Why people find it difficult to detect changes in their own hearing, and implications for hearing care providers.
Practice Management | December 2015 Hearing Review
Our traditional approach of labeling people as “in denial” clearly hasn’t been working, as evidenced by the minority adoption of hearing technology and the resistance experienced by hearing healthcare professionals in the initial appointment. We have a choice. We can continue as we have always done, looking for a future miracle in societal attitude change that will never happen. Or, we can start learning from the social sciences, which have been addressing issues like this for well over a hundred years.
The assumption of denial in the hearing care field is so well-established that it is seldom questioned, so when patients offer their own perspective—“My hearing’s not bad” or “I hear everything I want to hear” or “I find some situations a challenge” —it is automatically seen as evidence of their denial.1 This presupposition of denial leads to “rehabilitative” strategies that aim to break down a person’s resistance, where the perspective of two parties (HHP/Significant Other vs Client/Patient) are pitted against each another. The social sciences teach us that such an approach is likely to fail and even strengthen a person’s resistance.2 Ultimately, “people persuade themselves”3 and the role of the HHP should, therefore, be to facilitate that persuasion.
The purpose of this article is to provide practical insight into this putative denial, demonstrate how we can reframe it to better align with a patient’s own perspective, and examine implications for the provision of hearing healthcare. The result will be to create the necessary conditions—capability, opportunity, and motivation—for behavioral change (eg, the increased uptake of hearing technology) to take place.4
Part 1: Why it’s so difficult to perceive changes in hearing
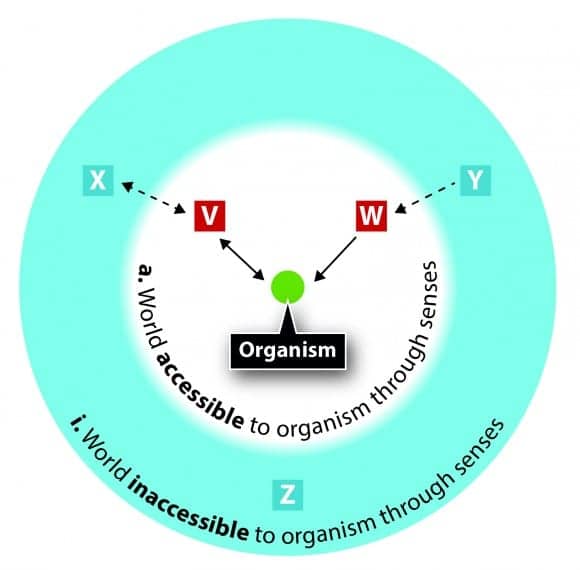
Challenge #1: You can’t perceive what doesn’t exist. There is a concept in the study of animal and human behavior called umwelt.5 It describes how our own perception of the world is shaped and limited by our senses (Figure 1), and “reality” will therefore differ from one organism to another. A bee’s reality, with its ultraviolet vision, will be very different from that of a shark equipped with electroreception, which will differ again from our own experience of the world as humans.
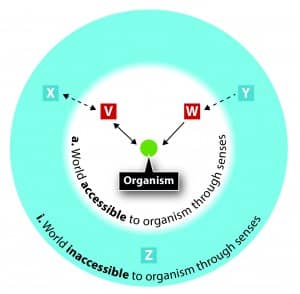
Figure 1. Every organism (eg, a bee, shark, human) experiences the world through its senses, which either make things accessible (a) or inaccessible (i). So [V] and [W] are things that are accessible to this organism. If the organism were a bee, then it may be the patterns on the flower that are accessible to it through its ultraviolet vision. The organism can interact with these things (bidirectional arrow shown between [V] and organism) or receive information from it (unidirectional arrow from [W]) The things [X], [Y] and [Z] are inaccessible to the organism through its senses. However, the organism may still be able to deduce their existence through its interaction with [V] and [W]. Applied to hearing, sounds such as bats or a dog whistle are inaccessible to us, so are represented by [Z], whereas the sound of a washing machine or human speech is accessible [V] and [W]. However, if our hearing range contracts, other sounds may also fall outside of our hearing range and become inaccessible [X] and [Y]. We may be able to deduce their existence only through their interaction with other people for whom they are accessible, or through information received through our other senses, or through previous experience (memory).
The exception is if we have some visual (or other sensory) indication to highlight the “non-existent” sound, such as a bird moving its beak with no sound emanating, or a violinist moving their bow across the strings in utter silence. But, for such events to occur at the precise moment our attention is directed towards them relies primarily on serendipity.
The other exception is if someone with us happens to hear a sound and comment on it, and we trust that person enough to believe they are telling us the truth, and there is nothing salient in the environment that could be considered a more “obvious” reason for not hearing it (eg, “My friend has exceptionally sharp hearing”)—the so-called Illusory Causation Effect.6-8 The probability of all three criteria being met is remote.
In each of these exceptions there is an underlying theme: the luxury of comparison. In the first case, the presence of the sound is deduced only by a comparison with information available from another sense, such as the visual system. In the second, we are comparing our experience with that of another human, our social system. In both cases, reliance is made on cognitive systems, such as associative and autobiographical memory, as well as theory of mind.
So, for another human being to tell us we are “in denial” is unfair and inaccurate. Because for us, it’s observation.
Challenge #2: Chasing a moving target. Sound, by its very nature, is a moving target. The same sound can be louder or quieter for all sorts of reasons. Experience tells us that some sounds on TV are quieter or louder than others, which is why we have a volume control. We also know that information contained in a signal can be weakened or distorted:
- People do sometimes mumble if, for example, they are shy9 or depressed.10
- The TV can sound distorted (eg, poor microphone placement during a recording, an old recording, etc).
- The environment can be echoic and smear speech.
- Enough noise will interfere with the signal through energetic and informational masking.11
- People do appear to speak more quickly today than “yesterday.” (For example, see: http://www.cbc.ca/news/canada/how-technology-is-turning-us-into-faster-talkers-1.1111667)
A lifetime of experience will inform us that any difficulties we may be experiencing with our hearing now is likely to be a further example of such situational factors.12 To counteract any compromise in the speech signal, we can employ the same compensatory measures that have worked for us in the past: move away from the noise, move closer to the signal, adjust the volume, and/or employ conversational repair strategies.13
We may need to use such measures more frequently, but who’s keeping count?
Challenge #3: Taking one for the team. Hearing works in partnership with a number of other systems, including the visual system,14,15 the cognitive system,16,17 and our social system.18 These three systems each contribute information from which the overall gestalt emerges, each seamlessly compensating, where possible, for any shortfall in the other systems:
- In background noise where the auditory signal is compromised, we look more intently (visual) at the face;19
- If someone coughs and it masks a word, we can fill in the missing word (cognitive) without even being aware of its absence;20,21
- In darkness, we pay more attention to the sounds (auditory), such as creaking floorboards, and
- If someone isn’t hearing us, we increase our volume, slow down, or repeat ourselves (social).
Such multimodal compensation can mask acute and chronic deficiencies in a single domain. So the fact that a conversation “flows” can be misinterpreted as evidence that our hearing is operating as expected. It’s not denial; it’s observation.
Challenge #4: Sneaking up on you? It’s no comparison. For most people, change in hearing is gradual with no accompanying symptoms (except, sometimes, tinnitus) to draw attention to it. For someone to perceive any change, it has to be possible to make a comparison between two different samplings taken at separate times. If the contrast between the samplings is too small, or the time between those samplings is too widespread, the change won’t be detected.
If we assume, for simplicity, that pure-tone thresholds increase approximately 1 dB every year,22 for someone to “deny a hearing loss” we are expecting the average person to perceive a daily change of 0.003 dB (1/365). Yet most people need a contrast of at least 1.5 dB before they can detect a difference,23 providing the sounds are presented in close succession.
For someone to detect a change in their own hearing would require them to accurately hold in memory exactly how they heard that same tone presented 18 months earlier, which isn’t realistic.
Challenge #5: Nothing wrong with the volume. Many hearing losses predominantly involve the higher frequencies, so the perception of volume is often subjectively maintained for the most commonly experienced sounds, namely:
1) The longterm average spectrums for speech and singing, which contains more energy in the frequencies below 1000 Hz.24,25
2) Many environmental noises, which tend to fall in the lower register, such as traffic and household appliances.
Furthermore, the perception of loud sounds is normally maintained in sensorineural hearing loss, and even increased through abnormal loudness growth, leading to the perception that one’s hearing is “too good, so why would I need amplification?”
Conclusions: Using observation to combat denial. Once we recognize that the problem is not primarily denial but observation, we can begin formulating a practical solution. It becomes clear that for someone to recognize change in their own hearing they need:
1) A baseline sampling of their hearing that can remain as a static measurement for future comparisons.
2) Routine monitoring at fixed time intervals that can be compared to the baseline.
Without these two things people will wait until they notice a change, which delays action. The exception, of course, is hearing that changes more rapidly. We will address both these issues below.
Part 2: Implications of the difficulty in perceiving changes in hearing
This inability to perceive changes in hearing has some important implications:
1) Lack of evidence decreases action. People are often unaware of changes in their own hearing unless they are presented with evidence that provides them with a credible comparison between what they manifestly hear and what they are expected to hear. This is what HHPs misinterpret as denial.
Ironically, “denial” can then later emerge as the result of sustained accusations of denial by HHPs and family. Work by Tomala et al26 on attitude certainty has shown that, if people successfully resist a strong attack on their own belief, then it makes them more likely to resist future attacks and act in a way consistent with the original attitude.
Applying this to hearing: if someone “observes” that their hearing is fine and can prove it to themselves when someone criticizes their hearing (Principles 1-5 above), once hearing is further reduced and good hearing becomes harder to justify, the earlier strengthening of the belief in response to the criticism, combined with “ego-defense” mechanisms,27,28 will result in making it harder to convince them of the need to use hearing technology.
2) Finger-pointing decreases action. We are more likely to recognize a change in another person’s hearing than we are in our own; if someone doesn’t hear us, we witness indicators that aren’t available to the person with reduced hearing. These include a) Having to increase our efforts in conversational repair, and b) incongruity in their response to us or to environmental signals.
3) Disbelief decreases action. Being told by someone else that our own hearing has changed, when we have no available evidence to suggest this, is likely to result in disbelief. The more we maintain this “reality,” the more we will look for—and find—evidence to confirm our conviction.12
And the more we do so, the more those disadvantaged by our reduced hearing will seek to put us straight! How we personally respond to their challenge will depend on a variety of factors, such as cognitive dissonance,29 which has the potential to further delay action.
4) Mildness decreases action. Those with milder hearing loss are less likely to perceive any reduction in their hearing ability because:
a) Their visual, cognitive, and social systems find it easier to compensate effectively for the shortfall in auditory information, thus maintaining the overall gestalt and impression that “everything is as expected.”
b) There are fewer events occurring in their everyday listening experience that present the necessary opportunities required for a comparison with expected hearing. For example, someone with a milder reduction will hear the washing machine, whereas someone with a moderate hearing loss may not. In the first case, the noise of the washing machine matches expectations so no comparison; in the second case, it doesn’t match and a comparison is triggered—assuming someone remembers what a washing machine should sound like and doesn’t assume that modern technology has developed silent washing!
c) The sounds they do hear will offer evidence that they are hearing as expected (Principle 5).
5) Isolation decreases action. People who live alone are likely to encounter fewer opportunities for comparison of their hearing and are therefore less likely to notice change, so the need for amplification will be harder to recognize, delaying appropriate action. Furthermore, motivating factors for taking action will be reduced without encouragement from communication partners.
To compound matters, socializing may be less enjoyable due to the stark contrast between their quiet world at home and the noisy world outside. There is, therefore, an increased risk of social isolation and/or loneliness, and subsequently a higher risk for depression,30 dementia,31,32 and even increased mortality.33,34,35
It should be noted that 33% of Baby Boomers are unmarried and that most unmarried Boomers live alone.36 This should be sounding alarm bells to our profession.
6) Delayed intervention decreases action. If someone’s hearing range has “always” been reduced (eg, congenital, acquired in early childhood, longstanding gradually acquired), they are less likely to perceive reduced hearing as they have no remembered experience to compare it with.
7) Rapid change increases action. Hearing that changes significantly enough over a short enough period of time is more likely to be noticed, and salience will be increased where a direct comparison is available, such as unilateral hearing loss (bilateral comparison) or sudden hearing loss (daily comparison).
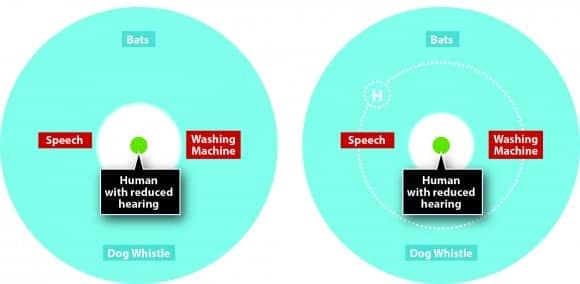
Figure 2. With a fluctuating hearing loss the thresholds transition between two points. If environmental sounds and speech are already falling below the threshold of hearing at the better hearing point (left diagram), then someone will be unable to notice the fluctuation (right diagram), just as they wouldn’t be able to detect if a dog whistle was louder or quieter. The fluctuation may only become evident once hearing technology (H) is fitted, which then extends the hearing range to encompass the previously inaccessible sounds. Now a comparison becomes possible, but the fluctuation in hearing may be mistaken for fluctuation in the performance of the technology.
8) Fluctuations harder to detect when hearing is worse. Fluctuating hearing loss may be imperceptible to an individual if their thresholds are elevated to the extent where they have no direct environmental or cognitive comparison available (see Figure 2). For example, if their better thresholds are already elevated to the point that static environmental sounds are already outside of their hearing range, these can’t be used as the initial sampling. When their hearing is then further reduced during fluctuation, they have no prior experience to compare the lower thresholds with. In such case, self-reported fluctuating hearing loss may be impossible and might only become manifest once hearing technology is fitted. Even then, the fluctuation may be mistaken for variable performance of the hearing device.6-8
Part 3: Implications for hearing assessments and adoption of hearing technology
1) Action trigger cannot depend on self-recognized hearing loss. If the primary motivation for getting hearing checked is because people notice a problem with their hearing, then the majority are unlikely to do so as most people simply don’t have the capability to detect the change. This applies regardless of whether a hearing check is with a doctor, a hearing healthcare professional, or using a Smartphone app.
For example, what would be the motivation for downloading an app for checking our own hearing? Or taking time out of a busy schedule to leave what we are currently doing to visit a website that has an online hearing check? Curiosity? Perhaps. But this cannot be expected of the vast majority of society who don’t share our professional interest in hearing. We need something more: people must be given some other reason to get their hearing checked. And telling people they are in denial is not the answer.
It is interesting to note that, in the United Kingdom, 63% of people with self-reported hearing loss say that they will begin using hearing technology “when their hearing gets worse.”37 In other words, people are looking for a trigger that, in most cases, won’t exist. It’s equivalent to saying that we’ll only answer the door if the doorbell rings, even if we don’t own a doorbell! It doesn’t mean nobody has come to our door and rung the bell; it simply means we don’t have the ability to detect it.
It should also be emphasized that, while the promotion of PSAPs may be seen by some as one way to make hearing technology accessible to more people (whatever its other advantages/disadvantages may be), PSAP use still relies on people actually noticing a change in their hearing, and as explained earlier, this is less likely for people with milder hearing loss—which is where PSAPs are positioned. PSAPs are, therefore, unlikely to have a significant impact on increasing the overall adoption rate of hearing technology for factors other than affordability.
2) Action resulting from noticeable change is a red-flag. When change is noticeable, it will increase the likelihood of seeking some form of intervention (eg, professional advice, traditional hearing technology, PSAPs). But, as we saw above, noticeable change is the exception, rather than the norm. It usually means:
a) Either a perceptible contrast has developed (eg, sudden/rapid onset, or asymmetry), which usually indicates an underlying referable condition.
b) Or that reduction in hearing has already become severe enough, which means that a delay in intervention has already taken place.
It should be stated that the absence of noticeable change does not exclude the possibility of an underlying referable condition (eg, otosclerosis), nor does it mean that someone’s hearing has not yet become “severe enough” to warrant intervention.
Noticeable change has important consequences for the advice we give the public. If we say that bypassing a trained hearing expert (eg, “self-screening” or “using a PSAP is sufficient”) is acceptable behavior for people who notice changes in their hearing, then we are increasing the risk to their health and well being, unless:
a) We have a robust method for ruling out the possibility of an underlying condition.
b) We have evidence that non-involvement of a hearing healthcare professional in the longer term management of “easier-to-notice” hearing loss is as effective for individuals and society as the involvement of a professional following best-practice protocols.
Consider the following scenario: Someone lies with their head on one side, one ear pressed into the pillow. They then try it with the opposite ear, and notice a clear difference in environmental sounds. This could be a sign of an asymmetry. They have neither the equipment nor training to know the degree or cause of the asymmetry—only that they’re not hearing as well.
If the public advice is “if you notice problems with your hearing, you can get an over-the-counter PSAP or download an app,” this is more affordable and easier than arranging to see the appropriate specialist. They try it, and it alleviates the effects of the hearing loss enough to dampen the motivation to take action. Meanwhile the underlying condition worsens (eg, a growth) or becomes less susceptible to reversal (eg, sudden sensorineural hearing loss).
Part 4: Implications for Hearing Care Professionals and Policy Makers
Action Point #1: Shift your frame from “denial” to observation. First and foremost, we must stop telling ourselves that people are in denial, and begin seeing this through the eyes of the people we serve: as observation. Their observation may be “wrong” compared to how we see things—and how their families see things—but telling someone they are wrong goes against every principle of effective persuasion, and is likely to increase resistance. Furthermore, it risks damaging a person’s self-identity and self-esteem, and that makes the rehabilitation process far harder.38
Instead, when we see it as observation, and we look at what people need in order to recognize a change in their hearing, we can begin designing our services accordingly. We conduct our appointments differently. We encounter less resistance. Our goal is not to convince someone they have hearing loss. Instead, it is to enable them to bring sound back within their hearing range so they don’t lose out. This immediately better aligns with their own goals, because people are motivated to avoid loss and seek gain.39,40
Action Point #2: Don’t wait for people to notice a problem. It is absurd for us to wait until people recognize a change in their own hearing, then wonder why more people aren’t using hearing technology!
The detection of a reduction in hearing obviously precedes the use of hearing technology; yet most hearing care provisions focus solely on hearing aids, and many hearing care providers (and manufacturers) see hearing checks as being a “waste of time” or a failure unless they directly lead to a fitting. We have been putting the cart before the horse, then wondering why we haven’t moved forward in increasing the uptake of hearing technology!
As explained earlier, to detect change we need at least two samplings: a baseline, and a deviation from that baseline. People often don’t have that luxury “in the real world” because hearing changes gradually. It’s up to the HHP to provide it for them by:
1) Offering a baseline hearing check so people have a starting point; and
2) Routinely monitoring it every 5 years (if they are hearing as expected), or more regularly if there is a reduction.
In the first case, we attract two types of people: those with good hearing, and those who think they have good hearing. In the past, these individuals haven’t visited a HHP because they believed their hearing wasn’t “bad enough” to warrant it, because the focus was on poor hearing. Yet these are many of the individuals who would benefit from hearing technology, but haven’t acted—which means, by offering a baseline, we begin tapping into some of those 3 out 4 of people we currently leave behind.41
Additionally, the individuals who have good hearing are:
1) Being exposed to hearing healthcare, which builds trust and liking;42
2) Increasing the importance of their hearing through their actions;43
3) Educating themselves about auditory well-being and updating social attitudes to hearing technology;
4) Becoming more likely to be messengers to others in society about the benefits of hearing care (“keeping your hearing at its best”);
5) Creating “social proof” that encourages others to have their hearing checked, including those who would benefit from hearing technology,44,45 and
6) Helping to offset the overheads of running a practice (unless the hearing check is free) by spreading the cost over a greater number of individuals, so that the cost of hearing technology becomes more affordable.
In the second case, routine monitoring establishes a habit that involves a qualified professional, like a dentist or optician. More importantly, we are providing a comparison for people, which as we’ve seen is essential for recognizing change. If they come the first year with a slight reduction in hearing that wouldn’t measurably benefit from hearing technology, but on the re-assessment the hearing has changed, the contrast between the two audiograms will help to persuade someone to “bring sounds back within their hearing range” (ie, prevention of future loss).
When done properly, offering baseline hearing checks and routine monitoring “throughout life” will do more to increase the uptake of hearing technology and prevent noise-induced hearing loss than any other measure. (The other two most important measures being affordability/accessibility and the avoidance of stereotyping.)
Action Point #3: Make hearing checks about well-being, not loss. As explained earlier, we have to give people a motivation for getting their hearing checked that doesn’t rely on noticing a change in hearing. Our message must present hearing checks as a normal part of health and well-being, rather than for singling out “abnormality.”46
So our message must not focus on a specific demographic (eg, age 50+, 60+, or the “hearing impaired”). Instead it must be seen as applying to everyone (ie, ageless) and “normal”—otherwise we stigmatize those who respond.
This means shifting the meaning of the hearing assessment from “detecting hearing loss” to “maintaining maximal hearing” (and the implications of this). Note that we are shifting the meaning of hearing care away from trying to “fix/correct/treat the condition of the ear” and to maintaining the auditory connection between the external (social) world and the internal (psychological) world, or psychosocial well-being. Such a message has universal (and topical) appeal: it means being all that you can be,47,48 and hearing plays an integral role in this (for reasons that would require a separate article).
Here are two simple ways we can present such a message:
Eyes checked. Teeth checked. Hearing checked. We all know how important it is to get our eyes and teeth checked regularly. The same is true of our hearing. For most of us, it’s the only way to detect changes before our hearing loss becomes a problem to others. Hearing is our 24/7 connection to all that is happening in the moment. We should check it every 5 years (at 20, 25, 30 years, etc) to prevent our connection fading away.
Hear to stay. Not fade away. You don’t need anyone to tell you how integral hearing is to every aspect of life. No wonder that people who don’t regularly check their hearing are more at risk of fading away.
Conclusions
Our traditional approach of labeling people as “in denial” clearly hasn’t been working, as evidenced by the minority adoption of hearing technology and the resistance experienced by HHPs in the initial appointment.
We have a choice. We can continue as we have always done, looking for a future miracle in societal attitude change that will never happen. Or, we can start learning from the social sciences, which have been addressing issues like this for well over a hundred years.49
For people to change their behavior, they need the capability, motivation, and opportunity to do so.4 If the target behavior is to use hearing technology, they first need to recognize the need for the technology. But we have seen that most people don’t have that capability because it’s virtually impossible to notice changes in one’s own hearing. So we must give them the capability, and the most logical way to do this is by offering a baseline hearing check (the initial sampling), followed by routine hearing checks throughout life (comparative samplings).
We must then give people the motivation, and this must align with their own goals and self-concept. Otherwise, we create resistance —which is what we have been doing all these years with our accusations of denial. Instead, we reframe the hearing check from the detection of loss (with its concomitant stigmatization of the minority) to the maintenance of well-being through maximal hearing.
Finally, we must give people the opportunity to have their hearing checked—and not just when they suspect a need for hearing technology. Otherwise, we miss all those who could be benefiting but don’t have the capability to recognize it. And isn’t that where the increased uptake must come from?
References
-
Kochkin S. MarkeTrak VII: Obstacles to adult non-user adoption of hearing aids. Hear Jour. 2007;60(4):24-51.
-
Knowles ES, Linn JA. Resistance and Persuasion. Abingdon, Oxon, UK: Taylor & Francis Psychology Press;2004.
-
Perloff RM. The Dynamics of Persuasion: Communication and Attitudes in the Twenty-first Century. Abingdon, Oxon, UK: Taylor & Francis Psychology Press;2010.
-
Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Sci. 2011;6(1):42.
-
Von Uexküll J. (2014). Umwelt und innenwelt der tiere. Springer-Verlag.
-
Lassiter GD, Geers AL, Munhall PJ, Ploutz-Snyder RJ, Breitenbecher DL. (2002). Illusory causation: Why it occurs. Psychological Science, 299-305.
-
McArthur LZ. (1980). Illusory causation and illusory correlation: Two epistemological accounts. Personality Soc Psych Bulletin. 6; 507–519.
-
McArthur LZ. (1981). What grabs you? The role of attention in impression formation and causal attribution. In Higgins ET, Herman CP, Zanna MP (Eds). Social cognition: The Ontario symposium (Vol. 1, pp. 201–241). Hillsdale, NJ: Erlbaum.
-
Zimbardo PG, Pilkonis P, Norwood R. (1977). The Silent Prison of Shyness (No. TR-Z-17). Stanford Univ Calif Dept Psych.
-
Mundt JC, Snyder PJ, Cannizzaro MS, Chappie K, Geralts, DS. (2007). Voice acoustic measures of depression severity and treatment response collected via interactive voice response (IVR) technology. Journal of Neurolinguistics. 20;(1): 50–64. http://doi.org/10.1016/j.jneuroling.2006.04.001
-
Brungart DS, Simpson, BD, Ericson MA, Scott KR. (2001). Informational and energetic masking effects in the perception of multiple simultaneous talkers. Jour Acous Soc Am. 110;(5): 2527-2538.
-
Nickerson RS. (1998). Confirmation bias: A ubiquitous phenomenon in many guises. Rev Gen Psych. 2;(2): 175.
-
Lind C, Hickson L, Erber NP. (2004). Conversation repair and acquired hearing impairment: A preliminary quantitative clinical study.
-
McGurk H, MacDonald J. Hearing lips and seeing voices. Nature. 1976;(264):746–748.
-
Stein BE, Stanford TR. (2008). Multisensory integration: current issues from the perspective of the single neuron. Nature Reviews Neuroscience. 9;(4):255-266.
-
Zekveld AA, Heslenfeld DJ, Festen JM, Schoonhoven R. (2006). Top–down and bottom–up processes in speech comprehension. NeuroImage. 32;(4):1826-1836.
-
Mattys SL, Davis MH, Bradlow AR, Scott SK. (2012). Speech recognition in adverse conditions: A review. Language and Cognitive Processes. 27;(7-8):953-978.
-
Hayashi M, Raymond G, Sidnell J. (2013). Conversational repair and human understanding (Vol. 30). Cambridge University Press.
-
Sumby WH, Pollack I. Visual contribution to speech intelligibility in noise. J Acoust Soc Am. 1954;(26);212–215.
-
Warren RM. (1970). Perceptual restoration of missing speech sounds. Science. 167;(3917):392-393.
-
Warren RM, Obusek CJ. (1971). Speech perception and phonemic restorations. Perception & Psychophysics. 9;(3): 358-362.
-
Lee FS, Matthews LJ, Dubno JR, Mills JH. (2005). Longitudinal study of pure-tone thresholds in older persons. Ear and hearing. 26;(1):1-11.
-
Forinash K. An Interactive eBook on the Physics of Sound. https://soundphysics.ius.edu/?page_id=914
-
Byrne D, Dillon H, Tran K, Arlinger S, Wilbraham K, Cox R, Ludvigsen C. (1994). An international comparison of long?term average speech spectra. J Acoust Soc Am. 96;(4):2108-2120.
-
Monson BB, Lotto AJ, Story BH. (2012). Analysis of high-frequency energy in long-term average spectra of singing, speech, and voiceless fricatives. J Acoust Soc Am. 132;(3):1754-1764.
-
Tormala ZL, Petty RE. (2002). What doesn’t kill me makes me stronger: the effects of resisting persuasion on attitude certainty. J Personality and Soc Psych. 83;(6):1298.
-
Katz D, Sarnoff I, McClintock C. (1956). Ego-defense and attitude change. Human Relations.
-
Knight Lapinski M, Boster FJ. (2001). Modeling the ego-defensive function of attitudes. Communication Monographs. 68;(3):314-324.
-
Festinger L. (1957). A Theory of Cognitive Dissonance. Evanston, IL: Row, Peterson.
-
Golden J, Conroy RM, Bruce I, Denihan A, Greene E, Kirby M, Lawlor BA. (2009). Loneliness, social support networks, mood and wellbeing in community-dwelling elderly. Intl J Geriatric Psychiatry. 24;(7):694-700.
-
Holwerda TJ, Deeg DJ, Beekman AT, van Tilburg TG, Stek ML, Jonker C, Schoevers RA. (2014). Feelings of loneliness, but not social isolation, predict dementia onset: results from the Amsterdam Study of the Elderly (AMSTEL). J of Neurol, Neurosurg & Psychiatry. 85;(2):135-142.
-
Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Barnes LL, Bennett DA. (2007). Loneliness and risk of Alzheimer disease. Arch of General Psychiatry. 64;(2):234-240.
-
Steptoe A, Shankar A, Demakakos P, Wardle J. (2013). Social isolation, loneliness, and all-cause mortality in older men and women. Proc Nat Acad Sci. 110;(15):5797-5801.
-
Cacioppo JT, Hawkley LC, Norman GJ, Berntson GG. (2011). Social isolation. Annals NY Acad Sci. 1231;(1):17-22.
-
Contrera KJ, Betz J, Genther DJ, Lin FR. Association of Hearing Impairment and Mortality in the National Health and Nutrition Examination Survey. JAMA Otolaryngol Head Neck Surg. Published online September 24, 2015. doi:10.1001/jamaoto.2015.1762.
-
Lin IF, Brown SL. 2012. “Unmarried Boomers Confront Old Age: A National Portrait.” The Gerontologist. 52;(2):153-165.
-
EuroTrak 2012, 2015.
-
Steele CM. (1988). The psychology of self-affirmation: Sustaining the integrity of the self. Advances Exper Soc Psych. 21;(2):261-302.
-
Updegraff JA, Sherman DK, Luyster FS, Mann TL. (2007). Understanding how tailored communications work: The effects of message quality and congruency on perceptions of health messages. Jour Exper Soc Psych. 43; 248-256.
-
Kahneman D, Knetsch JL, Thaler RH, (1991). The Endowment Effect, Loss Aversion, and Status Quo Bias. Jour Econ Perspectives, 1991;(5):193-206.
-
Kochkin S. (2009). MarkeTrak VIII: 25-year trends in the hearing health market. Hearing Review. 16(11), 12-31; Kochkin S. (2014). A Comparison of Consumer Satisfaction, Subjective Benefit, and Quality of Life Changes Associated with Traditional and Direct-mail Hearing Aid Use. Hearing Review. 21;(1):16-26.
-
Zajonc RB. (1968). Attitudinal effects of mere exposure. Jour Pers and Soc Psych. 9;(2): 1.
-
Bem DJ. Self-Perception Theory. In Berkowitz L (Ed). Advances Exper Soc Psych. 1972;(6):1-62. San Diego, CA: Academic Press.
-
Cialdini RB, Trost MR. Social influence: Social norms, conformity, and compliance. In Gilbert DT, Fiske ST, Lindzey G (Eds). The handbook of social psychology, 4th ed. 1998;(2):151-192.
-
Cialdini RB. (2009). Influence: Science and Practice (5th ed), Chapter 4.
-
Goffman E. (1963). Stigma: Notes on the Management of Spoiled Identity, Chapter 2. Simon & Schuster.
-
Maslow AH. (1943). A theory of human motivation. Psych Review, 50;(4), 370.
-
Deci EL, Ryan RM. (2002). Handbook of self-determination research.
-
Briñol P, Petty RE. (2012). The history of attitudes and persuasion research. In Kruglanski A, Stroebe W (Eds). Handbook of the history of social psychology (pp. 285-320). New York: Psychology Press.
-
Lin F, Metter E, O’Brien R, Resnick S, Zonderman A, Ferrucci L. Hearing loss and incident dementia. Arch Neurol. 2011;68(2):214-220.
-
Lakatos P, Chen CM, O’Connell MN, Mills A, Schroeder CE. Neuronal oscillations and multisensory interaction in primary auditory cortex. Neuron. 2007;53(2):279–292.
-
Sams M, et al. Seeing speech: visual information from lip movements modifies activity in the human auditory cortex. Neurosci Lett. 1991;127(2):141–145.
Curtis Alcock is a hearing care professional from Exeter, England, who has written and lectured extensively on the need to change the language, imagery, and marketing in hearing healthcare. In 2010, he founded Audira, an online think tank for hearing intended to bring together like-minded individuals and organizations who all have the same goal: to instigate change in society’s relationship to hearing care.
Correspondence can be addressed to HR or Curtis Alcock at: [email protected]
Original citation for this article: Alcock C. It’s Not Denial. It’s Observation. Hearing Review. 2015;22(12):16.






Hi Curtis:
I just read your article “It’s Not Denial. It’s Observation.” Wow! One of the best articles I’ve read.
The three points you make that really resonated with me were:
1. Instead, when we see it as observation, and we look at what people need in order to recognize a change in their hearing, we can begin designing our services accordingly. We conduct our appointments differently. We encounter less resistance. Our goal is not to convince someone they have hearing loss. Instead, it is to enable them to bring sound back within their hearing range so they don’t lose out. This immediately better aligns with their own goals, because people are motivated to avoid loss and seek gain.
2. As explained earlier, to detect change we need at least two samplings: a baseline, and a deviation from that baseline.
3. Make hearing checks about well-being, not loss. Eyes checked. Teeth checked. Hearing checked.
I am CEO of Clear Digital Media and ClearSounds Communications. We have been working with hearing care professionals for over 30 years and, year after year, have heard the same discussions and conversations around the anemic growth and adoption of solutions.
Our business provides a platform for the hearing industry to reach consumers with compelling content that speaks directly to your point and one of the top 3 take-aways: “Make hearing checks about well-being.” Our digital content platform delivers this very message in video format to consumers as they sit in the waiting room at their physician’s office. We also provide patient engagement systems for the hearing professional practice that reiterates these messages in video format in the waiting room. We recently conducted a consumer impact study that presented this very conclusion–people simply do not think about hearing checks as routine…ever. Encouraging the establishment of a baseline is such a clear concept to explain. How will you know what might be changing if you never establish a baseline?
Excellent information Curtis! Thank you for your fantastic work.
An excellent article Curtis. Until we have a ‘tool’ that is sensitive to change that can be reliably used for the hearing check or screening it is going to be difficult to move forward. The pure tone audiogram is simply not accurate enough, and there are too many variables in it’s delivery, not to mention the +/- 5dB accuracy (at best!). You mention that some may use a hearing check app or online test out of curiosity, and I think that this is correct, but also bear in mind that with everyone being so ‘busy’ it is maybe easier for them to do a ‘self-check’? This then raises the question of the course of action an individual considers if they subsequently do not do well on this check… If, and when, a tool is developed which is easy to deliver, AND provides repeatable results, AND provides a clear pathway for action, then I believe we will have turned a (big) corner.
Hi Gary, thanks for the feedback.
I think there are two things here: 1) The ideal we should be aiming for; 2) What we can be doing now with what we already have.
Sometimes what we don’t yet have (i.e. the ideal we should be aiming for) can induce a feeling of helplessness as a profession: we can feel so far away from where we want to be that we feel we can’t move forward until other things have taken place.
The danger of this is that we continue to wait and wait for things to change, and because we’re all waiting, nothing ever does. Think about how long as a profession we’ve been talking about things like speech in noise testing, but still can’t agree on a standard! We also have otoacoustic emissions that is sensitive enough to pick up noise damage when an audiogram can’t, but they’ve still not become standard.
Yet the one thing that everyone everywhere can agree on is Puretone Audiometry (PTA). Not only has stood the test of time, but we base our fitting prescriptions on it! Not on speech testing, not on speech in noise testing; the humble audiogram. We even use it to decide whether a condition should be referred (because of comparisons to other PTA). And this is despite its inherent limitations.
But I think as a profession we often assume that the PTA pretends to be more than it is. All it’s supposed to do is say whether a sound falls within a person’s hearing range, or it doesn’t (the concept of “just noticeable” is used in other psychophysics). It’s not supposed to say what someone actually does with the sound, or the quality of the sound, or the intelligibility of speech, or whether they can derive meaning from it (as important as these all are).
So we might think of the PTA as a test to say “You have access to this sound; you don’t have access to this one”. If we have ACCESS to a sound (i.e. within our umwelt), we have the first step in being able to do something with that sound. If we don’t have access to it, then we can’t (begin) to use it. (Like humans and ultraviolet light.)
In terms of the ±5dB, it’s worth remembering that sounds themselves, by their very nature, are transient and fluctuate in intensity. (“Missed is seeing, quickly glance; Missed it hearing; lost your chance.”) Sometimes someone will speak to us at an average of 55dB; sometimes at 60dB. That can be a ±5dB difference.
So when it comes to sound (and the sense we’ve “developed” specifically for detecting it) it’s inherently variable; it is the nature of the beast. So perhaps it’s natural to assume there will be “inaccuracies” in any test we do; it’s possibly a reflection of sound as a medium. Will it ever be otherwise in our tests? I wonder. That’s why we tend to base things on “norms”, which of course incorporate such variation within its own distribution curve.
So the PTA, carried out according to an agreed method on equipment calibrated to an agreed specification and interpreted by people who are trained to an agreed standard and comparing the audiogram to an agreed set of norms, is (I would argue) a perfectly suitable test for measuring a baseline, then monitoring changes over time compared to that baseline. After all, how small do the changes in an inherently variable medium need to be, before they are significant?
The question is how we USE that test (and interpret it – but that’s for another article). And I believe that we could be using the PTA more effectively. How?
1) By using it as a tool for assessing ACCESSIBILITY to sound, rather than for the detection of hearing loss.
2) By promoting BASELINE hearing checks, followed by routine monitoring – rather than WAITING until someone notices a problem with their hearing.
We know that not everyone is going to have the time to get their hearing checked regularly. But at the same time we know that not everyone will visit the dentist regularly. Or stick to the speed limit. Or eat 5 fruit/veg a day. Or need to use their seatbelt But at least with these things we know what we SHOULD be doing. So that when those things become relevant to us, we have proper guidance from the experts. We also know that with all these things there will be variation within the population in terms of what’s best for that individual, but the advise is generalised by once again relying on “norms”.
But within hearing care, we’ve been so fluffy with our guidance! We tell people to get their hearing checked if they “notice a problem with their hearing”, and then when they don’t come forward we say they’re in denial, when actually all they’re doing is following our advice(!) – because they DIDN’T notice any problems (for all the reasons explained in my article above).
So why don’t we just come clean with the public and tell them outright, you CAN’T (normally) notice changes in your hearing*. That’s why we all need a baseline for our hearing, plus routine monitoring. And we should tell the public, “If you say you have good hearing but you’ve not had it checked in the past five years, do you realise you are saying exactly the same as someone whom everyone knows is mishearing but can’t recognise it themselves. So how do you know YOU’RE not mishearing? You can’t, not without a routine hearing check.”
Personally I believe we can do all this without needing to wait for a different, more sensitive test. It’s something we can all do now that will contribute to creating the necessary conditions for attitudes to change. Yes, it’s only part of the solution. But it’s a vital one. And a step forwards towards the greater ideal.
(*So if you do notice, seek professional help immediately.)