped to change internal attitudes about hearing protection.
Case Study: Directive to Minimize Employee Noise Exposures
Ed Tougaw, production manager at Dixie Industries, and his organization had taken substantial measures over 10 years to mitigate a severe noise problem. Dixie Industries is involved in forging, one of the loudest endeavors in all manufacturing. Forging involves the use of heavy-duty hammers, presses, and rollers, generating forces upwards of 50,000 tons to shape metals into high-strength parts. Forged metals are inherently stronger than other processed metals, and are engineered to withstand a variety of application concerns, including weight, heat, and constant or repetitive use in machinery.
At Dixie Industries, operators stand in front of forging hammers that cycle up to 80 strokes per minute. The combined mass of the top ram and dies often exceeds 6,000 lbs of force, generating a massive amount of kinetic energy.1 Most of this energy is transferred in the deformation of the steel being forged. As the steel reaches its desired geometry, much of the excess energy is converted into sound that is loud enough to be felt as a physical presence. Typical employee 8-hour time weighted average (TWA) noise exposure levels reach upwards of 108 to 112 dBA. Dixie Industries’ HCP requires all workers to properly wear hearing protection throughout the facility and to use dual protection in the forge area.
Forging is a precision process. Operators must be able to see and manipulate the product as it is being formed, and effective shielding can be nearly impossible, according to Tougaw. This leaves the manager to rely heavily on proper personal protective equipment (PPE).
For over a decade, the operation also underwent over 30 different engineering noise control projects. More than $1.8 million was spent to install baffles, insulated walls, and noise-absorbent materials; redesign air valve controls on hammers; install quieter auxiliary equipment; relocate non-forging employees away from extreme noise areas; and move to less noisy equipment (known in our field as “buy quiet”). Yet, a noise problem persisted.
In the fall of 2005, Dixie Industries was cited by Tennessee OSHA (TOSHA) for excessive noise exposures. The TOSHA citation identified that Dixie Industries did not ensure that the hearing protectors attenuated employees’ exposure to at least an 8-hour TWA of 90 dBA and that the HPDs did not reduce overall exposure for workers with a STS to below an 85 dBA TWA (8 hours). Overall HPD attenuation was calculated using the “subtract 7, divide by 2” method, with 5 dB added to that value to estimate the benefit of the dual protection.
Dixie Industries was instructed by TOSHA to develop a detailed plan to implement further engineering or administrative controls to minimize employee noise exposures. About the engineering controls, Tougaw said: “We did not gain anything on the direct exposure to the hammer operators while they were operating the equipment. We reduced noise by a couple of decibels in the area of reflected and indirect exposure.”
Proposed Solution: “Upstream” Control of Noise Exposure
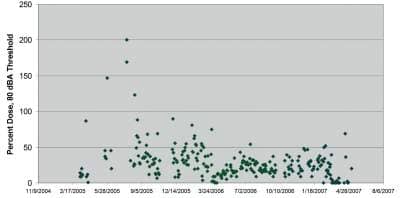
Figure 1. Scattergram of data for one worker. Alternatively, these scattergrams can be generated for entire departments, shifts, etc.2
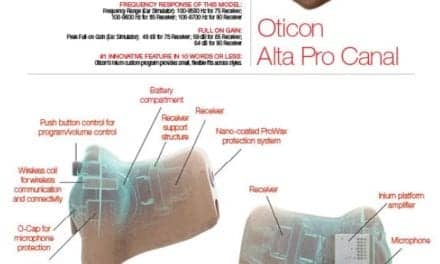
After following recommendations and guidelines from TOSHA, as well as implementing noise control solutions that had minimal effect, Tougaw sought out alternative methods to document and control the noise exposure problem. As recommended by a hearing conservation professional, Tougaw turned to the second author (KM) and J. Alton Burks, ScD, who had recently introduced in-ear dosimetry technology at another steel processing plant. This technology, now known as QuietDose™ from Howard Leight®, measures and quantifies an individual’s cumulative daily noise exposure, accounting for both the quality of fit of the HPD and for periods when HPDs are not worn.
Integrated into earplugs or earmuffs, QuietDose is designed to measure and record the worker’s actual protected noise dose over their entire work shift. When worn in-the-ear (insert-type HPDs) or over-the-ear (muff-type HPDs), QuietDose measures sound pressure level (SPL) interior to the protector. During periods when the protectors are not worn, QuietDose measures ambient noise level, which is equal to the exposure impinging on the ear (since HPDs are not being worn).
Thus, the QuietDose dosimeter measures the ear’s actual protected noise exposure, without any estimates of HPD performance. The authors believe this is the first time that this type of measurement has been available for the hearing conservationist, and it is the only quantity that is directly related to NIHL.
While QuietDose is useful as a sampling tool, in severe and/or high-risk conditions, it is likely that it will be worn by the noise-exposed workers every day as part of their PPE. When used as a continuous monitoring instrument, this provides hearing care professionals with a comprehensive daily noise exposure history for the workers.
The QuietDose Exposure Smart Protector (ESP) dosimeter meets Type II requirements as described in ANSI S1.25-1991(R2007). The dosimeter is a 2-channel device, with one microphone sampling in each ear. The binaural design eliminates the common “head shadow” effect that can compromise dosimeter accuracy. Each microphone is sampled 10 times per second, and the higher value between the two microphones is used for the dose computation. Thus, the level at each ear is combined in a conservative manner. Only one dose value is presented to the worker. For the worker, the benefits of the design include simplicity of operation, with minimal training and need for interaction.
Real-time alerting and documentation system. The dosimeter provides real-time alerts for instantaneous and cumulative overexposures. A red LED on the top surface of the dosimeter flashes when the instantaneous exposure level is greater than 85 dBA, which is generally considered to be the maximum safe level of noise exposure. This signal alerts the worker that he is currently accumulating noise dose. If the worker is not wearing the QuietDose hearing protectors, he should probably fit them immediately. If he is wearing the protector and the red LED flashes, then the worker should adjust the protectors for a better fit in order to improve noise reduction.
The yellow LED on the dosimeter top panel will flash when the cumulative exposure for the day nears the goal of 50%, which is equivalent to a TWA of 85 dBA. This signals that the worker is approaching the target level of noise exposure approved by the HCP manager. If the yellow LED is flashing, the worker should limit noise exposure as much as possible for the remainder of the work shift.
At the end of each day, the worker downloads the dosimeter readings by placing the ESP dosimeter in an infrared reader and pressing a button for about 2 seconds. The reader is connected to a personal computer running the QuietDose application software. The dose exposure information is instantly presented to the worker, and it is also relayed to the HCP manager. If the exposure level for the shift is below the goal of 50% dose, exposure levels were safe and no further action is required. If the exposure levels were greater than the target of 50%, management should intervene to ensure that the overexposures don’t continue. Intervention may take the form of retraining, refitting HPDs, or selection of a different HPD.
Measure and intervene: Reinforcing basic HCP tenets. The QuietDose approach to preventing hearing loss relies on two basic tenets of hearing conservation: 1) exposure to less than 50% noise dose (85 dBA TWA) on a daily basis will not cause hearing damage, and 2) noise-induced hearing loss won’t occur after a single overexposure. If intervention effectively limits the occurrence of overexposures, occupational noise-induced hearing loss can be eliminated. Optionally, more rigorous daily limits can be selected and/or the NIOSH and ACGIH criterion levels and exchange rates can be used. Measure and intervene—it’s as simple as that.
The application software archives all daily dose data per employee, and is capable of reporting data in various formats. If a daily download for a worker exceeds a pre-set limit, the software can send an e-mail or cell phone text alert to his supervisor or manager. This is designed to enhance accountability by making both worker and management immediately aware of any overexposures.
Figure 1 is a sample scattergram generated by the software. Noise dose values are plotted on the Y-axis against the date on the X-axis. For this worker, the initial downloads were within safe limits. Then, there was a brief period during which the noise dose was above the goal of 50%. According to the HCP, a supervisor would initiate an intervention to discuss the finding with the worker and develop a solution for the future. The goal is to empower the worker to keep nearly all daily exposures within safe limits, with only occasional overexposures.
Measure and Intervene
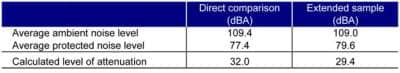
Table 1. Direct comparison and extended sample data of noise level and worker daily dose at Dixie Industries in 2007.2
Treatment of overexposures is absolutely critical for a successful QuietDose program. The science of NIHL is based on the fact that daily exposure to an 8-hour TWA of less than 85 dBA is not harmful to a worker’s hearing. NIHL occurs after months and years of overexposures, not after a single or occasional overexposure.
Thus, when the software reports that an employee has had a single work-shift overexposure, it’s critical that the HCP manager intervenes with the message, “Your exposure was too high today. Let’s do a better job with your hearing protection tomorrow and reduce your noise exposure.” Then, the next step would be to ensure that consequent noise exposure values fall in line with safe guidelines.
Monitoring personal exposure on a daily basis and intervening when necessary limits overexposures to occasional instances. By doing this, the HCP manager can all but guarantee that a worker will not suffer NIHL on the job.
In fact, this comprehensive data effectively delineates between occupational and non-occupational noise exposure. If a worker in the QuietDose program has a history of safe noise exposure at work, and still suffers NIHL, it is likely that the noise exposure occurred off-the-job. In a successful implementation of this model, the HCP manager provides proactive upstream prevention rather than be left to react to threshold shifts on audiograms after the damage is done.
Tougaw said he felt that QuietDose in-ear dosimetry could be the solution to documenting a solution to the noise problem with precise, personalized data. After receiving the approval and support from management, his team presented a new plan incorporating the technology to TOSHA in two steps. First, they presented past, present, and planned engineering and administrative controls.
“We referred to it as our ‘science fair’ presentation,” Tougaw says. “We covered the walls of our conference room with photographs and samples of our previous engineering work, consisting of 30 projects over an 11-year period representing an investment of $1.8 million. We also included proof of our administrative controls, including daily audits of our double hearing protection policy, and proof in the form of disciplinary action we were enforcing it.”
The final element was a proposal to use QuietDose to determine actual exposure levels. “We were fortunate that the representatives from TOSHA were aware of the product and open to the proposal,” says Tougaw. “They gave it their blessing and we kicked it off. From the beginning, we made the decision to use QuietDose as an instrument to collect actual exposure data and not use it as a replacement for our existing HCP.”
He acquired a QuietDose In-Ear Starter Kit for each enrolled employee, as well as software and calibration equipment. Drs Michael and Burks both visited the plant, and trained a team consisting of the plant’s environmental engineer, production supervisor, production manager, and two hammer operators in the use of the equipment. Six workers were enrolled full-time in the program and recorded their daily dose over several months. Concurrent ambient noise measurements also were recorded with a sound level meter.
Findings
The data from both in-ear and ambient dosimetry were collected and analyzed by Tougaw’s team.2 They found that workers utilizing in-ear dosimetry experienced noise exposures under the 90 dBA PEL. Moreover, nearly all measurements were under 80 dBA (Table 1). The workers exposed to the loudest of loud noise achieved only 25% of their allowable daily dose.
Tougaw found that in-ear noise dosimetry was able to prove that with proper protection, training, and motivation, workers can be adequately protected from extreme noise over an entire work shift, with statistics to back up these claims.
“From our extensive field studies, we weren’t surprised to see that the workers were adequately protected, especially since they were wearing double protection,” Tougaw said. “In fact, nearly all industrial exposures can be reduced to a safe level with a properly fitted single hearing protector.”
The data indicated that Dixie Industries was providing adequate protection. This shows that conventional de-ratings can be grossly inaccurate. In the end, the failure of HCPs to prevent hearing loss can be attributed to one thing: the effectiveness of personal hearing protection while on-the-job is completely unknown. HPD performance on an individual can’t be predicted from laboratory measurements, and fit-testing data are completely valid only during the fit-testing session. Since the attenuation is unknown, personal exposure is unknown. Industrial hygienists can prevent an occupational disease only if they can quantify the exposure. In our opinion, QuietDose offers a solution to a problem that has frustrated the hearing conservation community for decades.
Conclusion
Tougaw and his team presented the data to TOSHA in April 2007 and the citation was abated 2 months later. According to Tougaw, QuietDose provides a foundation for Dixie Industries’ overall hearing health care program, creating a value-based safety culture. In the last 4 years, the company’s lost time/reduced work ratio has dropped from 7.04 to 3.44, with a goal of 2.75 in 2011.
According to Tougaw, the in-ear dosimetry program also sent a message that everyone can make a contribution to the overall safety environment at the company. The case study also emphasizes that agencies like TOSHA really are there to help, not hinder, the development and success of industry.
References
- Forging Industry Association. Forging facts. http://tinyurl.com/6qd5kln
- Michael K. Establishing the real-world adequacy of personal hearing protection in a high noise environment: A case study in a forging operation. Paper presented at: American Industrial Hygiene Conference and Expo; May 2008; Minneapolis.
Citation for this article:
Bessette R., Michael K. Measure and Intervene: An In-Ear Dosimetry Method That Can Change an OSHA Violation—and Internal Attitudes Hearing Review. 2012;19(04):46-51.