Audiologists at a busy clinic share their experiences implementing the new Audible Contrast Threshold test with 100 patients.
By Erica Bennett, AuD, PhD; Josephine Marino, AuD; Brad A. Stach, PhD; Virginia Ramachandran, AuD, PhD; and Kathleen Faulkner, PhD
Summary
The Audible Contrast Threshold (ACT) test, a quick and language-independent tool for assessing speech-in-noise ability, is designed to provide insights into auditory performance beyond traditional audiometric tests.
Key Takeaways
- Enhanced Diagnostic Utility: The ACT test effectively identifies patients with difficulty hearing in noise, even those with normal audiograms, offering a more nuanced understanding of auditory challenges.
- Ease of Implementation: Clinically feasible, the ACT test integrates seamlessly into routine audiometric evaluations, requiring minimal additional time.
- Future Potential: The ACT test may optimize hearing aid fittings and serve as a diagnostic tool for identifying retrocochlear or central auditory disorders.
New clinical tests or methods may hold great promise, but their implementation in a busy clinical setting can be challenging. These challenges include time constraints, ease of use, interpretation, and applicability to complex and diverse patient populations.
In this article, we share our experiences with the implementation of the new Audible Contrast Threshold (ACT) test—our first 100 patients—in a busy audiology clinic at a large multicenter healthcare system.
The Purpose of Speech Audiometry
The purpose of speech audiometry during routine audiometric testing is multifaceted when it comes to testing functional abilities of individuals with hearing loss. Most commonly, speech testing—specifically word recognition in quiet (WRQ)—is thought of as an assessment of suprathreshold speech understanding, which offers insights into communicative function and practical connections to rehabilitative measures. However, as many hearing professionals recognize, a patient’s hearing loss can be far more complex than what is reflected in the audiogram and on WRQ tests. Speech testing can also be important for its diagnostic value. For example, if a word recognition score is poorer than expected from the patient’s profile and audiogram, it can be indicative of retrocochlear or central auditory disorder.
To better serve as a diagnostic indicator, Henry Ford Health System completes all WRQ at a high intensity level to screen for “rollover.” “Rollover” refers to a phenomenon of decreasing word recognition scores with increasing speech presentation levels (Jerger & Jerger, 1971), a sign of retrocochlear disorder.
WRQ is largely the default measure of speech perception during routine audiologic assessment. However, in more recent years, there is a growing body of research suggesting that measures of speech-in-noise should be a routine component of the standard audiologic assessment. A majority of patients with hearing loss report challenges in understanding speech in the presence of background noise (Le Prell & Clavier, 2017). The audiogram, including WRQ, is shown to be a marginal predictor of how well patients perform in more real-world environments, including in noise (Vermiglio et al., 2012; Wilson, 2011). Recent studies have suggested that monosyllabic word recognition in quiet should be supplemented with or replaced by speech-in-noise measures, as these provide a more accurate prediction of a patient’s real-world abilities in noisy environments (Fitzgerald et al., 2023) and may be a more effective diagnostic tool for identifying retrocochlear and central pathologies (Qian et al., 2023).
The Challenge of Speech-in-Noise Testing
Speech in noise (SIN) testing has been suggested as a routine part of clinical practice dating back to the 1970s (Carhart & Tillman, 1970). However, outside of cochlear implant care, this practice has not been adopted into standard hearing evaluations. This lack of testing occurs despite numerous clinical tools available for clinician use, including the Hearing in Noise Test (HINT)(Nilsson et al., 1994), the QuickSIN (Killion et al., 2004), and the Bamford-Kowal-Bench (BKB) SIN (Wilson et al., 2007). This raises the question: why, despite the many available options and supporting literature, has it not become a routine part of clinical care?
There are probably several contributing factors to the lack of adoption. The first is that monosyllabic word recognition in quiet is a historic and traditional part of the routine audiologic evaluation and is expected to be included by both audiologists and otolaryngologists as a part of the hearing evaluation report. ,
Secondly, as demands for patient care increase, the time available for clinicians to perform clinical audiometric testing decreases. As increasing time constraints influence the clinician’s schedule, many are not able to add additional SIN testing to their routine clinical practice.
Also, as patient populations have become increasingly diverse, the patient’s native language may also be a barrier to performing SIN testing as it likely requires higher linguistic demand than simply repeating back monosyllabic words in quiet.
Finally, even if SIN testing is performed, it can be challenging to interpret and apply the additional information provided by the SIN tests. It may be unclear to clinicians how to incorporate data from SIN testing into recommendations for amplification, candidacy for cochlear implants, and predictive satisfaction with hearing aids.
For these reasons, further research on the application of SIN tests in a clinical environment is needed, particularly if there is a move to replace WRQ with SIN (Fitzgerald et al., 2023).
The Audible Contrast Threshold (ACT) Test
The ACT test was designed for the purpose of being a quick, objective, language-independent diagnostic test to predict aided speech-in-noise ability.
The test stimuli are spectro-temporally modulated (STM) signals, which means that they have acoustic changes that occur over time in a manner that is like speech. Early research conducted at Walter Reed Medical Center showed STM stimuli to be highly correlated with a patient’s speech-in-noise abilities (Bernstein et al., 2013; Mehraei et al., 2014). The STM stimuli of the ACT test are presented in a train of episodes of regularly occurring pink noise (without STM). By inserting speech-like STM target stimuli with varying degree of modulation into the train of non-STM reference sounds, the ACT test serves as a language-independent proxy for traditional speech-in-noise testing. Its language-independent nature makes it potentially more broadly applicable to a diverse clinical population. Large-scale international clinical studies with the ACT test confirmed its significant relationship with speech-in-noise performance in ecologically valid settings in different clinical populations and its predictive power of speech-in-noise ability compared to the audiogram alone (Santurette& Laugesen, 2023.; Zaar et al., 2023, 2024; Zaar, Ihly, et al., n.d.; Zaar, Simonsen, et al., 2024.).
The outcome that the ACT test is designed to predict is aided performance on the HINT under ecologically valid conditions (Zaar et al., 2024). To predict aided performance, the ACT stimulus must account for the hearing sensitivity loss of the listener. Thus, the ACT test can only be performed following pure-tone audiometry, as it uses the patient thresholds to automatically create frequency-dependent stimuli. The “audible” in Audible Contrast Threshold refers to this aspect of the stimulus.
To facilitate ease of use and brevity in testing, the stimulus presentation re-uses the psychometric strategy of the Hughson-Westlake method for obtaining an audiometric threshold—in this case using a down 4, up 2 dB step size. The degree of modulation in the ACT target signal is adjusted until a threshold level of performance is reached. The individual just-noticeable degree of STM is normalized to a reference of data acquired from young adults with normal hearing and is known as the “audible contrast threshold.” So, the value obtained is relative to a 0 dB normalized contrast level, or nCL (Zaar/Simonsen et al, 2023).
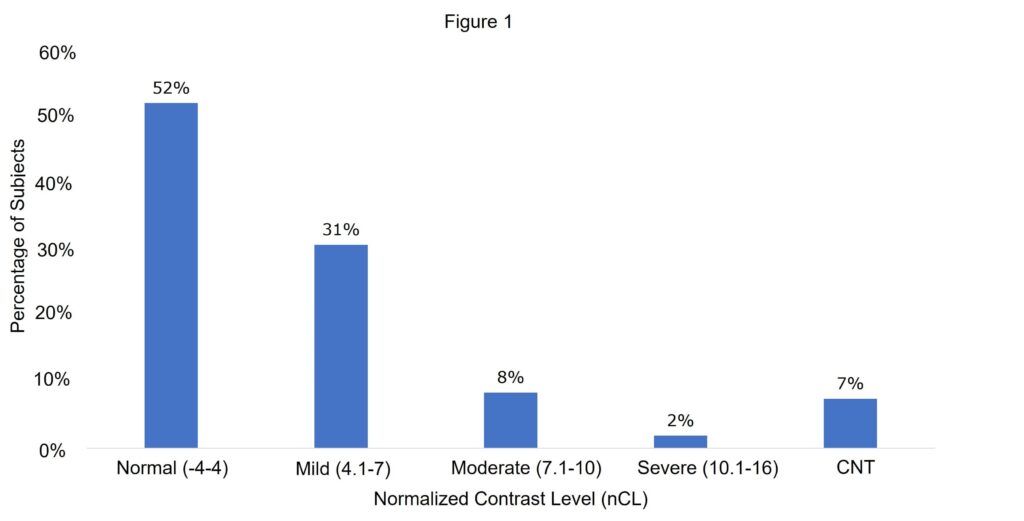
The ACT value obtained during testing can range from -4 to 16 dB nCL, with ranges -4 to 4 dB nCL being normal, 4.1-7 dB nCL being a mild contrast loss, 7.1-10 dB nCL being a moderate contrast loss, and 10.1-16 dB nCL being a severe contrast loss. Higher levels of contrast loss predict greater degrees of difficulty in aided speech testing.
The test is conducted using pre-existing diagnostic audiometric systems via a software upload, including models of the Interacoustics Affinity Compact; the Grason-Stadler AudioStar Pro Version 2; and the MedRx AVANT ARC, AVANT A2D+, AWRC, and AVANT (Stealth) systems.
Based on the aforementioned characteristics, the ACT test has potential clinical benefit that we wished to investigate. For example, the ACT value may be able to help set realistic expectations for hearing aids or aid in the provider’s counseling of patients with poor ACT values. The ACT value may also be implemented directly into manufacturer fitting software to optimize noise-reduction algorithms to match the patient’s abilities in background noise (Santurette and Laugesen, 2023). It is currently unknown whether there is potential diagnostic utility in identifying specific suprathreshold auditory disorders.
Clinical Implementation at Henry Ford Health
The ACT test was implemented on four compatible GSI AudioStar audiometers at three clinical sites (out of 14 audiometers among the 8 clinics). It was completed in real-world clinical conditions on the first 100 patients seen in the clinic following installation and audiologist training. Routine audiometric testing, including immittance measurements, pure-tone threshold testing, and speech audiometry (including speech reception threshold and word recognition in quiet using the NU-6 list) were completed on each patient. The ACT test was completed at the end of the routine test battery. We estimate that this additional testing added one to three minutes of patient encounter time.
Testing of the first 100 patients was completed over a one-month period from 3/18/2024-4/17/2024. Patients ranged in age from 22-96 with a median age of 61 years old. 67% of patients were female, and 36% of patients were male. To reach our goal of 100 patients tested on the ACT test, 108 patients were required in total as eight patients were not able to be tested. Of the eight patients who could not be tested, two had a documented cognitive impairment, two had debilitating tinnitus that they reported prevented them from distinguishing the stimuli from the noise, one had a language barrier and was unable to understand instructions, one had a significantly asymmetric hearing loss with one ear falling in the severe to profound range, and two were not able to be conditioned to the task without an identifiable reason. It should be noted all eight of the patients were able to complete a traditional hearing evaluation.

Figures 1-5 represent results from the first 100 patients at Henry Ford Health that were able to be tested on the ACT test. Percentage of patients by normalized Contrast Level is shown in Figure 1. Over 80% of patients fell into either the normal or mild contrast loss range. Following the overall trend, we investigated what factors may be playing a role in this distribution. The relationship of pure tone average (PTA) with patients’ nCL is shown in Figure 2. Figure 2 displays only patients with symmetric hearing (less than 10 dB between PTAs) (n=82), and the PTA depicted is the average between the patient’s ears. A Pearson correlation coefficient was computed to assess the linear relationship between PTA for patients with symmetric hearing and nCL (82 of 100 patients). There was a significant positive correlation between the two variables, r(80)=[0.63], p<0.01, suggesting that higher PTAs are generally associated with poorer values on the ACT test.
Average nCL (± standard error) as a function of patient age is shown in Figure 3. In general, older patients had higher nCL values, suggesting poorer predicted performance in noise with age. This is consistent with previous research on aging and performance in background noise (Tremblay et al., 2021). On average, starting at age 60, patients began to fall into the mild to moderate contrast loss categories. In this study, PTA was highly correlated with performance on the ACT test. While older adults likely had greater amounts of hearing loss as well as higher PTAs, other studies have reported that older adults show poorer performance on speech in noise than younger adults, even after controlling for degree of hearing loss (Bilodeau-Mercure et al., 2015; Fostick et al., 2013). This suggests that the ACT test may be a useful tool to identify impairment beyond the audiogram in this population, allowing for improved counseling and hearing technology recommendations.

The ACT values for patients with normal hearing, defined as thresholds 20 dB or better across all frequencies, are shown in Figure 4. The normal hearing patients were divided into two groups along the x-axis, patients who presented with a chief complaint of hearing loss and patients who presented with a chief complaint other than hearing loss (e.g., dizziness). Of the patients who did not have a chief complaint of hearing loss, 100% had a normal ACT value. In this study the ACT test demonstrated 100% specificity for normal hearing patients with no hearing related complaints. Alternatively, of the patients who presented with hearing loss concerns, 16% had an elevated nCL value. This suggests that the ACT test could be an objective measurement to assist in counseling patients who struggle to hear, despite the audiogram suggesting normal audibility.
The relationship of WRQ scores (x-axis) to nCL value (y-axis) is shown in Figure 5. A Pearson correlation coefficient was computed to assess the linear relationship between WRQ for patients with symmetric hearing and nCL value (82 of 100 patients). There was a small but significant negative correlation between the two variables, r(80)=[-0.26], p=0.02. This means that lower ACT values (better contrast ability) were related with better word recognition. The ACT values across all patients with 100% WRQ are shown in Figure 6. Of patients with 100% WRQ, 35% demonstrated a mild or moderate contrast loss. These results suggest that the ACT test is an objective way to identify patients who may need additional support in noise beyond what WRQ may be able to predict.
Discussion
Despite its potential for contributing to a better understanding of auditory communication function, traditional SIN testing methods present barriers to routine clinical implementation. The new ACT test may be a solution by providing a rapid metric with which to evaluate a patient’s performance outside of the standard audiometric testing battery that is efficient and independent of the patient’s native language. The ACT test proved to be feasible and easy to use for the audiologist, allowing for easy integration into everyday clinical practice. As described, of the patients tested, only 7% were unable to complete the test.

Correlation
An important aspect of our results with the ACT test is that for patients with hearing loss, the ACT value was highly correlated with their PTA but not correlated with their WRQ scores. For example, for patients with 100% WRQ, we saw greater variation in ACT values, suggesting that WRQ alone is not predictive of patients who may struggle in background noise, possibly due in part to its ceiling effect, but likely also due to the absence of competing noise. This is consistent with what is well known clinically, as two patients with the same audiogram may report very different communication abilities. These results are also consistent with previous literature that suggests that unaided WRQ through insert earphones is not predictive of hearing aid benefit or aided WRQ (McRackan et al., 2016). Even with WRQ of 100%, 30% of patients displayed abnormal ACT values, consistent with previous literature that showed deficits in SIN observed in individuals with little to no difficulty understanding speech in quiet (Fitzgerald et al., 2023; Middelweerd et al., 1990; Saunders & Haggard, 1989; Vermiglio et al., 2018). The variance of ACT values among patients with excellent WRQ suggests that the ACT value may be a quick and efficient SIN measurement to aid in making recommendations for hearing technology beyond what the audiogram might suggest.

Variance
A second notable aspect of our results with the ACT test is the variance in scores among patients with normal hearing based on their audiometric thresholds. Among patients with normal hearing and chief complaint of hearing loss, 17% demonstrated increased nCL values on the ACT test, suggesting that the test may be reasonably sensitive to patients’ performance in background noise. The patients with normal hearing and an elevated ACT value ranged in age from 23-34 years of age. They all had normal middle ear function (defined by type A tympanograms with present ipsilateral and contralateral acoustic reflexes), no known cognitive impairment, a normal otoscopic exam, and no reported history of noise exposure. The population of patients with normal hearing and poorer than expected SIN abilities is consistent with previous literature suggesting that SIN challenges may be present in some patients with normal hearing thresholds (Fitzgerald et al., 2023; Middelweerd et al., 1990; Saunders & Haggard, 1989; Vermiglio et al., 2018).
On the other hand, 100% of patients with normal hearing and no complaints of hearing loss demonstrated normal ACT values, suggesting that specificity of the ACT test is excellent. These data suggest that the ACT test may capture auditory deficits in a way that the traditional audiometric test battery cannot.
Future Research
One aspect of the ACT test that was not investigated in this study is its clinical applicability to fitting hearing aids. Oticon has developed an ACT-based prescription for speech in noise settings. Oticon’s Genie 2 fitting software creates a prescription based on the three most significant predictors of speech in noise ability including the ACT value, the audiogram, and age (Santurette & Laugesen, 2023). While the current study looked at the clinical feasibility of performing the ACT test, it did not assess how it may personalize the advanced hearing aid features for our patients to promote greater success in background noise. Future research will focus on how the ACT test can be used to individualize hearing aid selections and fittings.
Finally, the ACT test may be beneficial as a diagnostic tool; however, the current study was not extensive enough to provide any evidence. Recent research suggests that SIN measures may be more accurate than WRQ as an audiologic screening for acoustic tumors (Qian et al., 2023). Should the ACT test be beneficial as a diagnostic tool, it would add additional strength in the detection of retrocochlear and central auditory disorders. In addition, if beneficial as a diagnostic tool, audiologists could transition to routine ACT assessment as part of a standard audiometric test battery without hindering assessment of various other audiologic disorders. Future research will focus on the ACT test as a potential diagnostic tool.

Summary
In summary, the ACT test was easy to implement, and we were clinically successful in obtaining outcomes on the vast majority of patients. The test was fairly sensitive to complaints of difficulty hearing, even in those with a normal audiogram. In addition, the test demonstrated 100% specificity at detecting normal patients (normal hearing and no complaint of hearing loss).
Future research on the ACT test may help to drive more individualized recommendations on hearing technology as well as have potential as a diagnostic tool for differentiating cochlear disorders from retrocochlear disorders.
About the Authors:
Kathleen Faulkner, PhD, is a Senior Researcher at the headquarters of Oticon in Denmark, and is responsible for post-market research.
Brad A. Stach, PhD, is Director of the Division of Audiology, Department of Otolaryngology-Head and Neck Surgery, of the Henry Ford Medical Group in Detroit, Michigan. He also oversees the clinical education component of the AuD program at Wayne State University. Dr. Stach is a founding board member and past President of the American Academy of Audiology and is the Audiology Editor-in-Chief for Plural Publishing.
Erica Bennett, AuD, PhD, is a senior staff audiologist at Henry Ford Health. She earned her AuD and PhD from the University of Wisconsin.
Josephine Marino, AuD, is a member of the audiology department at ENT Specialty Care of Minnesota.
Virginia Ramachandran, AuD, PhD, is the Head of Audiology at Oticon Inc. Dr. Ramachandran is a past president of the American Academy of Audiology. She currently serves on the Audiology Editorial Board of Plural Publishing Inc.
References
Bernstein, J. G. W., Mehraei, G., Shamma, S., Gallun, F. J., Theodoroff, S. M., & Leek, M. R. (2013). Spectrotemporal Modulation Sensitivity as a Predictor of Speech Intelligibility for Hearing-Impaired Listeners. Journal of the American Academy of Audiology, 24(04), 293–306. https://doi.org/10.3766/jaaa.24.4.5
Bilodeau-Mercure, M., Lortie, C. L., Sato, M., Guitton, M. J., & Tremblay, P. (2015). The neurobiology of speech perception decline in aging. Brain Structure and Function, 220(2). https://doi.org/10.1007/s00429-013-0695-3
Carhart, R., & Tillman, T. W. (1970). Interaction of Competing Speech Signals With Hearing Losses. Archives of Otolaryngology – Head and Neck Surgery, 91(3), 273–279. https://doi.org/10.1001/archotol.1970.00770040379010
Fitzgerald, M. B., Gianakas, S. P., Qian, Z. J., Losorelli, S., & Swanson, A. C. (2023). Preliminary Guidelines for Replacing Word-Recognition in Quiet With Speech in Noise Assessment in the Routine Audiologic Test Battery. Ear & Hearing,44(6), 1548–1561. https://doi.org/10.1097/AUD.0000000000001409
Fostick, L., Ben-Artzi, E., & Babkoff, H. (2013). Aging and speech perception: Beyond hearing threshold and cognitive ability. Journal of Basic and Clinical Physiology and Pharmacology, 24(3). https://doi.org/10.1515/jbcpp-2013-0048
Jason Qian, Z., Vaisbuch, Y., Gianakas, S. P., Tran, E. D., Ali, N. E. S., Blevins, N. H., & Fitzgerald, M. B. (2023). Evaluation of Asymmetries in Speech-in Noise Abilities in Audiologic Screening for Vestibular Schwannoma. Ear and Hearing, 44(6). https://doi.org/10.1097/AUD.0000000000001397
Jerger, J., & Jerger, S. (1971). Diagnostic Significance of PB Word Functions. Archives of Otolaryngology, 93(6), 573–580. https://doi.org/10.1001/ARCHOTOL.1971.00770060875006
Killion, M. C., Niquette, P. A., Gudmundsen, G. I., Revit, L. J., & Banerjee, S. (2004). Development of a quick speech-in-noise test for measuring signal-to-noise ratio loss in normal-hearing and hearing-impaired listeners. The Journal of the Acoustical Society of America, 116(4), 2395–2405. https://doi.org/10.1121/1.1784440
Le Prell, C. G., & Clavier, O. H. (2017). Effects of noise on speech recognition: Challenges for communication by service members. Hearing Research, 349, 76–89. https://doi.org/10.1016/j.heares.2016.10.004
McRackan, T. R., Ahlstrom, J. B., Clinkscales, W. B., Meyer, T. A., & Dubno, J. R. (2016). Clinical implications of word recognition differences in earphone and aided conditions. Otology and Neurotology, 37(10). https://doi.org/10.1097/MAO.0000000000001205
Mehraei, G., Gallun, F. J., Leek, M. R., & Bernstein, J. G. W. (2014). Spectrotemporal modulation sensitivity for hearing-impaired listeners: Dependence on carrier center frequency and the relationship to speech intelligibility. The Journal of the Acoustical Society of America, 136(1). https://doi.org/10.1121/1.4881918
Middelweerd, M. J., Festen, J. M., & Plomp, R. (1990). Difficulties with speech intelligibility in noise in spite of a normal pure-tone audiogram: Original papers. International Journal of Audiology, 29(1). https://doi.org/10.3109/00206099009081640
Nilsson, M., Soli, S. D., & Sullivan, J. A. (1994). Development of the Hearing In Noise Test for the measurement of speech reception thresholds in quiet and in noise. The Journal of the Acoustical Society of America, 95(2), 1085–1099. https://doi.org/10.1121/1.408469
Santurette, S. & Laugesen, S. (2023). Audible Contrast Threshold (ACTTM) Science made smarter ABR OAE Balance Tympanometry Audiometry Hearing Aid Fitting A language-independent diagnostic test to quantify real-life speech-in-noise ability and personalise help-in-noise settings in hearing aids EDITORS OF ISSUE (Issue 2). ACTTM
Saunders, G. H., & Haggard, M. P. (1989). The clinical assessment of obscure auditory dysfunction 1. auditory and psychological factors. Ear and Hearing, 10(3). https://doi.org/10.1097/00003446-198906000-00011
Tremblay, P., Brisson, V., & Deschamps, I. (2021). Brain aging and speech perception: Effects of background noise and talker variability. NeuroImage, 227. https://doi.org/10.1016/j.neuroimage.2020.117675
Vermiglio, A. J., Soli, S. D., & Fang, X. (2018). An argument for self-report as a reference standard in audiology. Journal of the American Academy of Audiology, 29(3). https://doi.org/10.3766/jaaa.16128
Vermiglio, A. J., Soli, S. D., Freed, D. J., & Fisher, L. M. (2012). The Relationship between High-Frequency Pure-Tone Hearing Loss, Hearing in Noise Test (HINT) Thresholds, and the Articulation Index. Journal of the American Academy of Audiology, 23(10), 779–788. https://doi.org/10.3766/jaaa.23.10.4
Wilson, R. H. (2011). Clinical Experience with the Words-in-Noise Test on 3430 Veterans: Comparisons with Pure-Tone Thresholds and Word Recognition in Quiet. Journal of the American Academy of Audiology, 22(07), 405–423. https://doi.org/10.3766/jaaa.22.7.3
Wilson, R. H., McArdle, R. A., & Smith, S. L. (2007). An Evaluation of the BKB-SIN, HINT, QuickSIN, and WIN Materials on Listeners With Normal Hearing and Listeners With Hearing Loss. Journal of Speech, Language, and Hearing Research, 50(4), 844–856. https://doi.org/10.1044/1092-4388(2007/059)
Zaar, J., Ihly, P., Nishiyama, T., Laugesen, S., Santurette, S., Tanaka, C., Jones, G., Vatti, M., Suzuki, D., Kitama, T., Ogawa, K., Tchorz, J., Shinden, S., & Jürgens, T. (n.d.). Predicting speech-in-noise reception in hearing-impaired listeners with hearing aids using the Audible Contrast Threshold (ACTTM) test.
Zaar, J., Simonsen, L. B., Dau, T., & Laugesen, S. (2023). Toward a clinically viable spectro-temporal modulation test for predicting supra-threshold speech reception in hearing-impaired listeners. Hearing Research, 427. https://doi.org/10.1016/j.heares.2022.108650
Zaar, J., Simonsen, L. B., & Laugesen, S. (2024). A spectro-temporal modulation test for predicting speech reception in hearing-impaired listeners with hearing aids. Hearing Research, 443. https://doi.org/10.1016/j.heares.2024.108949
Zaar, J., Simonsen, L. B., Sanchez-Lopez, R., & Laugesen, S. (n.d.). The Audible Contrast Threshold (ACTTM) test: a clinical spectro-temporal modulation detection test. https://doi.org/10.1101/2023.10.12.23296977
Figure Captions:
Figure 1: Percentage of patients who fell within each category of amount of normalized contrast loss.
Figure 2: Individual ACT values (y-axis) by patient pure tone average (x-axis) for patients with symmetric hearing.
Figure 3: Average ACT value (y-axis), ± standard error, by patient age (x-axis) for patients with symmetric hearing.
Figure 4: Percentage of patients with normal hearing who had normal (blue bars) and elevated ACT values (orange bars). Patients are divided into two groups along the x-axis, those with a chief complaint of hearing loss and those without.
Figure 5: Individual ACT values (y-axis) by patient word recognition scores (x-axis) for patients with symmetric hearing.
Figure 6: Percentage of patients in each category of amount of normalized Contrast Loss for patients with scores of 100% on word recognition in quiet.