Research | October 2021 Hearing Review
Toward testing and clinical management of this unique patient population
By Andrea Dunn, AuD, PhD; Philippa James, AuD; Angela Pelosi, MAuDA; Eldon Sorensen; and Jacob Oleson, PhD
Although auditory issues have been consistently identified among the most common parent-reported sensory issues affecting children with ASD, audiologists rarely evaluate complex listening ability during clinical appointments. The disconnect between patients’ presenting complaints and the conventional test battery may stem from limited knowledge of the listening challenges common to patients with ASD or the range of available management options. This study examines testing in a group of children with ASD and normal hearing sensitivity, and introduces a remediation-driven streamlined assessment as well as a management matrix tailored to each distinct pattern of performance on auditory tests.
When assessing a patient with Autism Spectrum Disorder (ASD), most clinical audiologists rely on pure-tone audiometry and traditional tools to document hearing status. However, conventional audiometry may have limitations given the striking contrast between the high rate of parent-reported listening issues1 and lack of conclusive evidence of increased risk of peripheral hearing loss in this population.2 This dichotomy between reported and measured auditory problems has spurred further investigation into the assessment and management of functional listening deficits in individuals with ASD.
In a study of over 400 parents of children with ASD, auditory filtering deficits (eg, reduced auditory responsiveness, difficulty attending to auditory stimuli in noise, distractibility, etc) were reported in more than 50% of children with ASD.1 These parent-reported auditory difficulties have been corroborated with behavioral, objective, and qualitative evidence of disproportionately poor performance on complex auditory tests. For example, research shows that children with ASD have poorer auditory temporal processing,3,5 reduced speech recognition-in-noise ability,3,4,6 and higher hearing disability ratings3 compared to neurotypical peers.
Fortunately, management options are available to mitigate listening issues. Remote microphone (RM) technology has been shown to improve speech understanding4,7-9 and listening behavior,3,7-9 and auditory training shows promise for addressing binaural processing abnormalities.7,10-11
Remote-Microphone System Benefits on Listening
There is substantial prior evidence of improved speech recognition in noise and over distance for normal-hearing listeners with versus without RM, as well as recent data showing RM benefits in individuals with ASD and normal hearing. Among study findings, researchers have reported that soundfield (SF) classroom systems can improve functional hearing in some preschoolers with ASD and low-language by reducing response latency or the level of prompting needed for a response.12 Soundfield classroom and personal RM benefits have also been observed in older children, including increased speech recognition-in-noise accuracy,4,7-9 improved parent- and teacher-reported behavior,3,7-9 and reduced listening stress.8 Despite this, at present, many hearing healthcare providers are unable to meaningfully intervene to address the listening needs of children with ASD because traditional audiological tests like speech testing in quiet are less reflective of real-world, functional listening challenges.13
In the current article, clinical data is summarized from 41 children with ASD and normal pure-tone thresholds who presented to the University of Melbourne ASD Listening Clinic with auditory concerns. Their performance is characterized on a battery of clinical tests, and scores are compared across measures. A streamlined recommended assessment protocol is introduced that includes only those measures that were clinically feasible with most participants and that contributed to participant-specific management decisions. A clinical management matrix is also provided offering recommendations that are tailored to each distinct pattern of performance on auditory tests.
Study Methods and Results
Ethical approval for this research was obtained from the University of Melbourne Human Ethics Research Committee. The 41 children represented in the current study ranged in age from 6 to 14 years, had documentation of ASD diagnosis from a qualified healthcare provider, no known cognitive impairment, were native English speakers, and were able to communicate verbally.
Testing was completed during a single 1.5-hour visit. Conventional pure-tone hearing testing and tympanometry was administered first to confirm normal hearing sensitivity and middle-ear health prior to proceeding with any other measures. The test battery included measures previously identified as sensitive to auditory deficits in children with ASD.14 These tests were completed in the following prioritized order:
- High-cue condition of the Listening in Spatialized Noise – Sentence (LiSN-S) test,15
- Dichotic Digits Test,16 and
- Integrated Visual and Auditory Quick Screen Continuous Performance Task (IVA-QS CPT).17
Two questionnaires were also completed by parents:
- Short Sensory Profile 2 [SSP]18 for assessment of global sensory processing, and
- Listening Behaviors in Autism Scale [LBAS]19 for assessment of functional auditory skills.
Individual participant scores were compared to age-matched, test-specific normative data to distinguish normal versus abnormal performance, and the total proportion of abnormal scores was computed for each test. The rate of observed abnormal scores in participants with ASD was compared to the rate of expected abnormal scores in a neurotypical population. Consistent with previous research,14 significantly higher fail rates were identified on all tests (Figure 1).
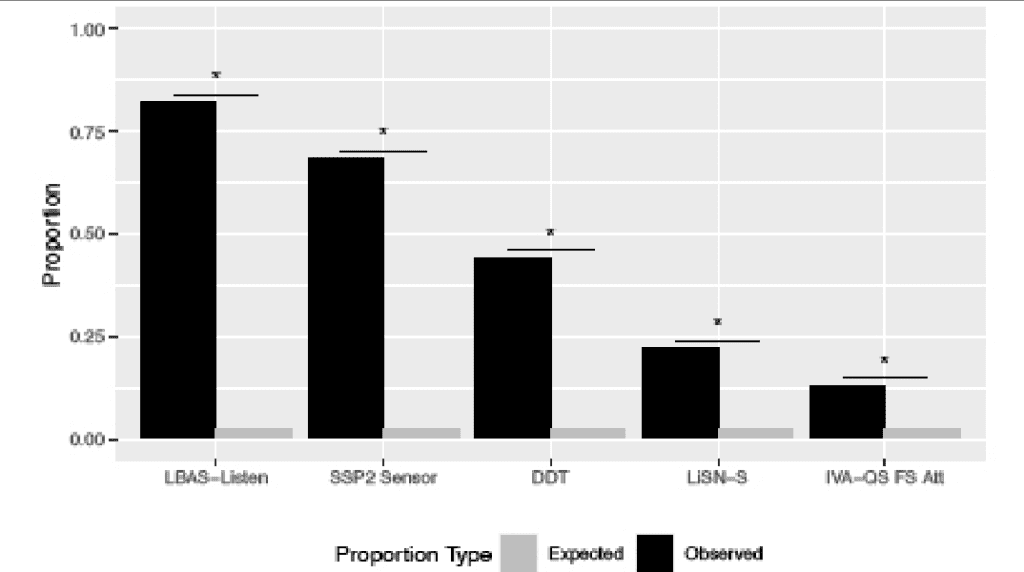
Figure 1. Comparison of the proportion of observed auditory spectrum disorder (ASD, black bars) versus expected (neurotypical, gray bars) abnormal scores on each test. *P-value < 0.05.
Follow-up analyses were performed to compare results across tests. A positive relationship was identified between DDT and LiSN-S scores (r = 0.45) such that poorer dichotic listening was associated with poorer speech recognition in noise. Scores on the LBAS (auditory-specific) and SSP2 (global sensory) were also positively correlated (r = 0.43), which may indicate that auditory features are a key component of global sensory processing deficits or the multisensory nature of sensory processing alterations.
Somewhat surprisingly, no significant correlation was found between parent-reported functional listening deficits on the LBAS questionnaire and the LiSN-S or DDT, which suggests that clinical tests may underestimate parent- and participant-reported real-world challenges or offer distinct information about complex listening and real-world functioning.
Attention scores on the IVA-QS were not correlated with performance on any other measures, suggesting that attention problems cannot fully account for dichotic or speech-in-noise deficits.
A Streamlined Assessment that Informs Clinical Management
To develop a streamlined recommended assessment battery, the original five tests were considered based on their ability to detect auditory deficits in children with ASD, clinical feasibility, and independent contribution to management recommendations. Subsequently, the IVA-QS test was eliminated because of limited clinical feasibility relative to other measures and reduced influence on management decisions. Test administration was lengthy, and 58% of participants already had documented diagnoses of attention deficits from outside testing. Furthermore, there is currently no published data showing the benefit of auditory training or technology on attention as measured via the IVA-QS and no correlation between this and other measures (eg, dichotics, speech-in-noise) where documented performance benefits have been observed with these interventions.
The second test eliminated from the streamlined assessment battery was the Sensitivity/Sensory subscale of the SSP2. The SSP2 questionnaire is widely used with children with ASD and although the sensitivity/ sensory subscale contains many auditory-relevant questions, it also encompasses non-auditory processing areas (eg, tactile responsiveness). The SSP2 and LBAS were positively correlated, suggesting a relationship between auditory functioning and broader sensory processing capabilities. However, given the greater auditory specificity of the LBAS, it was determined to be more useful for informing patient management. Thus, the SSP2 was removed.
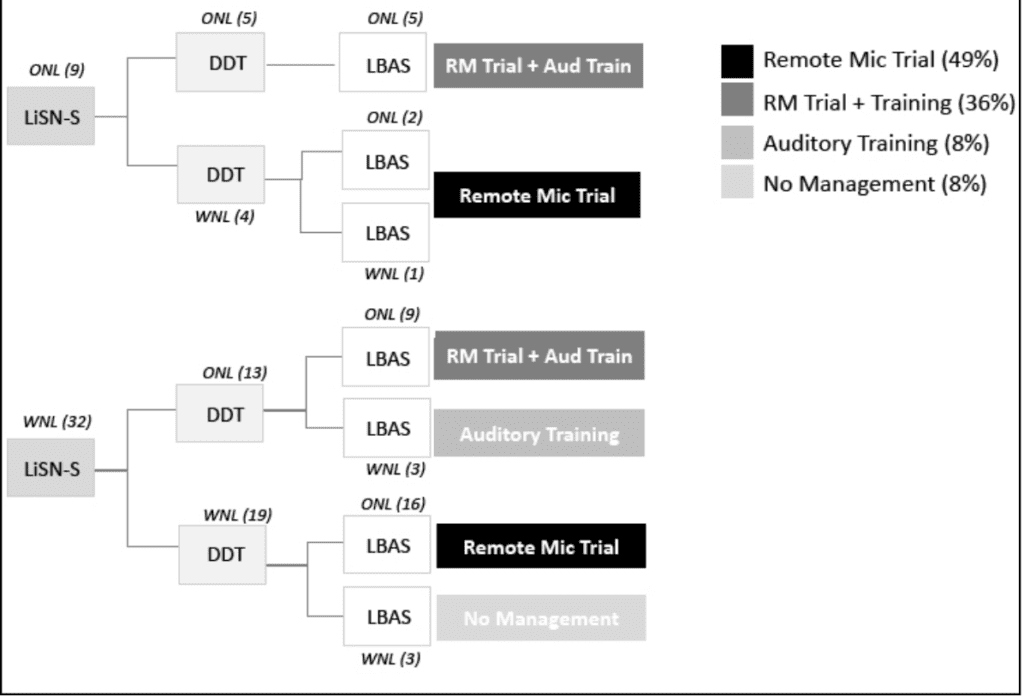
Figure 2. Management matrix displaying four distinct clinical recommendations based on the different deficit patterns observed on measures in the streamlined assessment protocol.
Participant performance was categorized on the three tests included in the streamlined assessment protocol (ie, LBAS, LiSN-S, and DDT) and management recommendations were assigned based on each distinct pattern of results (Figure 2). A total of 39 of the 41 participants completed all tests and four management patterns emerged:
- No recommended management (n = 3, 7.7%),
- Auditory training only (n = 3, 7.7%),
- Remote microphone trial (n = 19, 48.7%), and
- Remote microphone trial + auditory training (n = 14, 35.9%).
No auditory management was recommended for participants with scores within normal age limits on all measures, and auditory training was recommended for participants with performance outside normal age-based limits on the DDT only. Auditory training was recommended in conjunction with a personal RM trial for participants who presented with DDT deficits and either abnormal speech discrimination-in-noise on the LiSN-S, abnormal scores on the LBAS functional listening questionnaire, or both. The performance of all participants could be classified within the management matrix (Figure 2).
Discussion
This study evaluated complex auditory skills in a group of children with ASD and normal hearing sensitivity who presented to the University of Melbourne ASD Listening Clinic with listening concerns. On all clinical tests, the rate of abnormal performance was significantly higher in participants with ASD than expected in a neurotypical population.
A streamlined assessment protocol was introduced comprised of three tests deemed clinically feasible that uniquely informed clinical recommendations. A management matrix was developed offering efficacy-based recommendations for each distinct pattern of clinical results. Future research should re-evaluate recommended assessment and management strategies as new tools and interventions for children with ASD and listening difficulties emerge.
The proportion of participants with ASD who presented with abnormal performance on the LBAS, DDT, and LiSN-S tests was at least 8 times higher (LBAS = 32.8x higher; DDT = 17.6x higher; LiSN-S = 8.8x higher) than expected based on data in neurotypical, age-matched peers. Although auditory filtering deficits have been reported by parents of as many as 51-79% of children with ASD,1 the rate of observed auditory deficits in study participants may be elevated compared to the general population of children with ASD. This is likely due at least in part to sample bias since participants in the study self-referred for hearing evaluation due to reported listening difficulties. On the streamlined assessment, all but 8% of children exhibited abnormal performance on at least one measure. Of those clinically identified with auditory deficits, 85% presented with reduced performance on a behavioral speech-in-noise test (22%) and/or a questionnaire evaluating real-world complex listening skills (82%), and 44% exhibited abnormal dichotic listening scores.
The tests in the abridged battery comprise measures of speech recognition in noise, functional listening, and dichotic listening; all have prior evidence of management-associated improvements on these tests or similar tests in children with ASD. Auditory training has been shown to improve binaural listening performance in individuals with ASD,7,10-11 but it is noteworthy that benefits depend on program adherence which typically requires multiple training sessions per week for an average period of 2 months or more.
Remote microphone technology has been shown to produce immediate benefits to speech recognition in noise and improved auditory behavior with device use over an extended trial.3,7-9 Efficacy data is available for both soundfield and personal RM systems,3,4,7-9,12 but candidacy for one versus the other depends on individual patient presentation. Ear-level personal devices are more appropriate for higher-functioning patients with low tactile defensiveness, such as those who tolerate earphone placement during conventional audiometric testing. Personal RM technology has the advantage of being used in both home and school settings while soundfield systems are generally reserved for classrooms. Nonetheless, both put children in a better position to access speech to support learning and engagement.
Although auditory issues have been consistently identified among the most common parent-reported sensory issues affecting children with ASD,1 hearing care professionals rarely evaluate complex listening ability during clinical appointments. The disconnect between patients’ complaints and the conventional test battery may stem from limited knowledge of the listening challenges common to patients with ASD or the management options available to promote listening in these patients. The current work characterized complex listening skills in a group of children with ASD and normal hearing sensitivity and introduced a remediation-driven streamlined assessment and management matrix to quantify functional listening difficulties and associated clinical recommendations. By more comprehensively assessing auditory functioning in patients with ASD, hearing healthcare providers are better able to support patients with ASD struggling with functional listening difficulties.
References
- Tomchek SD, Dunn W. Sensory processing in children with and without autism: A comparative study using the short sensory profile. Am J Occup Ther. 2007;61(2):190-200.
- Beers AN, McBoyle M, Kakande E, Santos RCD, Kozak FK. Autism and peripheral hearing loss: A systematic review. Int J Ped Otorhinolaryngol. 2014;78(1):96-101.
- Rance G, Saunders K, Carew P, Johansson M, Tan J. The use of listening devices to ameliorate auditory deficit in children with autism. J Pediatrics. 2014;164(2):352-357.
- Feldman JI, Thompson E, Davis H, et al. Remote microphone systems can improve listening-in-noise accuracy and listening effort for youth with autism. Ear Hear. In press.
- Alcántara JI, Cope TE, Cope W, Weisblatt EJ. Auditory temporal-envelope processing in high-functioning children with autism spectrum disorder. Neuropsychologia. 2012;50(7), 1235-1251.
- Alcántara JI, Weisblatt EJL, Moore BCJ, Bolton PF. Speech-in-noise perception in high-functioning individuals with autism or Asperger’s syndrome. J Child Psychol Psychiatry. 2004;45(6):1107-1114.
- Schafer EC, Gopal KV, Mathews L, et al. Effects of auditory training and remote microphone technology on the behavioral performance of children and young adults who have autism spectrum disorder. J Am Acad Audiol. 2019;30(5):431-443.
- Rance G, Chisari D, Saunders K, Rault J-L. Reducing listening-related stress in school-aged children with autism spectrum disorder. J Autism Developmental Disorders. 2017;47:2010-2022.
- Schafer EC, Wright S, Anderson C, et al. Assistive technology evaluations: Remote-microphone technology for children with autism spectrum disorder. J Commun Disorders. 2016;64:1-17.
- Denman I, Banajee M, Hurley A. Dichotic listening training in children with autism spectrum disorder: A single subject design. Int J Audiol. 2015;54(12):991-996.
- Kozou H, Azouz HG, Abdou RM, Shaltout A. Evaluation and remediation of central auditory processing disorders in children with autism spectrum disorders. Int J Pediatric Otorhinolaryngol. 2018;104:36-42.
- Keller MA, Tharpe AM, Bodfish J. Remote microphone system use in preschool children with autism spectrum disorder and language disorder in the classroom: A pilot efficacy study. American Journal of Speech Language Pathology (AJSLP). 2021;30(1):266-278.
- Hillock-Dunn A, Taylor C, Buss E, Leibold LJ. Assessing speech perception in children with hearing loss: What conventional clinical tools may miss. Ear Hear. 2015;36(2):e57-e60.
- James P, Schafer E, Wolfe J, et al. Increased rate of listening difficulties in children with autism spectrum disorder. Submitted.
- Cameron S, Dillon H. Development of the Listening in Spatialized Noise-Sentences test (LISN-S). Ear Hear. 2007;28(2):196-211.
- Musiek FE. Assessment of central auditory dysfunction: The Dichotic Digit Test revisited. Ear Hear. 1983;4(2):79-83.
- BrainTrain website. IVA-QS Integrated Visual and Auditory Continuous Performance Test Quick Screen Version [computer software]. https://www.braintrain.com/iva-qs/.
- Dunn W. Sensory Profile 2. 1st ed. Pearson;2014.
- Keller MA, Tharpe AM, Bodfish JW. Listening Behavior in Autism Scale (LBAS). In: MA Keller, ed. Listening Difficulty in Children with Autism Spectrum Disorder: Evaluation and Intervention [doctoral dissertation]. Vanderbilt University;June 2021.

FOR MORE DETAILS on managing listening difficulties in children with ASD, visit: www.PhonakPro-US.com/ASD.
CORRESPONDENCE can be addressed to Dr Dunn at: [email protected].
Citation for this article: Dunn A, James P, Pelosi A, Sorensen E, Oleson J. Managing listening difficulties in patients with ASD and normal hearing sensitivity. Hearing Review. 2021;28(10):12-16.






I for one was not surprised at the correlation between auditory dysfunction, in spite of normal hearing, and global sensory processing deficits. And I am sure many other readers who are familiar with this population are nodding their heads in agreement.
What I would like to point out is the opportunity missed when we simplistically say, “That’s interesting.” or “That’s common.”
I would like to suggest that the ears can be our key in to unlocking the solution to many of the issues faced by a child with ASD. But to do so we need to be willing to step away from the “hearing aids are the tool we use to try and address everything auditory” be it hearing loss, hyperacusis, or APD, and be open to how much more there is we can offer.
The gut-brain connection in this population has been well demonstrated and yet is ignored, approached in a hit-or-miss fashion via elimination diets, or assessed privately through expensive lab work. Which I find odd, since there must be signs of this immune issue that professionals should be able to pick-up on. I would suggest that identification of otitis media may be the key we can bring to the table.
Have you ever wondered why we as professionals need the oversight of an MD to approve providing amplification?
And yet an SLP does not require auditory clearance before providing treatment?
Imagine, if every child with a communication issue had an auditory assessment, in spite of having passed a NBHS. With an equal concern in identifying hearing loss and to catching otitis media. How much more effective would speech therapy be?
Now imagine even bigger. What if we recognized otitis media as a sign of the immune issue it largely is? Instead of simply giving antibiotics or even tubes for relief of symptom, we referred parents to also get to the bottom of why their child keeps having middle ear fluid. what gut-brain factors are causing this medical problem that is resulting in developmental issues due in part to auditory and vestibular deprivation?
To do this we need to understand…
1) How to catch otitis media instead of missing the incidences, just because the child isn’t crying in pain or didn’t just happen to be by the pediatrician.
2) The significance of doing more than just relieving the symptoms. For even if the tubes remain in place and patent we are missing the larger red flag and the window of developmental opportunity that may be lost. We know for sudden onset hearing loss you want to get to the ENT ASAP to benefit from the possibility of steroids reversing the hearing loss. We know we want to provide implants to congenitally deaf children within the 1st year to minimize the gap in speech and language development that is blatant on someone who is only implanted after age 3. We need to likewise understand that otitis media needs to be better identified, that relying on a child to cry in pain is woefully inadequate. Communication struggles is our red flag to do auditory testing and should be done before speech services are tried. Similarly, I would suggest that vestibular issues should be a red flag as well. This means if an infant is not crawling, a toddler not walking or clearly shows signs of vestibular insecurity the OT’s and PT’s should know, not only to have the vision assessed, but the auditory/vestibular system as well. A good sign that otitis media is at play is a child who is prone to colds, coughs or seasonal allergies. It is something any of these other allied healthcare professionals can ascertain to support the recommendation of an auditory evaluation. I encourage parents to schedule specifically when the child has a cold or seasonal allergies.
We have a lot of value to bring to the table, let’s do so.
Chanie Monoker, CCC-A
Developmental Audiologist
I’m not only nodding my head in agreement, this has been a big aha moment for me. Should I have know about this earlier? After seeing a panel of specialists a couple years ago to get my then 4 year old son diagnosed with Autism no one seemed to be talking about underlying causes. It seemed to make them uncomfortable mostly. I would get the same answers ‘We think Autism is caused by 2 factors, 1. Genetic 2. Environmental( toxins/heavy metals maybe). We were then given really only 2 options for treatment. Speech Therapy and Occupational therapy. Nothing targeting root cause or gut/brain disruptions. It seems to me both Therapy and targeting root issues would be more effective. After reading this article it gives me hope that using a hearing device with a remote microphone or a soundfield system could make his therapy, school and at home learning sessions much more beneficial while helping create those much needed neuro pathways during his early development. At this point I’m highly interested in finding out more and hopefully implementing something with him asap. Is it possible to find a local Audiologist that works with kids with Autism that can conduct the tests in the article? Id assume this is in early stages of research however I can’t imagine much risk trying a remote mic or other system. A hearing device may be a bit tricky for him to keep on but worth working at. I’m also looking into finding DAN/Functional Medicine Doctor that we can work with and discuss safe detox protocol’s or other alternatives that may address the gut issues.
Tim Newcomb – Hearing Instrument Specialist
Hi Tim,
Thank you so much for your comment. Although there is a growing number of professionals in schools and clinics who recommend trialing remote microphone technology for children with ASD and listening difficulties, this area is still relatively new. Hopefully, as the efficacy data continues to grow, comprehensive assessment and treatment will become more common. Reflecting back on the earlier comments, I agree that intervention may not only help reduce listening difficulties, but also put children in a better position to be able to learn and engage whether it be in school, during therapy, or when interacting with family at home.
Andrea Dunn, AuD, PhD