What is the lowest price you can offer a hearing aid?
Can audiology practices compete in the sub-$800 per aid price range? What would be required to compete in this market arena? From a professional standpoint, is this something we wish to do?
Hearing aid pricing has long been a subject of discussion in audiological literature and among hearing aid users.1-4 While hearing aid pricing has never been rated as the primary impediment to obtaining appropriate hearing aids, it has repeatedly been noted as an important factor.5,6 Thus, marketing plans should address hearing aid pricing in order to have face validity.
This article examines marketing models that offer hearing aids at around $800 or less. All of these plans assume that the nationally established customary fees for diagnostic testing, hearing aid performance validation, and aural rehabilitation will be, in part, foregone by the provider. Authors’ Note: Although this article specifically addresses issues in audiology, we also believe that many of our points are relevant for and will resonate with our hearing instrument specialist and otology/ENT colleagues.
A Look at Low-Cost Hearing Care Plans
All of the cost-containment plans known to the authors have a streamlined evaluation procedure. Specifically, none require in-depth diagnostic testing for outer or middle ear pathology, retrocochlear disorders, central auditory processing deficit, balance disorders, or hair cell function. In our audiology clinic, these diagnostic screenings add an additional half hour of clinic evaluation time to every first meeting even when findings are negative.
Similarly, cost-containment plans do not require time-consuming real-ear aided testing and readjustment of the manufacturer’s best-fit algorithms. Such adjustments add an additional half hour to the fitting process during the patient’s initial visit under the best of circumstances.
Any plan that cuts 60 minutes out of clinic time during the first visit is cost-effective, as long as patient satisfaction and benefit are not compromised. However, our experience has been that many first-time hearing aid users report aided benefit as long as the hearing increases speech audibility above the unaided level. Moreover, Kochkin6 has stated that, if a hearing aid purchaser pays under $100 per percent of hearing aid improvement, they tend to report they are satisfied. Thus, a $90 disposable hearing aid needs only to add a minimum of 1% perceived hearing improvement to meet this satisfaction criterion.
Second, these plans are cost-efficient in that the equipment outlay is dramatically reduced. The real-ear measurement system described as “must have” technology by Consumer Reports4 costs between $5,000 and $12,000 per unit and requires expensive yearly calibration and occasional repair. Impedance equipment costs at least $3,000 per unit. Otoacoustic emission and evoked potential testing equipment with appropriate accessories costs approximately $17,000 per unit.7 Elimination of such equipment expense is a major money saver. As an example, our clinic requires three real-ear systems and three impedance meters to serve a population of 65,000.
In addition, there is no discussion of electronystagmography, caloric, rotational chair, acceleration platform, auditory brainstem response, electrocochleographic evaluation testing, nor video otoscopy, cochlear implant programming, tinnitus evaluation, or aural rehabilitation counseling in most hearing aid cost-containment programs. Elimination of these tests saves thousands of dollars in equipment purchase, calibration, maintenance costs, and time.
Third, any plan that does not take into account the above-mentioned services also requires less employee training and expertise. Thus, salaries can be lower, as less training is needed to perform a puretone audiogram and install the manufacturers’ “best-fit” algorithm into these low-priced hearing aids (if they are programmed at all).
Therefore, hearing aid prices can be minimized as long as the following criteria are met:
- Patients consider themselves satisfied with these hearing aids;
- Audiologists (and other dispensing professionals) are willing to accept the agreed-upon fee for minimalist hearing aid fittings; and
- Patients develop no exacerbated hearing or balance problems overlooked by such cost-containment strategies.
Issues Raised By Cost Containment
While the plans noted above have financial efficiency, they do not account for much of what audiologists are trained to do from a diagnostic, hearing aid fitting, hearing aid programming, hearing aid validation, vestibular rehabilitation, and aural rehabilitation standpoint. Likewise, our guess is that most hearing instrument specialists would also find much of the above problematic.
If elimination of these procedures had no effect on patient health or satisfaction, the plans noted above would be a “win” for all concerned parties: Less time and money spent by the patient; no overlooked medical conditions to worry about; less equipment outlay; less clinic time spent in hearing aid fitting verification; and fewer training requirements for the provider. Unfortunately, published data, including professional best-practice directives and state/federal regulations, say otherwise.
Proper Diagnosis of Hearing and Balance Disorders for Audiologists
As stated above, there are a number of hearing problems that audiologists diagnose including:
- Hearing disorders that are conductive outer ear;
- Hearing disorders that are conductive middle ear;
- Hearing disorders that are sensory outer hair cell;
- Hearing disorders that are sensory inner hair cell;
- Hearing disorders that are sensory strial;
- Hearing disorders that are related to cochlear dead regions;
- Hearing disorders that are related to auditory dysynchrony;
- Hearing disorders related to auditory neuropathy;
- Hearing disorders that are neural; and
- Hearing disorders that are localized to the auditory brainstem or central auditory system.
Audiologists are also charged with diagnosing various balance disorders and identifying potentially effective treatment strategies. Overlooking all of these diagnostic issues potentially endangers the patient should these disorders go unnoticed and untreated. These extra hearing and balance screening procedures add a minimum of 60 minutes clinic time for test execution, interpretation, and report writing—even when automated screening devices are utilized and all results are negative. Should positive pathological findings appear, the time easily expands to several hours of more in-depth evaluation, report writing, treatment, and specialist referrals.
Screening for other disabilities. Hearing loss is a medical condition that does not always exist in isolation; hearing loss often exists in conjunction with other disabilities. Published research has shown that 25% to 42% of children with hearing loss have at least one additional disability.8-11 Since these disabilities do not disappear over time and numerous studies show increasing central auditory and cognitive impairments associated with aging, this number is likely higher for aging adults.
In our clinic, like many across the country, we screen in four areas of function as suggested by Matkin (unpublished data, personal communication, 1980). These areas include: 1) Cognitive function; 2) Social-emotional function; 3) Motor (fine and gross); and 4) Speech-language (expressive and receptive). Some might argue that inquiry into these four areas is a waste of valuable clinic time, as the patient’s physician will be aware of these problems. We disagree. We see numerous adults in our clinic who have obvious cognitive problems that are not mentioned anywhere in their medical reports. We see numerous people with severe and profound hearing losses with highly distracting vocal behaviors that have never been evaluated or treated by a speech-language pathologist. We routinely see people in our clinic who are minimally mobile and at high risk of falling, but who have never been referred to a physical therapist for evaluation or treatment. Dysfunction in these four areas is not restricted only to children, and should be routinely screened in adults.
Hearing loss also results in a number of unfavorable economic and social conditions.12-17 Viewing hearing aid fittings from a marketing standpoint without due consideration of the associated medical, socioeconomic, cognitive, and psychosocial ramifications is potentially harmful to the patient and inconsistent with audiology “best-practice” standards.
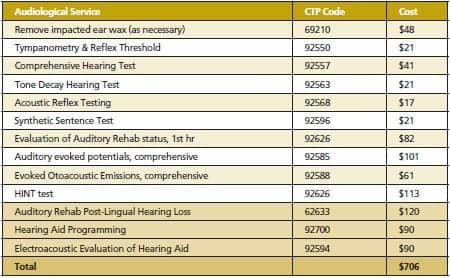
Table 1. Medicare fees as provided by the ASHA Web site for hearing and balance-related diagnostic testing.17
Neglect of Nationally Established Usual and Customary Fees Foe Audiological Services
Physicians and accountants representing the Centers for Medicare and Medicaid Services have worked for years with scientific/professional audiology organizations to establish a list of tests, services, and fees that are considered necessary to protect patient health. Any attempt to sell hearing aids at a price that is lower than the fees for the hearing aid plus diagnostic and validation tests necessary to confirm appropriate hearing health care and hearing aid performance is contrary to this agreement.
The list in Table 1 represents the Medicare fees as provided by the American Speech-Language-Hearing Association (ASHA) Web site for hearing and balance-related diagnostic testing.18 Table 1 shows additional fees for hearing aid fitting and verification provided by numerous other third-party payors. Strom19 notes that it is not unusual to find many or all of these tests routinely provided in audiology clinics and hospitals around the country. Even more common are the last three items on the list, routinely provided to those who require hearing aids.
The services noted in Table 1 add up to $706. Anything below this amount ignores the agreement reached by an independent third-party review board and the major US audiology organizations.
Hearing and Performance Verification Issues
Each person should know in some scientifically validated, repeatable, and quantifiable way what the hearing aid is providing for the unit cost.
While we agree that inexperienced hearing aid users typically can identify when hearing aids are providing some benefit, we do not agree their assessment of benefit is the sole criterion for “successful hearing aid use.” As stated previously, most new hearing aid users will note that any improvement above the unaided condition is perceived as benefit. At a cost of $90 per hearing aid, it does not take that much to perceive aided benefit using Kochkin’s $100 per percent benefit calculation. Further, unless hearing aid users have tried numerous brands and models of hearing aids all set to the same level of real-ear aided audibility for soft, medium, and loud speech, they really do not have the perspective to say they are “doing well” with any single hearing aid.
Even the second author, who has worn hearing aids most of her life and is pursuing a doctoral degree in audiology, initially presented at our clinic with a hearing aid that she deemed satisfactory. Her QuickSIN20 score with this hearing aid at 50 dBHL was a paltry 18.5 dB SNR loss (ie, higher scores on QuickSIN indicate worse performance). Further, her performance with this hearing aid in one-to-one quiet conversations in meetings and on the telephone was minimal at best. Since this time, she has tried 15 different hearing aids from six different manufacturers, one of which yielded a score of 5.5 dB SNR loss on the QuickSIN at 50 dBHL.
Few would argue that a hearing aid providing an 18.5 dB SNR loss would be deemed satisfactory if the hearing aid user had been previously wearing a hearing aid that yielded a 5.5 dB SNR loss under the same testing conditions. Thus, user perception of benefit can be of limited value even with sophisticated long-time hearing aid users. As Cox and colleagues21 stated:
“Because [hearing aid user satisfaction surveys] depend partly on the personality of the hearing aid patient, wearer-oriented outcomes are not very sensitive to differences [among] hearing aids. As a result, wearer-oriented outcomes are not optimal for use in clinical trials of new technology or processing strategies. There are no existing questionnaires that are known to be primarily device-oriented and relatively free of personality influence.”
In our clinic, we use real-ear aided performance verification at 40, 55, and 75 dBSPL inputs coupled with aided and unaided speech intelligibility index computation and performance scores on the QuickSIN presented in calibrated soundfield at either 45 or 50 dBHL as our standard of hearing aid benefit.
The QuickSIN test was chosen as our preferred speech-in-noise test because it is time efficient and well standardized.
However, using multi-input level real-ear aided testing, unaided and aided speech intelligibility index calculation, and QuickSIN testing in soundfield adds 1 hour minimum to the initial hearing aid fitting and a minimum 2 hours of follow-up visits, reprogramming, and Q&A sessions. Thus, we have added 3 hours to the process of hearing aid provision.
Kochkin’s MarkeTrak survey5 shows that this time spent in follow-up positively impacts hearing aid user satisfaction—which should translate into improving the hearing aid user’s quality of life.22 However, such services cannot be provided at the same cost offered at facilities that use none of these diagnostic and validation procedures. Further, if the selected hearing aids utilize Bluetooth connectivity or audio-zoom-type functions, another 2 hours are added to hearing aid programming, performance verification, and hearing aid orientation at minimum.
Hearing and Repair Verification
After a hearing aid returns from repair, changes in microphone and receiver frequency responses can dramatically alter hearing aid output. Replacement of the suspension tubing in the microphones and receiver may have a similar effect. If these changes are not measured with a real-ear system, there is no way to assure optimum speech audibility has been maintained.
These problems become particularly apparent to the patient when the new microphones or receivers result in acoustic feedback that was not present when the instrument was initially fit. These feedback problems occur due to new peaks in the response output, producing a feedback loop that did not previously exist. Similar problems occur when the earmold tubing or venting is modified, the medial tip of the earmold is ground down, or the earmold is replaced.
For all these reasons, hearing aid feedback calibration must be repeated after such repairs are completed. Subsequent to such repairs, real-ear aided speech audibility must be measured. We routinely allot an additional half hour of clinic time for this post-repair validation.
Patient Education and Counseling
Patients must be trained in proper use and care of their hearing aids. Even with the most basic hearing aids, patient training should include earmold/shell and battery insertion, proper placement of the hearing aid, proper care of the hearing aid, and use of the telecoil. In our clinic, many hearing aids are Bluetooth compatible and utilize multiple programs and/or forced directional functions. Proper patient training in these areas adds another 2 hours minimum to the clinic time.
Kochkin23,24 showed that training the patient to function successfully on the phone, when watching television, when attending meetings or classes, when attending parties or family group functions, and when listening to television or music increases hearing aid user satisfaction. Specifically, he showed that the more listening situations in which a hearing aid user can communicate, the higher the user satisfaction ratings. Thus, if customer satisfaction is the goal, this training time should be spent.
When the aforementioned hearing aid use training is over, we find it necessary to host an additional 1.5-hour monthly group training session to answer ongoing questions that hearing aid users and their families bring to the meetings. We find this training more cost-efficient than addressing ongoing questions in a patient-by-patient setting. We spend a minimum of 15 hours per month preparing for these meetings. Without the meetings, patients have limited means of getting updated hearing aid information that has come from randomized, double- or single-blinded, placebo-controlled studies based on a homogeneous population, as recommended by the US Department of Health and Human Services.25
We also use these meetings to demonstrate how people with significant hearing losses can function in a group meeting using multiple microphones connected to Bluetooth, FM, infrared, and loop systems.
Recommendations
From the above discussion, we have compiled a list of recommendations for an audiology marketing plan that attempts to balance documented patient satisfaction strategies with cost-containment measures and audiologist expertise.
Price hearing aids with due consideration of diagnostic best-practice standards and time spent in the hearing aid fitting and counseling process. Diagnostic, hearing aid fitting, training, verification, and education take at least 9 hours of time even when no active auditory or vestibular pathology exists. To provide a hearing aid at a cost of $90 per single unit would require that the audiologist or dispensing professional ignore American Academy of Audiology (AAA, 2006) and ASHA (1997) “best practice” standards, ignore potential legal liability, and, in the case of audiologists, stop diagnosing hearing and balance disorders for those purchasing a hearing aid. None of these marketing options seem realistic.
We propose that audiologists do what they are trained to do. One look at any audiology AuD or PhD program shows audiology to be a profession focused on statistical analysis of data, scientific inquiry, auditory and vestibular research, behavioral and physiological testing of the balance and auditory system, and auditory/vestibular rehabilitation. The sole benchmark of success should not be the distribution of hearing aids with little or no regard for audiological services. Allying with any of these groups has nothing to do with audiological training. Audiologists should practice what we are trained to do and bill for those services.
Monthly group education to address ongoing patient questions and concerns. Most of our patients who need hearing aids have questions after the first, second, and third scheduled clinic meetings. It is our experience that patient questions continue over the years. Without an ongoing means of addressing these questions, patients become less satisfied hearing aid users.24 Moreover, meeting others who are going through the same hearing, balance, and hearing aid issues seems to have some counseling benefit.24,26-30
Multiple input real-ear aided and QuickSIN aided verification measures of all hearing aid fittings and modifications. The data that support this recommendation are discussed above and can be viewed in greater detail on the AAA Web site.31
Use of audiology assistants where possible. Nearly 30% of audiologists report using audiology assistants.32 It is not cost-efficient for audiologists to spend time grinding earmolds and hearing aid shells, tubing custom earmolds, changing tubes on open-ear hearing aids, cleaning hearing aids, demonstrating proper hearing aid and battery insertion, checking battery voltage, cleaning equipment, inputting data into Noah and real-ear systems, etc. This work is within the scope of practice for audiology assistants33,34 and is an appropriate cost-containment measure.
Use of less-expensive hearing aids when real-ear and QuickSIN performance measures suggest similar performance. Data from Leavitt and Flexer35 have shown that an analog single-microphone, single-channel hearing aid can outperform today’s most expensive fully digital hearing aids with a myriad of noise reduction features, provided the analog hearing aids are set to real-ear verified NAL-R and the digital hearing aids are set according to the manufacturer’s “best fit” algorithm. This finding suggests that real-ear programming and aided speech audibility are more important than today’s state-of-the-art hearing aid noise-reduction features when those hearing aids are set using only the manufacturers’ best-fit algorithms.
Further, it has not been demonstrated in double-blinded, randomized, placebo-controlled studies that today’s most expensive contemporary digital hearing aids provide better speech recognition in noise than each company’s least expensive hearing aid models. Until these studies are forthcoming, we cannot assume significantly better hearing aid performance will be obtained with today’s most expensive hearing aids.
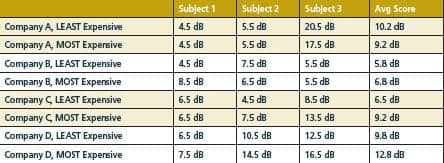
Table 2. QuickSIN scores for three subjects using four companies’ least-expensive and most-expensive hearing aids. All models were fit to equivalent REAR values for 40, 55 and 70 dBSPL inputs.
Table 2 shows results for three long-time digital hearing aid users who in a single-blinded, randomized, clinic setting listened to equivalent randomized QuickSIN sentences presented at 45 dBHL in a calibrated soundfield with all hearing aids set to the same real-ear aided response. While this research on a small population does not prove that the most expensive hearing aids are no better for speech understanding in noise than their less-expensive counterparts, it does question the widely held clinical belief that the most expensive hearing aids provide the best speech recognition in noisy environments. It should also be acknowledged that speech understanding is not the only objective of speech-in-noise algorithms (ie, comfort, reduction of mental fatigue, etc, may also be important). However, these findings should encourage other audiologists to test this hypothesis on a larger scale (one research group, led by Robyn Cox, PhD, is currently studying this question36).
Accurately compute the long-term cost of hearing aids. Fabry37 showed that, despite manufacturer claims, the disposable hearing aids (Songbird in 2001) dispensed at Mayo Clinic Rochester averaged only 27 days of use before the battery quit. While this does not represent a large difference between the manufacturer’s reported 30-day battery life, it significantly affects the 3-year cost of one such disposable hearing aid. Specifically, a disposable hearing aid that requires replacement every 30 days at a cost of $90 per month would cost $3,240 in 3 years per ear. By contrast, a disposable hearing aid that lasts only 27 days would cost $3,780. Either way, the disposable hearing aid is maximally expensive and minimally featured. For that money, most hearing aids on the market could be purchased and expected to last at least 5 years.6
Educate the public about evidence-based practices. Since we are proposing people spend thousands of dollars on hearing aids when $90 disposable or $300 to $900 Internet hearing aids are available,38 proof of cost benefit is essential. Toward this end, we have hosted a monthly consumer-education group for the past 23 years. At these meetings, long-time hearing aid users answer commonly asked questions and we provide a rationale for real-ear aided testing and diagnostic hearing/balance tests. We routinely discuss the standards of evidence,39,40 and have developed an evidence-based hearing aid performance form that we put in the patient’s file and send to third-party payors.
Audiologists should serve as educators of people with hearing and balance disorders. Currently, that education is too often done by manufacturers and dispensing networks. We are in agreement with relevant conflict-of-interest sections of the Vanderbilt University Audiology Graduate Student Handbook41 and suggestions made by Cox39 to be wary of corporate information/influence, and instead do self-directed teaching, research, and thinking based on our extensive training.
Without a sufficient unbiased knowledge base, we cannot expect potential hearing aid candidates to spend hundreds or thousands of dollars on hearing aids, diagnostic tests, and rehabilitative therapy. The potential hearing aid candidate needs hearing care professionals to serve as educators, not sales representatives.
Summary
Numerous hearing aid cost-reduction programs exist. Typically, these programs require the audiologist to work at payment rates that are less than nationally established customary fees. To compensate for this reduced fee structure, these programs often sacrifice diagnostic validation and rehabilitative services.
The net result of some of these plans is that medical concerns related to hearing and balance disorders are disregarded, as these diagnostic tests are apparently not considered relevant to the sale of hearing aids. In fact, testing for the medical conditions we have mentioned above can delay the provision of hearing aids when positive findings are obtained.
Any attempt by audiologists to sell hearing aids at a price lower than the established fees for hearing and balance diagnostic/rehabilitative services and hearing aid performance tests cannot be sustained. Such medical and scientific neglect cannot produce a favorable outcome for persons with hearing and balance disorders or for audiologists.
Correspondence can be addressed to HR or Ron J. Leavitt, AuD, at .
References
- AARP Consumer Guide to Hearing Aids. Washington, DC: AARP. Available at: www.hearingloss.org/docs/aarphearing_guide.pdf. Accessed August 2, 2011.
- American Speech-Language-Hearing Association Preferred Practice Patterns for the Profession of Audiology. Rockville, Md: ASHA; 1997.
- Kochkin S. MarkeTrak VI. The VA and direct mail sales spark growth in hearing aid market. Hearing Review. 2001;8(12):24,63-65. Accessed August 2, 2011.
- Hear well in a noisy world. Consumer Reports. July 2009:32-37. Available at: www.consumerreports.org/health/healthy-living/home-medical-supplies/hearing/hearing-aids/a-shopping-summary/hearing-aids-shopping-summary.htm. Accessed August 2, 2011.
- Kochkin S. MarkeTrak VI: On the issue of value: hearing aid benefit, price, satisfaction, and repurchase rates. Hearing Review. 2003;10(2):12-26. Accessed August 2, 2011.
- Kochkin S. MarkeTrak VI: 10-year customer satisfaction trends in the US hearing instrument market. Hearing Review. 2002;9(10):14-25,46. Accessed August 2, 2011.
- Bantock HM, Croxson S. Universal hearing screening using transient otoacoustic emissions in a community health clinic. Arch Dis Child. 1998;78:249-252.
- Fortune H, Davis A. Epidemiology of permanent childhood impairment in Trent region, 1985-1993. Br J Audiol. 1997;31(6):409-446.
- Gallaudet Research Institute. Regional and National Summary Report of Data from the 2004-2005 Annual Survey of Deaf and Hard of Hearing Children and Youth. Washington, DC: Gallaudet University; 2005.
- Holden-Pitt L, Albertorio J. Thirty years of the Annual Survey of Deaf and Hard-of-Hearing Children and Youth: a glance over the decades. Am Ann Deaf. 1998;143(2):72-76.
- Van Naarden K, Decoufle P, Caldwell K. Prevalence and characteristics of children with serious hearing impairment in metropolitan Atlanta, 1991-1993. Pediatrics. 1999;103:570-575.
- Pichora-Fuller KM. Implications of cognitive factors for rehabilitation. ARC 2010: In with the Old—New Research on Aging and Hearing Health. Audiology Today. 2010;22(5):59-60.
- Ronnberg J, Rudner M, Foo C, Lunner T. Cognition counts: a working memory system for ease of language understanding (ELU). Int J Audiol. 2008;47(Suppl 2):S99-S105.
- Lunner T. Cognitive function in relation to hearing aid use. Int J Audiol. 2003;42:S49-S58.
- Kochkin S. Hearing loss and its impact on household income: a special report on new data generated by the Better Hearing Institute. Hearing Review. 2005;12(11):16-24.
- Kochkin S, Rogin C. Quantifying the obvious: the impact of hearing aids on quality of life. Hearing Review. 2000;7(1):8-34. Available at: www.betterhearing.org/pdfs/MR40.pdf.
- Kochkin S. BHI highlights importance of hearing health to Alzheimer’s patients during National Alzheimer’s Disease Awareness Month. Mental Health Behavioral Health Medical Professionals Resources 2010. Available at: behavioralhealthcentral.com/index.php/20101101240823/Top-Headlines/bhi-highlights-importance-of-hearing-health-to-alzheimers-patients-during-national-alzheimers-disease-awareness-month.html. Accessed August 2, 2011.
- American Speech-Language-Hearing Association. 2010 Medicare Fee Schedule and Hospital Outpatient Prospective Payment System for Audiologists. June 30, 2010. Available at: www.asha.org/uploadedFiles/10AudMPFS.pdf.
- Strom KE. The HR 2006 dispenser survey. Hearing Review. 2006;13(6):39. Accessed August 2, 2011.
- Killion MC, Niquette PA, Gudmundsen GI, Revit LJ, Banerjee S. Development of a quick speech-in-noise test for measuring signal-to-noise ratio loss in normal-hearing and hearing-impaired listeners. J Acoust Soc Am. 2004;116:2395-2405.
- Cox RM, Alexander GC, Xu J. Development of the Device-Oriented Subjective Outcome (DOSO) Scale. Paper presented at: American Auditory Society Annual Scientific Meeting; March 2009; Scottsdale, Ariz.
- Chisolm TH, Johnson CE, Danhauer JL, et al. A systematic review of health-related quality of life and hearing aids: final report of the American Academy of Audiology Task Force on the health-related quality of life benefits of amplification in adults. J Am Acad Audiol. 2007;18(2):151-183.
- Kochkin S. MarkeTrak VIII: Consumer satisfaction with hearing aids is slowly increasing. Hear Jour. 2010;63(1):19-32.
- Kochkin S. Reducing hearing instrument returns with consumer education. Hearing Review. 1999;6(10):18-20. Available at: 64.78.5.140/hia/publications/MR38.PDF. Accessed August 2, 2011.
- Penslar R. IRB Guidebook: Chapter IV. Consideration of Research Design. Washington, DC: US Department of Health and Human Services. November 9, 2009. Available at: www.hhs.gov/ohrp/archive/irb/irb_chapter4.htm. Accessed August 2, 2011.
- Abrams H, Hnath-Chisolm T, Guerreiro S, Ritterman S. The effects of intervention strategy on self-perception of hearing handicap. Ear Hear. 1992;13(5):371-377.
- Kricos P, Holmes A. Efficacy of audiologic rehabilitation for older adults. J Am Acad Audiol. 1996;7:219-229.
- Northern J, Beyer C. Reducing hearing aid returns through patient education. Audiology Today. 1999;11:2.
- Smaldino SE, Smaldino JJ. The influence of aural rehabilitation and cognitive style discourse on the perception of hearing handicap. J Am Acad Rehab Audiol. 1988;21:57-64.
- Hawkins DB. Effectiveness of counseling-based adult group aural rehabilitation programs: a systematic review of the evidence. J Am Acad Audiol. 2005;16(7):485-93.
- American Academy of Audiology (AAA). Guidelines for the Audiologic Management of Adult Hearing Impairment. Reston, Va: AAA. Available at: www.audiology.org/resources/documentlibrary/Documents/haguidelines.pdf.
- Hamill T, Freeman B. Scope of practice for audiologist assistants: survey results. Audiology Today. 2001;13(6):34-35.
- American Academy of Audiology. Position statement and guidelines of the consensus panel on support personnel in audiology. Audiology Today. 1997;9(3):27-28.
- American Academy of Audiology. American Academy of Audiology Position Statement: Audiology Assistants. Reston, Va: AAA. September 2010. Available at: www.audiology.org/resources/documentlibrary/Documents/2010_AudiologyAssistant_Pos_Stat.pdf. Accessed August 2, 2011.
- Leavitt RJ, Flexer CA. Audibility trumps all other hearing aid features. Seminar presented at: American Academy of Audiology Annual AudiologyNOW! Convention; April 2010; San Diego.
- Researchers to study effectiveness of hearing aids at different price points. Hearing Review online news, April 21, 2011. Available at: www.hearingreview.com/news/2011-04-21_01.asp. Accessed August 2, 2011.
- Fabry D. Disposable, starter and instant fitting hearing aids. Seminar presented at: American Academy of Audiology Annual AudiologyNOW! Convention; April 19-22, 2001; San Diego.
- Kochkin S. MarkeTrak VIII: Utilization of PSAPs and direct-mail hearing aids by people with hearing impairment. Hearing Review. 2010;17(6):12-16. Accessed August 2, 2011.
- Cox RM. Evidence-based practice in provision of amplification. J Am Acad Audiol. 2005;16:419-438.
- Valente M. Guideline for Audiologic Management of the Adult Patient. Audiology Online. October 30, 2006.
- Vanderbuilt School of Medicine Student Guide to the Department of Hearing and Speech Sciences (pages 37-40). Available at: www.mc.vanderbilt.edu/documents/GHSS/files/2011%20Handbook%20FINAL%208-15-11.pdf. Accessed September 28, 2011.
Citation for this article:
Leavitt R., Vossler C., Knowles L.: Cost-effective Pricing for Hearing Aids and Related Audiological Services Hearing Review. 2011;18(12):28-35.