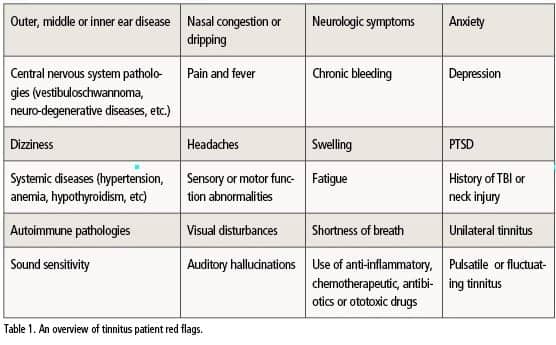
Tech Topic | May 2016 Hearing Review
Part 1
Hearing care professionals need to be able to recognize which tools in their tinnitus toolbox to utilize on a patient-by-patient basis, and be aware of research to help make navigation of this an easier process for both the clinician and the patient.
Since the inception of audiology in the 1950s, treatment and assessment have slowly become cornerstones of tinnitus patient care. Tinnitus management has been a major topic in audiology, especially in the past several years. Assessment, evaluation, and counseling tools are now available for hearing care professionals who would like to add tinnitus care to their practice. Hearing instrument manufacturers have addressed this need by adding tinnitus-specific features into their hearing instruments and even introduced new and innovative ways to treat tinnitus via smart phone applications.1 Tinnitus treatment options are abundant and online resources are increasingly available for people who would like to learn about their condition.
The American Tinnitus Association (ATA) estimates that 50 million people in the United States experience tinnitus to some degree.2,3 Approximately 16 million people seek medical attention for their tinnitus, and tinnitus affects the daily lives for up to 2 million patients.4 The overall increase in patient awareness has, in turn, brought more people into hearing care clinics to seek help.
Part I of the “Tinnitus Toolbox” is a comprehensive guide for hearing care professionals to successfully navigate a best practices assessment protocol for their patients presenting with tinnitus.
Common Tinnitus Care Challenges
While the assessment portion of patient care is an imperative part of quantifying and documenting a diagnosis of tinnitus, it is just as important to be able to provide well-rounded, scientifically based patient care post assessment. The hearing care professional also has to be able to communicate effectively with the patient, categorize the tinnitus and document it, and get a baseline to not only establish where the patient currently is, but also use the baseline to determine how effective treatment has been.5
Perhaps one of the challenging aspects of working with tinnitus patients is reimbursement. Reimbursement with the Current Procedural Terminology (CPT) code 92625 (Assessment of Tinnitus) has been available since 2005 and remains for the 2016 Medicare Physician Fee Schedule (2016 Medicare Fee Schedule for Audiologists).6 It should be noted that to use this code the provider must perform pitch matching, loudness matching, and maskability for both ears.3
However, outside of assessment, there is limited insurance reimbursement for many additional aspects of tinnitus care. For example, long-term treatment does not have a designated code; therefore, more comprehensive tinnitus management strategies, such as Tinnitus Retraining Therapy (TRT) and Cognitive Behavioral Therapy (CBT), may not be reimbursed by insurers. Both TRT and CBT require an extended timeline with regularly scheduled appointments that must be kept.7 For the audiologists who offer tinnitus services, this revenue challenge leaves them with the not uncommon quandary of providing uncompromised patient care while keeping in mind the financial implications and feasibility.8
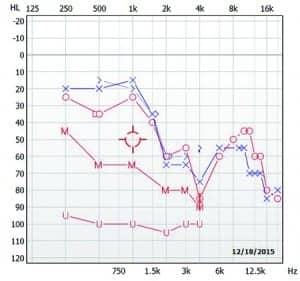
Hearing Assessment
For the hearing evaluation component, it is often useful to obtain high frequency audiometry with inter-octaves and an increased resolution around the area of the suspected tinnitus (Figure 1). For example, you may test 1,500, 3,000 and 6,000 Hz and determine threshold utilizing 2 dB steps instead of 5 dB. This can be useful particularly for patients who have normal or symmetrical audiological pure-tone results between 250-8,000 Hz. Obtaining Most Comfortable Levels (MCLs) and Uncomfortable Loudness Level (UCLs) for pure-tones gives an indication of the patient’s residual dynamic range or an indication of hyperacusis. As with any patient undergoing audiological evaluation, speech recognition thresholds and word recognition scores should also be obtained.11
In addition to the audiogram, middle-ear status should be verified by performing tympanometry and high frequency Otoacoustic Emissions (OAEs), preferably including frequencies above 8,000 Hz. Specifically, Distortion Product Otoacoustic Emissions (DPOAEs) completed with 5 points per octave can be useful for patients with normal hearing thresholds, as hearing loss can often be detected via OAEs prior to seeing any pure tone shifts on the audiogram.14
Tinnitus & Other Questionnaires
Questionnaires can garner important information from the patient about their current tinnitus management, if any, as well as facilitate discussion by giving the provider a framework in which to begin counseling. Information from these questionnaires can also provide an initial baseline for how the patient is coping with their tinnitus prior to, during, and at the conclusion of their time with the clinician.15 While there are many different questionnaires available for tinnitus assessment, the two most commonly used are the Tinnitus Handicap Inventory (THI)15 and the Tinnitus Functional Index (TFI).16

Figure 2. Excerpt from the Tinnitus Functional Index questionnaire in the MADSEN Astera2 Tinnitus Module.
Figure 2 provides an excerpt from the TFI. These two questionnaires not only give a variety of easy-to-score and comprehensive questions, but they have been validated in numerous studies as effective measures of tinnitus quantification.3 Both are brief, containing only 25 questions each, and when utilized in a baseline assessment, can be used as benchmarks for patient success post tinnitus management.
Hearing care professionals are naturally inclined to focus on the hearing aspect of tinnitus symptoms. However, it’s imperative to take a more universal approach to these patients and consider concomitant medical issues. For example, of all tinnitus patients, it is estimated that “approximately 35% have anxiety, 13-28% have depression, and 25% exhibit psychiatric disorder, all of which can contribute to the negative feedback loop, or vicious cycle,” that tinnitus can foster.13,17 So, while planning a thorough tinnitus evaluation, other types of validated, psychoanalytical questionnaires can be useful in determining if a referral needs to be made to a mental health professional. These can include the Beck Depression Survey, the Spuelberger State-Trait Anxiety Inventory, and the Primary Care PTSD survey.
A cursory review of current medications, while not imperative, can also give you some indication if the tinnitus is medically induced. However, all questions about medications and their interactions should be routed through the prescribing physician.13
Tinnitus Assessment
After performing the comprehensive audiological assessment and obtaining the appropriate questionnaire results, the final piece of a tinnitus evaluation is quantifying the tinnitus through measures such as Pitch Matching, Loudness Matching, and Residual Inhibition. Characterizing the subjective symptoms improves communication between the clinician and the patient and provides a documented basis for treatment. A tinnitus evaluation is typically associated with tests such as pitch matching and minimum masking levels, and those measures are needed for reimbursement as noted above. While these measures are useful in understanding and documenting a patient’s tinnitus, a thorough hearing assessment and tinnitus questionnaires provide important additional information that can assist in a differential diagnosis. Numerous resources have been published regarding tinnitus assessment and subtests, including the American Academy of Audiology and the American Academy of Otolaryngology-Head & Neck Surgery’s guidelines for the assessment and treatment of tinnitus patients.9-12
Figure 3 shows a preview of the tinnitus tab for the MADSEN® Astera2 by Otometrics, which has all of the necessary components for a tinnitus evaluation built into the software. In this example, since only the right ear has been assessed, a-52 modifier to the CPT code would be needed if no further testing was performed.
Conclusions
After leaving the defined harbor of a tinnitus evaluation, navigating the sea of tinnitus treatment options can be overwhelming. Each patient has unique experiences, comorbidities, and even perceptions of their tinnitus that can further complicate the therapy process, even for the most skilled clinician.
While there are promises of medical and minimally invasive approaches, currently the hearing care professional needs to be able to recognize which tools in their tinnitus toolbox to utilize on a patient-by-patient basis, and be aware of current and upcoming research to help make navigation of this an easier process for both the clinician and the patient.
References
-
Martin WH. Tinnitus care: what should I know when starting to provide tinnitus care? November 24, 2014. Available at: http://www.audiologyonline.com/articles/tinnitus-care-what-should-i-13109
-
American Tinnitus Association. Understanding the facts. Available at: https://www.ata.org/understanding-facts
-
Sanchez C, Switalski W. Tinnitus patient management for today’s audiologists. Audiology Today. 2015;27(2), 14-21.
-
Dobie R. What is tinnitus? Available at: http://hearinghealthfoundation.org//index.php?pg=what_is_tinnitus
-
Switalski W, Sanchez C. Tinnitus assessment: The key to successful tinnitus patient management [white paper]. Available at: http://www.audiologysystems.com/education/hearing-assessment-resources
-
American Speech-Language-Hearing Association. 2016 Medicare Fee Schedule for Audiologists. November 10, 2015. Available at: http://www.asha.org/uploadedFiles/2016-Medicare-Physician-Fee-Schedule-Audiology.pdf ; February 24, 2016.
-
Cima RFF, Andersson G, Schmidt CJ, Henry JA. Cognitive-behavioral treatments for tinnitus: a review of the literature. J Am Acad Audiol. 2014;25:29-61.
-
Piskosz M. How to establish a successful tinnitus clinic. Hearing Review. 2013;20(5)[May]:16-22. Available at: https://hearingreview.com/2013/05/how-to-establish-a-successful-tinnitus-clinic2
-
American Academy of Audiology. Audiologic guidelines for the diagnosis & management of tinnitus patients. October 18, 2000. Available at: http://www.audiology.org/publications-resources/document-library/tinnitus
-
Tunkel DE, Bauer CA, Sun GH, et al. Clinical practice guideline: Tinnitus. Otolaryngol–Head Neck Surg. 2014;151(2S):S1–S40. Available at: http://oto.sagepub.com/content/151/2_suppl/S1.full.pdf+html
-
Henry JA, Zaugg TL, Schechter MA. Clinical guide for audiologic tinnitus management I: Assessment. Am J Audiol. 2005;14, 21-48.
-
Jastreboff PJ, Hazell JW. A neurophysiological approach to tinnitus: clinical implications. Brit J Audiol. 1993;27(1):7-17.
-
Shi Y. Robb MJA, Michaelides EM. Medical management of tinnitus: role of the physician. J Am Acad Audiol. 2014;25:23-28.
-
Littman TA, Magruder A, Strother DR. Monitoring and predicting ototoxic damage using distortion-product otoacoustic emissions: pediatric case study. J Am Acad Audiol. 1998;9:257-262.
-
Newman CW, Sandridge SA, Jacobson GP. Psychometric adequacy of the tinnitus handicap inventory (THI) for evaluating treatment outcome. J Am Acad Audiol. 1998;9:153-160.
-
Meikle MB1, Henry JA, Griest SE, et al. The tinnitus functional index: Development of a new clinical measure for chronic, intrusive tinnitus. Ear Hear. 2012; 33(2)[Mar-Apr]:153-76.
-
McKenna L, Andersson G. Changing reactions to tinnitus. Hearing Review. 2007;14(9)[Aug]:12-19. Available at: https://hearingreview.com/2007/08/changing-reactions-to-tinnitus
Correspondence can be addressed to Hearing Review or Dr Young at: [email protected]
Original citation for this article: Young B, Boorazanes M, Sanchez C. The Tinnitus Toolbox Guide to Support the Full Patient Journey, Part 1. Hearing Review. 2016;23(5):24.?







While we may not be able to address tinnitus as well as we would like as audiologists, we do have some areas of success (tinnitus masking) with small groups of patients. Limitations for success are dependent on the complexities of the pathology itself or, maybe better stated, the causation of the pathology.
Even in this report, you outline well these complexities.
If I may address one aspect that at the very least, may provide information that might provoke some additional thoughts and open some dialog regarding tinnitus concerns within these areas of health issues.
In your box diagram you list a number of areas where tinnitus is a symptom of pathologies. The one area of my interest is dealing with Autoimmune related pathologies. I’ve been reviewing research in the radical cell biology arena over the past five years as related to autoimmune disease. My original search revealed over 40,000 studies on oxidative stress (causation for autoimmune diseases), this same search today yields nearly 160,000.
This should suggest for even the most novice of readers that there is a growing interest in medical science regarding what is happening at the cellular level in our bodies that trigger these disease processes. Audiology should not be any different. We should be looking at a much smaller level than starting at the ear and working backwards to find the solution.
You did mention, “of all tinnitus patients, it is estimated that “approximately 35% have anxiety, 13-28% have depression, and 25% exhibit psychiatric disorders”. These too have an oxidative stress component.
So what are our research colleagues in the cellular biology world saying about this? Well, that requires an extensive lecture to explain, but in a nut shell, here is where medical science is heading.
Currently we know that if a few cellular pathways as part of the aging process start to slow down, the production of the expressions of the genes within our DNA that are responsible for our cellular and ultimately our bodies [begin to change and affect our] health. One recently discovered is our Nrf2 pathway. Nrf2 is a protein responsible for the continued activation of our autoimmune response element (ARE) of our DNA. This is a group of nearly 500 genes whose genomic expressions are responsible for reducing free radicals, preventing disease pathologies, and maintaining overall cellular health. In one recent study, the authors went so far as to say Nrf2 will be recognized as the single most important discovery in medical history. I tend to agree with this statement.
Even more recent is the discovery of the NRF1 pathway (also slowed due to the aging process). These two pathways are involved in the overall health, cellular function, and genomic expression of over 1,500 genes who by design are the key to prevention of nearly every disease processes our bodies can produce.
The fact is that our aging processes cause these proteins to slow down–[the slowed] production of these genomic expressions is why we age quickly and develop diseases. So that said, what can we do?
There are currently three known products on the market today that are ‘researched’ genomic up regulators. Suggesting that when taken these products activate NRF1, Nrf2 and molecular hydrogen production throughout our bodies. I have been taking the Nrf2 herbal supplement for five years now. After 15 years of severe tinnitus (thinking there could never be a solution) I was introduced to a new Nutragenomic Nrf2 activator, and within two weeks my tinnitus shut off like someone hit a light switch. ****it wasn’t the product that ‘treated my tinnitus’, but by up regulating the Nrf2, it up regulated the ARE genomic expressions, thus reducing free radicals and allowing the cells to treat themselves through these genomic expressions.
These same healing processes can occur when we can up regulate hydrogen production in our bodies and now a brand new product (which I will be adding to my supplement regime this week) will be launched on Tuesday of this week which is a NRF1 activator.
We as audiologists can get on this trend with other medical community colleagues by taking a very serious look at what these products are doing.
There already have been a few studies looking at these approaches. One study suggests if we can reduce free radicals or oxidative stress by as much as 10% (Nrf2 activator reduces oxidative stress by an average of 40% in 30 days), it may completely eliminate hearing loss due to the aging process (oxidative stress). Other reports are suggesting an injection into the cochlea may prevent noise induced hearing loss. I’ve explained my reversed tinnitus and can say that I have 10 patients on this Nrf2 product with diagnosed Menieres Disease that haven’t had any attack since taking it.
There are many pathologies that are oxidative stress related in onset, that have vestibular and hearing related symptoms that we can assist with just a little cellular biology understanding.
I hope you find this helpful.
Larry G. Martin, AuD, ([email protected])