Case Study | Pediatrics | January 2015 Hearing Review
A reminder of what our tests really say about the auditory system.
How many times have I heard— and said myself—that the OAE is not a hearing test? How many times have I thought to myself that, just because a child passes their newborn hearing screening test, it does not mean they have normal hearing? This case brought those two statements front and center.
A 5-year-old boy was referred to me for a hearing test because he did not pass a kindergarten screening test in his right ear. His parents reported that he said “Huh?” frequently, and more recently they noticed him turning his head when spoken to. He had passed his newborn hearing screening, and he had experienced a few ear infections that responded well to antibiotics. The parents mentioned a maternal aunt who is “nearly totally deaf” and wears binaural hearing aids.
Initial Test Results
Otoscopic examination showed a clear ear canal and a normal-appearing tympanic membrane on the right side. The left ear canal contained non-occluding wax.
Tympanograms were within normal limits bilaterally. Unfortunately, otoacoustic emissions (OAE) testing could not be completed because of an equipment malfunction.
Behavioral testing with SRTs was taken, and I typically start with the right ear. The child seemed bright and cooperative enough for routine testing. I obtained no response until 80 dB.
I switched to the left ear and he responded appropriately. This prompted me to walk into the test booth and check the equipment and wires; everything was plugged in and looked normal. I tried SRTs again with the same results, even reversing the earphones. Same results. When the behavioral tests were completed, the results indicated normal hearing in his left ear and a profound hearing loss in his right ear.
The child’s parents were informed of these results, and we scheduled him to return for a retest in order to confirm these findings.
Follow-up Test
One week later, the boy returned for a follow-up test. The otoscopic exam was the same: RE = normal; LE = non-occluding wax.
Tympanograms were within normal limits. I added acoustic reflexes, which were normal in his left ear (80-90 dB), and questionable in his right ear (105-115 dB).
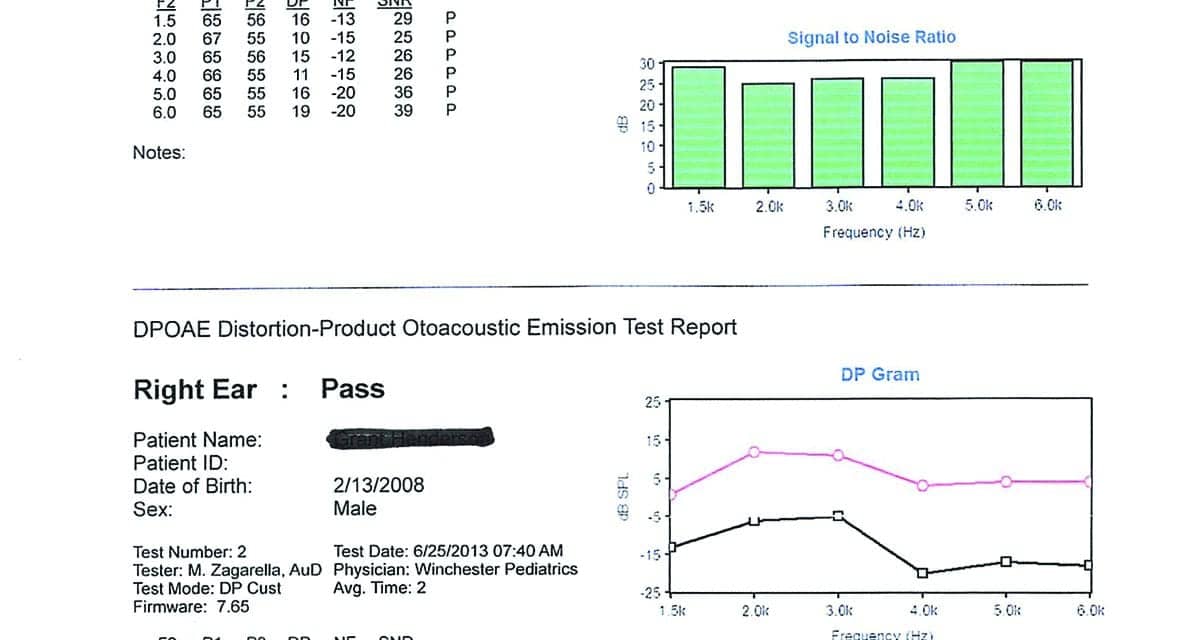
DPOAEs were present in both ears. The right ear was reduced in amplitude compared with the left, but not what I would expect to see with a profound hearing loss (Figure 1).
I repeated the behavioral tests with the same results that I obtained the first time (Figure 2). Bone conduction scores were not obtained at this time because I felt I was reaching the limits of a 5-year-old, and the tympanograms were normal on two occasions.
Recommendation to Parents
After completing the tests, I explained auditory dyssynchrony to the parents, and told them that this is what their son appeared to have. Since they were people with resources, I advised them to make an appointment at Johns Hopkins to have this diagnosis confirmed by ABR.
Johns Hopkins Results
The initial appointment at Johns Hopkins was at the ENT clinic. According to the report from the parents, the physician reviewed my test results and said it was unlikely that they were valid. She suggested they repeat the entire test battery before proceeding with an ABR. All peripheral tests were repeated with exactly the same results that I had obtained. The ABR was scheduled and performed, yielding:
“Findings are consistent with normal hearing sensitivity in the left ear and a neural hearing loss in the right ear consistent with auditory dyssynchrony (auditory neuropathy). The normal hearing in the left ear is adequate for speech and language development at this time.”
Additional Follow-up
The boy’s mother was not completely satisfied with the diagnosis or explanation. After she arrived home and mulled things over, she called Johns Hopkins and asked if they could do an MRI. The ENT assured her that it probably would not show anything, but if it would allay her concerns (and since they had good insurance coverage), they would schedule the MRI.
Further reading: Vestibular Assessment in Infant Cochlear Implant Candidates
Findings of MRI. Evaluation of the right inner ear structures demonstrated absence of the right cochlear nerve. The vestibular nerve is present but is small in caliber. The internal auditory canal is somewhat small in diameter. There is atresia versus severe stenosis of the cochlear nerve canal. The right modiolus is thickened. The cochlea has the normal amount of turns, and the vestibule semicircular canals appear normal.
The left inner ear structures, cranial nerves VII and VIII complex, and internal auditory canal are normal. Additional normal findings were also presented regarding sinuses, etc.
Key finding: The results were consistent with atresia versus severe stenosis of the right cochlear nerve canal and cochlear nerve and deficiency described above.
The Value of Relearning in Everyday Clinical Practice
According to the MRI, the cochlea on the right side is normal—which would explain the present DPOAE results. The cochlear branch of the VIIIth Cranial Nerve is completely absent, which would explain the absent ABR result and the profound hearing loss by behavioral testing.
This case has certainly caused me to re-evaluate what I think and say about my test findings. How many times have I heard—and said myself!—that the OAE is not a hearing test? How many times have I thought to myself that, just because a child passes their newborn hear- ing screening test, it does not mean that they have normal hearing?
This case has surely brought those two statements front and center. In addition, what about auditory neuropathy? In about 40 years of testing, I had never seen a case that I was convinced was AN. Naturally, I was somewhat skeptical about this disorder: Is it real, or does it reside in the realm of the Yeti. (Personal note to Dr Chuck Berlin: I truly don’t doubt you, but I do like to see things for myself!)
Finally, this case only reinforces my trust in “mother’s intuition” and the value of deferring to the sensible requests of parents. If she had not felt uneasy about what she had been told at one of the most prestigious clinics in the country, the actual source of this problem would not have been discovered.
So what? Does any of this really make a difference? The bottom line is we have a 5-year-old boy with a unilateral profound hearing loss. How important is it that we know why he has that loss? From a purely clinical standpoint, I think that it is poignant because it brings home the importance of understanding what our tests really say about the hearing mechanism and auditory system (ie, is working or not working?).
And although it may not make a large difference in the boy’s current treatment plan, I do know that the boy’s mother is grateful for understanding the reason for her son’s hearing loss and that it’s at least possible the boy may benefit from this knowledge in the future.
Michael Zagarella, AuD, is an audiologist at RESA 8 Audiology Clinic in Martinsburg, WVa.
Correspondence can be addressed to HR or or Dr Zagarella at: [email protected]
Citation for this article: Zagarella M. Case study of a 5-year-old boy with unilateral hearing loss. Hearing Review. 2015;22(1):30-33.