Improving quality at the point of sale to establish a patient-driven practice
Differentiating your practice not only bolsters your market position and value to your patients, but also safeguards you against the steady rise in Internet sales, over-the-counter PSAPs, and low-margin distribution systems. Here is a Top-10 list of ways your hearing care practice can remain the provider-of-choice for your patients, as well as specific tests, tools, and procedures you can use to bring to life each item on the list within a busy dispensing business.
There has never been a more critical time for all hearing care professionals—audiologists, hearing instrument specialists, manufacturer’s representatives, and business executives—to embrace the need to raise quality standards. Competition from direct-to-consumer hearing aid distribution models and quasi over-the-counter instant-fit devices are among the threats practitioners must face over the next decade. These industry changes are likely to force hearing care professionals to differentiate their products and services or risk the marginalization of the traditional patient-provider business model.
The ability to differentiate with quality is especially critical for service providers who have worked for several decades within a relatively stable distribution system, and have recently felt the rising tide of less expensive alternative systems, including the Internet and the over-the-counter sales of personal sound amplification products (PSAPs). Fortunately, the path to differentiation rests in the hearing care professional’s ability to customize delivery of products and services to patients. Three recent studies underscore this trend.
In July 2009, Consumer Reports published a review of various industry practices.1 One of the key conclusions was that two-thirds of patients were not properly fitted with hearing aids. Regardless of the methodology of this review, this finding alone should raise concerns within the various professions responsible for delivering hearing health care. Another recent article2 published in the April 2010 edition of Hearing Review drew similar conclusions, suggesting that and a “common sense” hearing aid fitting approach would include:
- Physical evaluation/examination of the ear and a review of the patent’s history;
- Acquisition of reliable and valid measures of the patient’s hearing loss;
- Selection of the correct technology for the patient;
- Assessment of expectations and establishment of realistic expectations;
- Performing quality-control measurements on the hearing aids prior to fitting via a hearing aid analyzer;
- Determining the required valid gain and output prescription and verifying the fitting via real ear measurement (REM) with probe microphones;
- Fine-tuning the hearing aid fitting with available software based on patient input, as well as the use of patient-specific behavioral measures such as loudness discomfort levels (LDLs/UCLs), acceptable noise levels (ANLs), and signal-to-noise ratio (SNR) loss;
- Validating that the patient’s treatment with hearing aids has been effective by comparing pre- and post-measures of speech or sentence comprehension in noise and quiet and using real-world performance metrics;
- Providing counseling and aural rehabilitative services relative to the patient’s specific needs.
Kochkin et al2 examined the relationship between satisfaction with hearing aids and the use of a pre-fitting clinical protocol. The authors evaluated various components of a pre-fitting protocol and concluded that the majority of clinicians failed to implement many of the common sense “best practice” approaches listed above.
In addition, their data strongly suggested that the implementation of comprehensive protocols has a major impact on: hearing aid brand loyalty, utility of hearing aids, positive-word-of-mouth advertising, satisfaction with benefit achieved, hearing handicap reduction, hearing aid usage, and reduction of hearing aids in the drawer. Lastly, this research indicated that those not utilizing many of these best practices are vulnerable to disruptive technologies, such as direct mail, Internet distribution, and over-the-counter devices (Figure 1).

Finally, Rogin3 publicized the results from a focus group of dozens of highly satisfied hearing aid users. The Top-10 Reasons for Hearing Aid Delight shown in Table 1 suggest there are at least 10 ways to improve the overall patient satisfaction levels. Although this unpublished report offered several suggestions to leverage the findings of the focus group, the author did not suggest any specific tools or tactics that could be used clinically.
This article provides several clinical tools, audiometric tests, and service tactics—many of them based on reasonable scientific evidence—designed to leverage the findings of these three important studies.
#10 Hearing Aids Actually Work
Recently, there has been renewed interest in sound quality as a key determinant of patient benefit and satisfaction. Test chamber and real-ear analyses are useful for detecting anomalies that may be related to poor sound quality, such as irregular frequency response, limited bandwidth, or distorted output, but objective tests alone cannot fully define hearing aid fidelity.4 Before a patient receives hearing aids from the professional, a live listening check and objective analysis of the devices are essential.
At the core of Reason #10, however, is ensuring that as many listening situations as possible encountered by patients on a daily basis are targeted and improved with amplification. Research has shown that, when 80% or more of a patient’s targeted listening situations are improved with amplification, there is a good chance the patient will have high overall satisfaction and become a promoter of your practice (Figure 2).
Multiple environment listening utility (MELU) describes the number of discrete listening situations encountered by patients that are successfully remediated with amplification.5 Most patients are likely to encounter more than a dozen uniquely different listening situations throughout a typical week. One tool used to evaluate these discrete listening situations is the TELEGRAM (Figure 3), a tool created by Linda Thibodeau, PhD, of the Callier Center at the University of Texas-Dallas.6
TELEGRAM is an acronym signifying common listening situations encountered by most patients. During the pre-fitting appointment, the dispensing professional is able to rate the patient’s ability to communicate in a variety of common listening situations on a 1 to 5 scale. In addition to serving as a pre-fitting assessment of unaided communication ability, the TELEGRAM readily enables professionals to evaluate many challenging listening environments, such as cell phones, movie theaters, and large groups. It serves as an avenue to open dialogue with the patient about assistive listening devices (ALDs), loop systems, and alerting devices, all of which may improve the MELU of the patient when prescribed by the professional.
#9 Motivation
Reason #9 is motivation of the patient to seek your services. Over the next 20 years, 10,000 people per day are expected to turn 65. These so-called Baby Boomers are known to be more proactive about their health care than their parents. At the local level, this means that you need to utilize marketing tactics that continually educate and attract these prospects to your practice.
Due to the wonders of the World Wide Web and social media, there are now a variety of ways a patient can come into contact with your practice. Recent data has shown that about 80% of people over age 65 are connected to the Internet. This suggests that your website must be engaging enough to educate and attract these prospects to your office.
In addition to a great website, you must find other ways to keep these non-buyers engaged in your practice. Some of the tactics used to keep the consequences of untreated hearing loss top-of-mind with this segment include reaching out to other medical professionals using the Quick Hearing Check7 and other downloadable hearing “apps” as a means of attracting people to your practice.
#8 Professionalism
When a prospect decides to make an appointment with your practice for services, it’s a given that he or she and the significant other will be treated with dignity and respect. This concept is referred to as etiquette-based medicine.9 Etiquette-based medicine is an interaction in which professionalism and patient satisfaction are put at the center of the clinical encounter.
One way to incorporate etiquette-based medicine into your practice is through process mapping. Process mapping refers to segmenting the patient’s interaction with your office into discrete stages (Figure 4). For example, for each stage shown in Figure 4, your practice would map out what behaviors and time commitments are required of you and your employees to maximize patient satisfaction at each stage.
FIGURE 4. The workflow of a typical hearing aid dispensing practice, along with suggested time allotment benchmarks.
#7 Evaluation
One of the biggest opportunities in many practices is improving the closure rate, which is best defined as the number of true opportunities to purchase divided by the number of prospects actually agreeing to purchase hearing aids from you. Improving your closure rate by 10% to 20% can result in upwards of $100,000 increase of annual revenue.
One way to improve closure rates is through the use of computerized testing. The data used to create this HIA top-10 list shows patients are more likely to be extremely satisfied when tests have the perception of being high tech.
We can think of no better example of high-tech pre-fitting measures than speech-in-noise tests. What’s remarkable about these pre-fitting tests is there is good clinical evidence supporting their effectiveness. Two tests that have research supporting their use in the hearing aid fitting process are the QuickSIN and the Acceptable Noise Level (ANL) tests.
#6 Counseling
Delighted users receive counseling both verbally and in print. In addition to providing personal adjustment counseling, it is essential to provide the patient with information on the care and use of hearing aids, proper orientation to initial use, and expectations.
Research has shown that patients forget most of the information we shared with them shortly after their appointment. In order to help patients retain this information, printed material needs to be given to the patient to take home following the initial visit.
#5 A Strong Recommendation
Your ability to be persuasive is essential to making a strong recommendation at the conclusion of a pre-fitting appointment. When we talk about persuasion, we are not referring to high pressure sales tactics. Rather, persuasiveness is a combination of being a great relationship builder and your ability to effectively communicate technical information to patients.
Persuasiveness is a natural consequence of conducting yourself in a professional manner. Once you have established your professionalism, your ability to make a strong recommendation is relatively straightforward. Making a strong recommendation for the technology you think is appropriate for the patient is a by-product of confidence and credibility.
#4 Experimentation
Hearing aids are considered to be a high ticket item. Given this fact, consumer psychology tells us that the patient needs to take the time to touch, feel, and use amplification prior to agreeing to purchase it. Incorporating a hearing aid demonstration into the evaluation has the potential to improve return-for-credit rates by 50%, according to the HIA study used to formulate this top-10 list.
When conducting a live hearing aid demonstration during the pre-fitting appointment, you can save time by pre-programming a pair of BTE devices. Place the hearing aids into the ears and conduct a “distance demo.” With your face covered to prevent lip reading, have the patient repeat short sentences as you increase the distance from the patient. When the patient fails to repeat half of the sentence, record your distance. Repeat the same procedure in the unaided condition. The aided condition should yield a distance of about twice as far as the unaided condition.
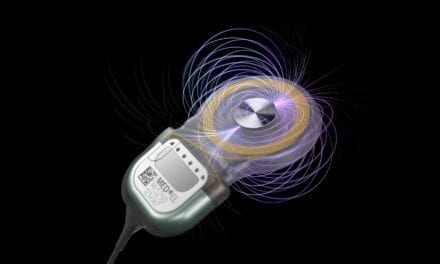
#3 Verification & Validation
Probe microphone measures have been the recognized gold standard for hearing aid verification for more than 20 years. Recent advances in wireless functionality, digital sound files, and pre-set computer programs have made the use of probe microphone measures less cumbersome.
If your goal is to restore audibility and comfort for soft, average, and loud sounds, matching one of the independent prescriptive targets (eg, NAL-NL2 or DSLv5.0a) would be your starting point. Using live speech, probe microphone measures can also be used to demonstrate to patients the effect of amplification on familiar voices or common environmental sounds.
A separate clinical procedure is validating patient benefit through the routine use of objective and subjective outcome measures. Table 2 outlines a recommendation protocol for using a combination of objective and subjective (self-reports) to measure outcome. As a rule of thumb, patients should receive a two to three category improvement on any self-report on a 1 to 5 scale. This amount of improvement would reflect 40% to 60% benefit from amplification and is an indication that your treatment has been effective.
#2 Continued Connection
Research has indicated that more than 50% of all hearing aid users repurchase from another practice or distributor upon their next purchase. This finding would suggest professionals have an opportunity to improve retention of their existing patient base.
The best way to accomplish this is through a comprehensive patient retention program, which includes patient newsletters and routine follow-up appointments. In our experience, we have found that a practice needs between 20 and 25 patient contacts over a 4- to 5-year period between hearing aid purchases. Using a combination of semi-annual patient check-up appointments and newsletters is a proven strategy to retain patients.
#1 You, the Hearing Care Professional
The ability of the hearing care professional to deliver personalized care using protocols supported by good clinical evidence has been shown to improve satisfaction and loyalty. Professionals with both the skill and will to differentiate their practice on quality will continue to enjoy a significant competitive advantage as well as the ability to command a premium price for their products and services. The traits and behaviors believed to be highly associated with quality are depicted in the Pyramid of Success in Figure 5.
Organizations and practice owners must have the courage to implement high standards and make certain their staffs execute evidence-based clinical protocols. Individuals within these organizations are obligated to stay abreast of the latest research findings by reading current journals, visiting professional websites, and implementing best practices with patients.12
As the business environment becomes more competitive, practitioners who successfully differentiate their practice along quality lines will command a higher average selling price, enjoy more word-of-mouth referrals, and become recognized as the provider of choice in their marketplace.
References
- Hear well in a noisy world. Consumer Reports. July 2009:32-37. www.consumerreports.org/health/healthy-living/home-medical-supplies/hearing/hearing-aids/a-shopping-summary/hearing-aids-shopping-summary.htm. Accessed April 14, 2011.
- Kochkin S, Beck D, Christensen L, et al. MarkeTrak VIII: The impact of the hearing healthcare professional on hearing aid user success. Hearing Review. 2010;17(4):12-34. Accessed May 27, 2011.
- Rogin C. Top 10 reasons for hearing aid delight. (Recorded course #14615.) Available at: www.audiologyonline.com. Accessed November 29, 2011.
- Brown M. So what’s in the black box? 5 reasons why it matters. Audiology Practices. 2011;3(1):18-23.
- Kochkin S. MarkeTrak VI: On the issue of value: Hearing aid benefit, price, satisfaction and brand repurchase rates. Hearing Review. 2003;10(2):12-25. Accessed May 27, 2011.
- Thibodeau LM. Maximizing Communication via Hearing Assistance Technology. Plotting beyond the audiogram to the TELEGRAM, a new assessment tool. Special Issue: Assistive Listening Devices. Hearing Journal. 2004;57(11):46-51.
- Kochkin S, Bentler R. The validity and reliability of the BHI Quick Hearing Check. Hearing Review. 2010;17(12):12-28.
- Ayres S, Smith N. Location, location, location: SEO and your business. Hearing Review. 2009;16(6):28-30. Accessed May 27, 2011.
- Kahn M. Etiquette-based medicine. N Engl J Med. 2008;358:1988-1989.
- Taylor B, Bernstein, J. The Red Flag matrix using the Quick SIN and Acceptable Noise Level Test. Poster presented at: 22nd annual American Academy of Audiology Conference; April 5-9, 2011; Chicago.
- Urban B. Five ways an online report writer helps dispensing offices. Hearing Review. 2010;17(12):34-36. Accessed May 23, 2011.
- Taylor B. A working-person’s guide to quality and productivity: Part 2: How to increase productivity in your practice. Hearing Review. 2010;17(9):14-24. Accessed May 23, 2011.
Correspondence can be addressed to HR or Brian Taylor, AuD, at .
Citation for this article:
Taylor B., Rogin C. The Top-10 Ways to Create Consumer Delight with Hearing Aids. Hearing Review. 2011;18(7):10-23.