Patient Care | October 2022 Hearing Review
Migraine affects nearly 40 million individuals in the United States, more than asthma and diabetes combined. Most will have dizziness, vertigo, misophonia, and hyperacusis with or without a headache.
By Richard E. Gans, PhD, and Joseph Sakumura, AuD
It is difficult to believe that it has been 20 years since our first series on the audiovestibular aspects of migraine in children and adults was published in Hearing Review.1 In 2002, there was not much written in the audiology and otolaryngology literature about migraine and its varied and common manifestations affecting the peripheral and central auditory and vestibular pathways. In fact, many experts were slow to recognize that there was any correlation with migraine and auditory-vestibular symptoms. Perhaps the greatest change in medical practice has been the rethinking of diagnostic categorization of “atypical or non-classic” Ménière’s disease (MD), now widely accepted as vestibular migraine (VM).2 Symptoms include episodic dizziness or vertigo without fluctuating sensorineural hearing loss or tinnitus. It is mostly seen in females of childbearing age, often associated with the monthly menses cycles.
The first of this three-part series will focus on the updated description, prevalence, and latest International Headache Societies’ criteria of migraine. The second article will review the research and clinical experiences detailing the abnormal findings often associated with migraine on the neurodiagnostic auditory-vestibular test battery, including case studies. The final article will discuss pediatric migraine both Benign Paroxysmal Vertigo (BPV) and puberty onset, as well as a myriad of other associated conditions including migrainous positional vertigo (MPV) and persistent postural-perceptual dizziness (PPPD). The objective is to provide the reader with an appreciation of one of the most common conditions presenting with auditory-vestibular symptoms.
Migraine Update 2022
Two decades ago, neurologists were still referring to the first publication of the International Classification of Headache Disorders (ICHD) (International Headache Society IHS) to make a diagnosis. Since then, there have been two significant updates in 20043 and 20184 and a fourth is in preparation now. Per the IHS 2018 report, migraine is described as a common disabling primary headache disorder. Many epidemiological studies have documented its high prevalence and socioeconomic and personal impacts. The Global Burden of Disease Study 20105 (GBD 2010), it was ranked as the third most prevalent disorder in the world. In GBD 2015,6 it was ranked the third highest cause of disability worldwide in both males and females under the age of 50 years. The prevalence of migraine is one in four females and one in six males. The global definition of migraine remains as a “genetic or familial neurologic condition.”
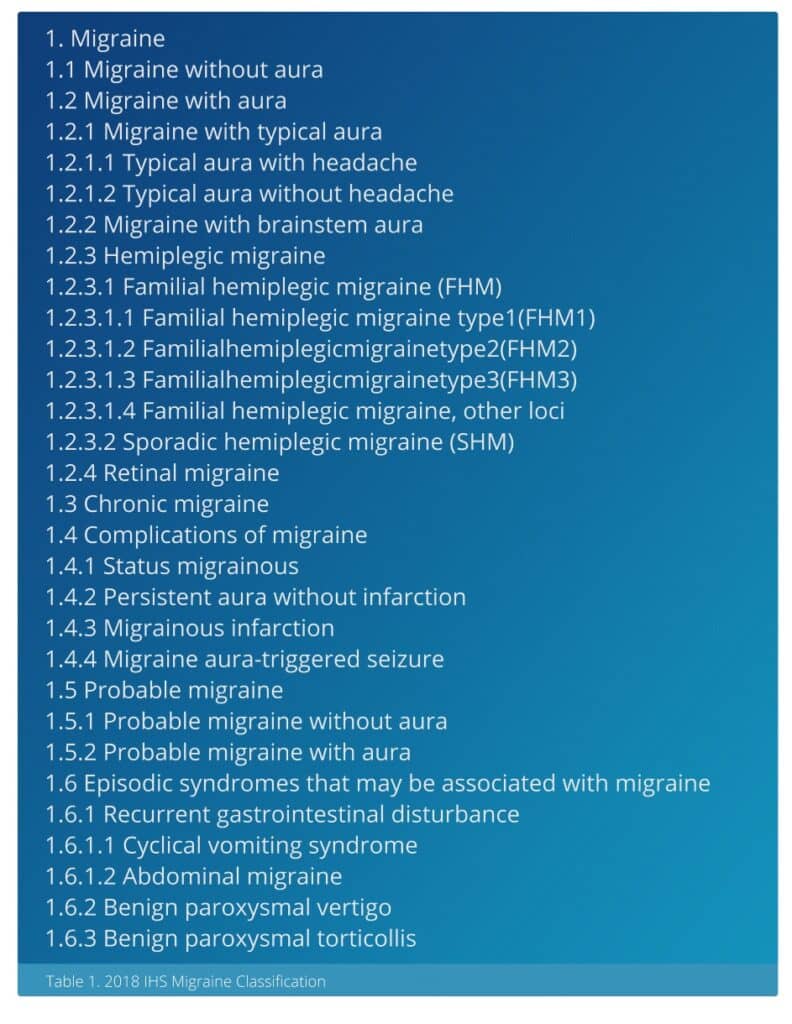
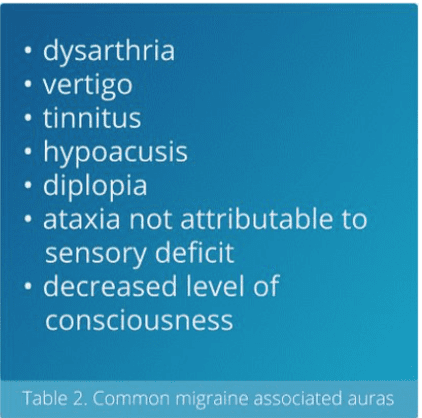
As can be seen in Table 1, according to the latest 2018 IHS guidelines, there are six primary categories of migraine with almost 30 subcategories. Migraine cannot be dismissed as merely a headache when there are so many associated symptoms. In general, the two major differentiations are migraine with aura and migraine without aura. An aura is best described as an abnormal sensory perception other than headache. Table 2 provides a list of the most common auras, many of which have an audiovestibular context. While fluctuating sensorineural hearing loss is not listed, it has been reported to occur in about 5% of migraine patients. Interestingly, it is more likely seen in the higher rather than lower frequencies as in Ménière’s disease. The complaints of vertigo, hypoacusis, and tinnitus are vastly more common and, thus, the reason for patients seeking care from audiology and otolaryngology practitioners.
What Has Changed in Medical Management?
Most of our information on migraine and its effect on quality of life, intervention strategies, and treatment come from our neurology colleagues. New conditions have been described and older ones redefined. These more standardized descriptions of conditions have made treatment, research, and education much more consistent. In addition, neurologists have learned that many new risk factors can lead to migraine progression: medication overuse and rebound, obesity, snoring, sleep apnea, mTBI, physical or sexual abuse, hypothyroidism, anemia, anxiety, and depression.
The earliest migraine medications, primarily triptans, revolutionized treatment, but these drugs mostly evolved from drugs used to control blood pressure, seizures, and depression. By 2018, the introduction for the first calcitonin gene-related peptide inhibitors (CGRP)—monoclonal antibodies that block a pathway involved in the migraine process—was a major advance in preventative therapy. Another breakthrough has been Lasmiditan, which targets a serotonin receptor in a new class of migraine drugs
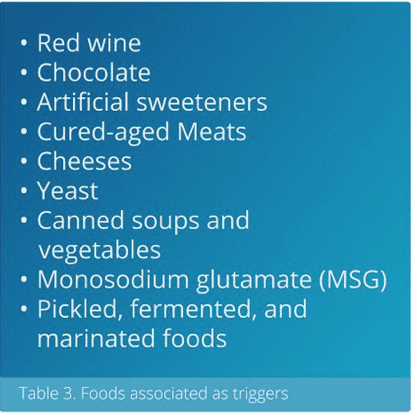
referred to as “ditans.” This has allowed migraine patients with a chronic condition to have far less disruption in their daily lives. In addition, more physicians have embraced alternative treatments in conjunction with these new drugs. The recommendation of Vitamin B12, magnesium, and coenzyme Q10 (CoQ10) are gaining popularity, along with the use of mindfulness and stress reduction activities, as often recommended for tinnitus patients. The Roberts et al study in 2021 reported that lifestyle modifications including restful sleep, consistent mealtimes, exercise, and avoidance of food triggers, had a significant positive impact on subjects with definite vestibular migraine.7 A list of common food triggers is shown in Table 3.
Role of Audiology and Otolaryngology
Once an individual is identified as a likely migraine or vestibular migraine patient (VM) during a case history, it is important to have them undergo a comprehensive neurodiagnostic audiovestibular assessment. Migraine patients have a much higher incidence of Benign Paroxysmal Positional Vertigo (BPPV) and Ménière’s disease as a comorbidity, as well as underlying unilateral vestibular dysfunction as identified by any one of several findings on a rotary chair, vestibular evoked myogenic potential (VEMP), Video Head Impulse Test (vHIT), and videonystagmography (VNG) caloric. Estimates show that as many as 50% of individuals may show caloric weakness in one ear. Most importantly, is identification of the vestibular dysfunction resulting from the migraine occurrences so that the patient is triaged accordingly for any appropriate non-medical intervention. This may include canalith repositioning maneuvers (CRM) for BPPV or vestibular rehabilitation therapy (VRT) for an unresolved or prolonged peripheral vestibular dysfunction with classic symptoms of exacerbation with head movement and visual stimulation.
The forthcoming second article in the series will review the tests within the neurodiagnostic audiovestibular battery and what results are typically associated with migraine. This will include an in-depth look at many of the newer technologies such as cervical and ocular VEMP and vHIT which were not available in decades past. Case studies to be provided will include infants as young as 10 months of age with BPV and older post-menopausal individuals with a variety of peripheral and central findings.
Summary
Practitioners can provide the patient with an important first step toward management by identifying the audiovestibular symptoms of the migraine patient. Oftentimes, migraineurs may not themselves associate their symptoms with migraine. Appropriate referral to a physician or collaboration with the referring physician will be an integral part of the continuum of care for this patient. Although neurologists typically are the lead practitioners in the management of the migraine patient, it is possible for interested otolaryngologists, primary care, and internal medicine physicians to also play a role in the management of their migraine patients. The evaluation of children and adults experiencing auditory-vestibular symptoms from migraine allows the audiologist to play a greater role in the continuum of patient care outside of traditional hearing testing and amplification.
Citation for this article: Gans RE, Sakumura J. Part 1. Audiovestibular symptoms related to migraine – What audiologists and ENTs need to know In 2022 for expanding patient care. Hearing Review. 2022;29(3):24-28.
References
- Gans RE. Classification of audiovestibular symptoms related to migraine, Part 1: Overview of migraine. Hearing Review. 2002.
- Schulz KA, Esmati E, Godley FA, et al. Patterns of migraine disease in otolaryngology: A CHEER network study. Otolaryngology-Head and Neck Surgery. 2018;159(1):42-50.
- Olesen J. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24(S1):9-10.
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1-211.
- Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2010 (GBD 2010) Results by Cause 1990-2010. (2010). https://ghdx.healthdata.org/record/ihme-data/gbd-2010-results-cause-1990-2010. Published 2022.
- Steiner TJ, Stovner LJ, Vos T. GBD 2015: Migraine is the third cause of disability in under 50s. J Headache Pain. 2016;17(104).
- Roberts RA, Watford KE, Picou EM, Hatton K, Trone TH, Brignola EY. Effects of lifestyle modification on vestibular migraine. Otology & Neurotology. 2021;42(10):e1537-e1543.