Overcoming one of the most debilitating obstacles to hearing help
There are a number of health conditions that are stigmatized. For many of these health conditions, including hearing loss, there are treatment programs that have been shown to be successful in overcoming self-stigma. Generally, the treatment is provided in the form of group intervention programs that provide: informational counseling on the targeted health condition and the deleterious effects of stigma and self-stigma; components of cognitive-behavior therapy; and empowerment and self-efficacy.
In 2010-2011, the Ida Institute (www.idainstitute.com) and its faculty—which included Leslie Jones, PhD, Patricia McCarthy, PhD, Christopher Lind, PhD, and Jean-Pierre Gagné, PhD—organized a series of seminars on the theme Living Well with Hearing Loss. This venue provided the faculty members with an opportunity to reflect on the meaning of “living well with hearing loss.” Because of their academic and research interests, it was obvious to the authors of the present article that, for many individuals, a major obstacle to “living well with hearing loss” is the social and self-stigma associated with hearing loss.
In order to live well with hearing loss, one must recognize and accept hearing loss. Specifically, many people must overcome the misplaced shame and poor self-esteem that they may experience. Only then is it possible to seek solutions to the difficulties attributable to their hearing loss experienced in everyday activities. Once this is achieved (if ever), they can extend their audiologic rehabilitation (AR) goals to activities that they identify as components of living well.
In this article, we briefly describe the social phenomenon of stigma and self-stigma. Then we describe the manifestation of self-stigma and how it constitutes a major impediment to seeking rehabilitation services, including the use of hearing aids. Finally, we broach the subject of treatment programs in hearing health care, as well as in other health conditions, which have been applied successfully to overcome the effect of self-stigma.
Defining Stigma and Self-stigma
Stigma has been defined as “the possession of, or belief that one possesses, some attribute or characteristic that conveys a social identity that is devalued in a particular social context.”1 In most western societies, there is a stigma associated with hearing loss. The general population perceives individuals with hearing loss as being “old,” “cognitively diminished,” “poor communication partners,” and generally “uninteresting.”2-7 Kochkin8 noted that hearing loss is often misunderstood as an intellectual challenge or a deficiency in personality and character.
Stigmatization is a social construct that can be studied from the vantage point of outsiders—people who do not possess the stigmatizing trait. Studies that have investigated the “hearing aid effect” are examples of research on the perceptions of outsiders concerning the stigma associated with hearing loss.3,9-13 As noted above, studies have shown that outsiders consider people with hearing loss to be old, senile, and socially unfit. In addition to possessing negative attitudes about individuals with stigmatizing conditions, outsiders often avoid and/or ostracize individuals with stigmatizing conditions.
Stigma can also be studied from the vantage point of insiders—people who possess a stigmatizing trait. Usually, insiders are aware of the prejudicial views held by the outsiders. Some insiders display self-stigma; they hold (consciously or not) the same prejudicial views about their stigmatizing condition as do the outsiders.
Self-stigma invariably involves a threat to one’s own identity. Often, people who experience self-stigma display a high level of stress, shame, and lower self-esteem and self-efficacy. In one of the ethnographic videos developed by Ida Institute anthropologists, Bill, an adult with an acquired hearing loss, described his perception of hearing loss saying, “[Being diagnosed with hearing loss] was the same as being told that I would have to wear adult diapers.”14 A detailed account of the phenomenon and manifestations of self-stigma is beyond the scope of this article. For a comprehensive look at social stigma and self-stigma associated with hearing loss, see Gagné et al.15
People who experience self-stigma are likely to develop maladaptive behaviors. For example, people with self-stigma will deny that they have a hearing loss. In most instances, the stigmatizing trait can be concealed (or the person with hearing loss believes that it can be concealed). Hétu16 reported that denial leads to statements such as, “I don’t have a hearing loss. It’s Jane that mumbles when she talks!” Ultimately, when people can no longer deny their hearing loss (eg, when they have had their hearing sensitivity tested), individuals displaying self-stigma may minimize their hearing loss. They may report: “My hearing isn’t that bad,” or “I have some difficulties, but I am not deaf!”

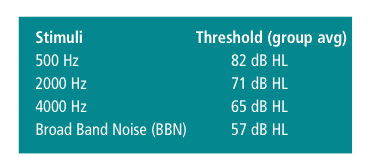
The manifestations of self-stigma were nicely captured by Kochkin.7,8 According to his investigations, 40% of adults with hearing loss who do not use hearing aids name stigma as one of the top 5 reasons for their non-purchasing decision (Table 1). Self-stigma is an important obstacle to AR. In other health conditions where stigma is concealable (eg, mental health disorders), it has been documented that, in order not to be identified as someone with a stigmatizing trait, people who display self-stigma choose not to seek treatment or they fail to comply with treatment regimens that are proposed.17-19
It is easy to imagine a similar scenario among individuals with hearing loss. Because they choose to conceal hearing difficulties from others, people with hearing loss who experience self-stigma will not purchase or wear hearing aids, and will not use assertive communication strategies that would require them to disclose their hearing loss to their communication partners. To avoid situations of identity threat due to their hearing loss, many stigmatized people employ (mal)adaptive coping strategies, such as avoiding social interactions in which communication breakdowns may occur.20-27
These strategies may make it possible to conceal the stigmatizing trait from others and thereby reduce the likeliood of experiencing an identity threat. However, these strategies also lead to withdrawing from social activities. Social isolation may lead to depression and have a negative impact on one’s general health.28
Rehabilitation Services to Overcome Self-stigma
Some rehabilitation programs have successfully addressed the self-stigma associated with a specific health condition. In the field of mental health, a combination of therapeutic approaches has been used to address self-stigma. These programs typically include:
- Informational counseling on the targeted health condition and the deleterious effects of stigma and self-stigma;
- Components of cognitive-behavior therapy;
- Empowerment and self-efficacy training in the form of interactions with people who have the same health condition, notably those who have successfully overcome self-stigma.29-34
Almost all treatment programs that address self-stigma issues are provided in a group intervention format. Bally states, “The objective of groups is to promote psychological and social growth and to ameliorate psychosocial problems through exploration of the cognitive, behavioral and affective interactions among members and within micro- and mesosocial contexts” (page 284).35 In his view, by definition, mutual support groups focus on providing psychosocial support.
Two-step AR program. Specifically related to acquired hearing loss, Hétu16 described a two-step normalization process for helping the person with hearing loss overcome feelings of shame and guilt associated with hearing impairment, and regain a more favorable social identity. The first stage of the normalization process involves meeting and interacting with other people who have a hearing loss, so that together the group members can share their experiences of hearing difficulties and unsatisfactory social interactions. This therapeutic activity helps the participants realize that unsatisfactory social interactions are the result of the hearing loss, and not the result of other factors that may have been unjustifiably attributed to them (eg, being unwilling to communicate). Moreover, group members realize that it is not unusual for people with hearing loss to feel denigrated, diminished, or ashamed of themselves. They come to realize that other people with hearing loss have the same feelings of ineptitude and self-denigration.
These realizations serve to trigger the normalization process. Specifically, group members come to the realization that they are not the only ones to have experienced shame and to have negative feelings about their hearing problems. They realize that other people experience the same feelings and that these feelings are “normal.” As a result of this process, they start to have a more positive attitude about themselves. The process of restoring a more positive social identity is initiated, and they are more willing to engage in social activities and interactions. In their group AR program (ie, in the presence of others who have hearing loss), they are likely to learn appropriate coping strategies and experience success in using these strategies when they interact in that favorable social environment.
In the second stage of the normalization process, people with hearing loss are encouraged to interact with people in their entourage who do not have a hearing loss. Moreover, they are encouraged and learn how to inform their communication partners that they have a hearing loss, and to solicit the use of communication strategies that will optimize the exchange of information. Under these circumstances, communication partners are more likely to acquiesce to the requests of the persons with hearing loss. It is likely that communication will become more efficacious and more satisfying for the person with hearing loss and their communication partners.
The result of participating in more satisfying conversations (social interactions) serves to further restore a more favorable social identity for the person with hearing loss. As the process of restoration continues, the individual gains confidence in the ability to be a satisfying communication partner. As a consequence, they are more likely to participate in valued activities that include people who do not have a hearing impairment and will likely develop a more positive image of themselves.
Supporting evidence. Hétu and Getty36-37 demonstrated that the group rehabilitation program that they provided to men with acquired sensorineural hearing loss due to noise exposure (and their spouses) was efficacious in overcoming self-stigma. After completing the program, participants were more likely to use hearing aids and assistive devices. They were also more likely to inform others of their hearing loss and to request communication strategies that involved the active participation of their communication partners.
Hogan38 termed Hétu’s stigma treatment program the “Montreal Hearing Help Program” (MHHP). Furthermore, he adapted and expanded the treatment program described by Getty and Hétu.36 Examples of activities that can be conducted within the group intervention therapeutic approach are provided in his book, Hearing Rehabilitation for Deafened Adults—A Psycho-social Approach (Whurr/Wiley).38
Hogan and his colleagues39 demonstrated experimentally that the therapeutic approach he proposed was successful in overcoming the effect of self-stigma. Specifically, the investigators reported improved self-confidence, less family conflict with regard to telephone calls and the volume of the television, as well as improved marital relations. Also, the participants with hearing loss reported that they were better understood, more able to pursue promotion at work, as well as more able to manage their stress. Partners of participants (63%) reported that the people with hearing loss took more responsibility for their communication needs and confirmed that family relations and communication had improved.
Later, using a similar intervention approach, Heydebrand and colleagues40 reported that, as a result of the group intervention, participants reported improved assertiveness, emotional well-being, and coping behaviors. Several other authors have reported that group intervention programs may serve to overcome the negative psychosocial aspects of hearing loss.41-43
Conclusion
It is well known that there is a stigma associated with hearing loss. Investigators have shown that people with hearing loss may experience self-stigma. That is, notwithstanding the fact that they have a hearing impairment, these individuals may hold prejudicial views and negative stereotypes toward people with hearing loss.
Having a negative perception toward oneself due to a stigmatizing trait leads people to be ashamed of themselves, and to have low self-esteem and low self-efficacy. Because hearing loss is invisible, people who display self-stigma often deny (or minimize) their impairment. Moreover, because they do not want to be identified as someone with a stigmatizing trait, they are likely to avoid or reject treatment programs (including the use of hearing aids) that may help overcome activity limitations and participation restrictions they experience. Similarly, they will not seek help for the stress they experience and the additional resources they expend by concealing their hearing loss from others. Also, they will not seek help to overcome the negative psychosocial manifestations that are attributable to their hearing loss.
ADDITIONAL ONLINE RESOURCES:

Aural Rehabilitation: Some Personal & Professional Reflections, by Mark Ross, PhD, with an introduction by Geoff Plant, PhD. September 2001 HR.
What Your Patients May Not Tell You, by Michael A. Harvey, PhD, ABPP. March 2010 HR.
HR Interviews…Sergei Kochkin, PhD, by Karl E. Strom. October 2005 HR.
There are a number of health conditions that are stigmatized. For many of these health conditions, including hearing loss, there are treatment programs that have been shown to be successful in overcoming self-stigma. Generally, the treatment is provided in the form of group intervention programs that provide: informational counseling on the targeted health condition and the deleterious effects of stigma and self-stigma; components of cognitive-behavior therapy; and empowerment and self-efficacy. There is evidence that this type of intervention program is successful when it is applied to people who experience self-stigma due to hearing loss.
Hearing health care professionals should be aware of the rehabilitative needs (including the psychological and psychosocial impact of hearing loss) of their clients, and they should provide this form of AR services. It has been shown that counseling (individually or in groups) improves the psychosocial disposition of clients and makes it more likely that they will use hearing aids and hearing assistive technologies, as well as use communication strategies that require them to inform the communication partner of their hearing loss.44-46
Correspondence can be addressed to HR or Jean-Pierre Gagné at .
References
- Crocker J, Major B, Steele C. Social stigma. In: Gilbert DT, Fiske ST, Lindzey G, eds. The Handbook of Social Psychology. Vol 2. 4th ed. New York: McGraw-Hill; 1998:504-553.
- Blood IM. The hearing aid effect: challenges for counseling. J Rehab. 1997;63(4):59-62.
- Doggett S, Stein RL, Gans D. Hearing aid effect in older females. J Am Acad Audiol. 1998;9(5):361-366.
- Erler SF, Garstecki DC. Hearing loss- and hearing aid-related stigma: perceptions of women with age-normal hearing. Am J Audiol. 2002;11(2):83-91.
- Franks JR, Beckmann NJ. Rejection of hearing aids: attitudes of a geriatric sample. Ear Hear. 1985;6(3):161-166.
- Kochkin S. MarkeTrak III: Why 20 million in US don’t use hearing aids for their hearing loss. Hear Jour. 1993;46(1):20-27.
- Kochkin S. Marke Trak VII: Obstacles to adult non-user adoption of hearing aids. Hear Jour. 2007;60(4):24-51.
- Kochkin S. MarkeTrak V: “Why my hearing aids are in the drawer”: the consumers’ perspective. Hear Jour. 2000;53(2):34.
- Blood GW, Blood IM, Danhauer JL. The hearing aid effect. Hearing Instruments. 1977;28(6):12.
- Blood I. The hearing aid effect: challenges for counseling. J Rehab. 1997;63(4):59-62.
- Gagné J-P, Stelmacovich P, Yovetich W. Reactions to requests for clarification used by hearing-impaired individuals. Volta Review. 1991;93(3):129-143.
- Johnson CE, Danhauer JL, Gavin RB, Karns SR, Reith AC, Lopez IP. The “hearing aid effect” 2005: a rigorous test of the visibility of new hearing aid styles. Am J Audiol. 2005;14(2):169-175.
- Ryan B-J, Johnson A, Strange A, Yonovitz A. The ‘Hearing Aid Effect’ in Northern Territory Indigenous Australian children as perceived by their peers. Aust N Z J Audiol. 2006;28(2):55-74.
- Ida Institute. Tool Room Videos. Naerum, Denmark: Ida Institute. Available at: idainstitute.com/tool_room. Accessed Jun 20, 2011.
- Gagné J-P, Southall K, Jennings MB. The psychological effects of social stigma: applications to people with acquired hearing loss. In: Montano J, Spitzer JB, eds. Advanced Practice in Adult Audiologic Rehabilitation: International Perspective. New York, NY: Plural Publishing; 2009:63-92.
- Hétu R. The stigma attached to hearing impairment. Scand Audiol Suppl. 1996;43:12-24.
- Barney LJ, Griffiths KM, Jorm AF, Christensen H. Stigma about depression and its impact on help-seeking intentions. Aust N Z J Psychiatry. 2006;40(1):51-54.
- Komiti A, Judd F, Jackson H. The influence of stigma and attitudes on seeking help from a GP for mental health problems: a rural context. Soc Psychiatry Psychiatr Epidemiol. 2006;41(9):738-745.
- Vogel DL, Wade NG, Hackler AH. Perceived public stigma and the willingness to seek counseling: the mediating roles of self-stigma and attitudes toward counseling. J Counseling Psychol. 2007;54(1):40-50.
- Hétu R, Getty L, Waridel S. Attitudes towards co-workers affected by occupational hearing loss. II: Focus groups interviews. Brit J Audiol. 1994;28(6):313-325.
- Hallberg L, Carlsson SG. A qualitative study of situations turning a hearing disability into a handicap. Disabil Handicap Soc. 1993;8(1):71-86.
- Hallberg LR, Barrenas ML. Coping with noise-induced hearing loss: experiences from the perspective of middle-aged male victims. Brit J Audiol. 1995;29(4):219-230.
- Major B, Schmader T. Coping with stigma through psychological disengagement. In: Swim JK, Stangor C, eds. Prejudice: The Target’s Perspective. San Diego: Academic Press; 1998:219-241.
- Steele CM. A threat in the air: how stereotypes shape intellectual identity and performance. Am Psychol. 1997;52(6):613-629.
- Link BG, Struening EL, Neese-Todd S, Asmussen S, Phelan JC. Stigma as a barrier to recovery: the consequences of stigma for the self-esteem of people with mental illnesses. Psychiatr Serv. 2001;52(12):1621-1626.
- Ritsher JB, Phelan JC. Internalized stigma predicts erosion of morale among psychiatric outpatients. Psychiatry Res. 2004;129(3):257-265.
- Perlick DA, Rosenheck RA, Clarkin JF, et al. Stigma as a barrier to recovery: adverse effects of perceived stigma on social adaptation of persons diagnosed with bipolar affective disorder. Psychiatr Serv. 2001;52(12):1627-1632.
- Arlinger S. Negative consequences of uncorrected hearing loss—a review. Int J Audiol. 2003;42 Suppl 2:2S17-20.
- Birbeck G. Interventions to reduce epilepsy-associated stigma. Psychol Health Med (Special Issue: Perspectives on Health-Related Stigma). 2006;11(3):364-366.
- Heijnders M, Van Der Meij S. The fight against stigma: an overview of stigma-reduction strategies and interventions. Psychol Health Med (Special Issue: Perspectives on Health-Related Stigma). 2006;11(3):353-363.
- Link BG, Struening EL, Neese-Todd S, Asmussen S, Phelan JC. On describing and seeking to change the experience of stigma. Psychiatr Rehab Skills. 2002;6(2):201-231.
- Sartorius N. Lessons from a 10-year global programme against stigma and discrimination because of an illness. Psychol Health Med (Special Issue: Perspectives on Health-related Stigma). 2006;11(3):383-388.
- Scambler G, Heijnders M, van Brakel WH. Understanding and tackling health-related stigma. Psychol Health Med (Special Issue: Perspectives on Health-related Stigma). 2006;11(3):269-270.
- Weiss MG, Ramakrishna J, Somma D. Health-related stigma: rethinking concepts and interventions. Psychol Health Med (Special Issue: Perspectives on Health-related Stigma). 2006;11(3):277-287.
- Bally SJ. Group therapy and group dynamics in audiological rehabilitation in adult audiologic rehabilitation. In: Montano JJ, Spitzer JB, eds. Adult Audiologic Rehabilitation. San Diego: Plural Publishing; 2009:283-302.
- Getty L, Hétu R. Development of a rehabilitation program for people affected with occupational hearing loss. II. Results from group intervention with 48 workers and their spouses. Audiology. 1991;30(6):317-329.
- Hétu R, Getty L. Development of a rehabilitation program for people affected with occupational hearing loss. I. A new paradigm. Audiology. 1991;30(6):305-316.
- Hogan A. Hearing Rehabilitation for Deafened Adults—A Psycho-social Approach. London: Whurr/Wiley; 2001.
- Hogan A, Ewan C, Noble WG, Munnerley G. Coping with occupational hearing loss: The University of Montreal Acoustics Group Rehabilitation Programme: An evaluation study. Journal of Occupational Health & Safety—Australia and New Zealand. 1994;10(2):107-118.
- Heydebrand G, Mauze E, Tye-Murray N, Binzer S, Skinner M. The efficacy of a structured group therapy intervention in improving communication and coping skills for adult cochlear implant recipients. Int J Audiol. 2005;44:272-280.
- Abrahamson J. Teaching coping strategies: a client education approach to aural rehabilitation. J Acad Rehab Audiol. 1991;24:43-53.
- Kricos P, Lesner S. Audiologic Rehabilitation for the Elderly: A Practical Approach to Rehabilitation. Boston: Butterworth-Heinemann; 1995.
- Trychin S. Coping with hearing loss. Seminars in Hearing. 1997;18(2):77-86.
- Hickson L, Scarinci N. Older adults with acquired hearing impairment: applying the ICF in rehabilitation. Semin Speech Lang. 2007;28(4):283-290.
- Jennings MB. Clinical report: evaluating the efficacy of a group audiologic rehabilitation program for adults with hearing loss using a Goal Attainment Scaling approach. Can J Speech Lang Pathol Audiol. 2009;33(3):146-153.
- Sauders GH, Lewis MS, Forsline A. Expectations, pre-fitting counseling, and hearing aid outcome. J Am Acad Audiol. 2009;20:320-334.
Citation for this article:
Gagné J-P, Southall K, Jennings MB. Stigma and Self-stigma Associated with Acquired Hearing Loss in Adults Hearing Review. 2011;18(8):16-22.