The current standard of care for patients who have received cochlear implants includes as many as eight follow-up appointments at an audiology clinic during the first year after surgery. A recent study sought to determine if fewer post-surgery visits scheduled at key intervals could provide the same standard of care while providing additional benefits.
Sandra Porps, AuD, of the Michigan Ear Institute in Farming Hills, Mich., was the lead author of the study, published in the journal Cochlear Implants International. “We wanted to see if we could use a reduced visit schedule to make things more efficient for the patient and the clinics while still having the same satisfaction outcomes,” she says. Porps and her team were approached by Cochlear to conduct the study, which involved five experienced clinicians and three centers: Michigan Ear Institute, Cochlear Hearing Center in Bellaire, Texas, and Texoma Hearing Institute in Wichita Falls, Texas.
First, the team identified 17 adults who were either newly implanted or were about to undergo cochlear implant surgery to participate in the study. Then they decided on a four-appointment evidence-based model blended with remote care, which was very different from what Porps and her colleagues had been doing.
Improving on the Traditional Model
The traditional model of aftercare for newly implanted CI recipients involves activation and follow-ups at one week, two weeks, three weeks, one month, three months, six months, and eventually once a year. “That meant 7 to 8 visits in the first year, which was a lot of time for our recipients to commit to,” Porps says. “That’s also a lot of chair time for our audiologists.”
Having to devote so much time to multiple appointments for cochlear implant patients limits the number of patients they can see. And that includes potential implant recipients, who often have to be put on wait lists and “go without sound” for an extended period of time. “Nobody wants that,” Porps adds. “We aim to get everyone implanted as quickly as they want.”
Reduced Treatment Schedule
The reduced treatment schedule used for the study consisted of an initial appointment at activation followed by an appointment at one month, three months, six months, and then once a year. “That brought us down to four to five visits because we tried to do some of those visits remotely,” Porps explains.
Before arriving at the four-appointment model, she and her team evaluated multiple models in the United States and Europe to determine the best ways to approach reducing the number of appointments. They asked themselves:
- Where can the number of appointments be reduced?
- When should it be reduced?
- Should it be reduced on the front end when patients are just getting familiar with their implants, or should it be reduced later on?
- How can it be done in a way that makes sense for the patients and the clinics?
- Then as they followed the four-appointment model, Porps and her team evaluated areas of the study by asking these questions:
- Do patients like this?
- Do patients prefer this to the traditional model? If they do, are they doing as well?
- Are their hearing outcomes similar to what they would have been with the traditional model?
- Is seeing patients in this reduced visit schedule effective in terms of their hearing outcomes, and are the patients satisfied?
- Do patients feel they’re getting the same level of care as they would through the traditional model?
Remote Care
Another major aspect of the study and its model was remote care. This component allowed Porps and the other audiologists to check in with study participants in between visits without them having to physically come into the clinic.
While most participants were reluctant at first, they quickly came around when they realized the technology they’d be using for remote care virtual visits wasn’t as complicated as they’d feared. When asked if they ever used FaceTime, most responded that they frequently did and were comfortable with that technology. Porps says she was able to assure study participants, “If you can FaceTime with your grandkids, you can do remote care.”
In fact, as far as the patient is concerned, Cochlear’s Remote Assist seems very much like a FaceTime video call. “I’m on my computer at the clinic, and the patient is on their phone at home,” she explains. “We can take control of the implant by using Remote Assist and make some adjustments if needed.”
In some ways, a video call was better than an office visit because it gave the audiologists more insight into how the study participants were using their cochlear implants on a daily basis. “It was a benefit for counseling our patients because this allowed us to see them in their home environment,” she says. “We can see where they are sitting, watching TV, or where they are talking to each other.”
Porps and her team also used Cochlear’s Remote Check, an at-home, clinician-enabled cochlear implant testing tool, to troubleshoot and see how patients were doing virtually. They were able to assess: Are they progressing? Are they hearing better in speech and noise? Are they meeting those audiological outcomes in terms of where their hearing thresholds are?
“So even though we weren’t seeing our patients as often in person, we had those check-ins via remote care,” Porps says.
Patient Satisfaction
At the end of the study, participants indicated they were satisfied with their remote care experience as well as the reduced appointment schedule.
When it came to remote care, “Every single patient said, ‘This is easier than I thought!’” And for the overall evidence-based model, “100% of the recipients that took the final survey rated the care as excellent,” Porps says. “That was above and beyond our expectations.”
But considering the benefits, the results don’t seem that surprising. “For the patient, it was less chair time, less time off work, and less driving to the clinic. All of those things had a positive impact,” Porps says.
Further reading: A Conversation on Patient Care with an Audiologist Living with Cochlear Implants
Adopting the New Model
Other audiology clinics are already adopting the evidence-based four-appointment model used in the study. Porps says, “I’ve talked to a lot of clinics about the study even before the article was published and explained how it’s worked for us, and I’ve gotten to hear from a number of clinics that have said, ‘We’re doing this, we’re dipping our toes in, and it’s going well.’”
Because the results of the study were so positive, she has high hopes the four-appointment model will become the new standard in cochlear implant patient aftercare treatment. She acknowledges that it won’t work for every patient, but she doesn’t see that as a negative.
“We estimate that around 80% of recipients will be able to use a model like this,” Porps says. “There will always be people who need a little more care, and that’s perfectly fine. You now have more time to care for those patients because you have more openings on your schedule.”
This model might also not work for every audiologist or every clinic, but it doesn’t have to be adopted wholesale to make a positive difference in CI aftercare.
“If you take nothing else from this paper, look at your own protocol and see if your current after-care model works for you and your patients,” urges Porps. “And if this four-appointment model isn’t a great fit for you, it can be modified to work for you.”
The article “Effects of an evidence-based model for cochlear implant aftercare delivery on clinical efficiency and patient outcomes” published in Cochlear Implants International is Open Access so that anyone interested can read it to learn more about the study.
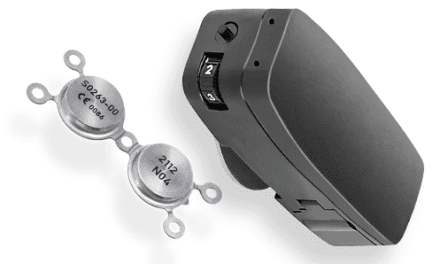
Featured image: Remote care appointments allowed audiologists to check in with study participants in between in-person visits. Photo: Cochlear