Patient Management | Mythbusters
As reported in The Hearing Review online (November 6, 2015), Phonak has convened a select group of hearing healthcare experts to provide evidence-based recommendations to hearing care providers on how to better engage family members. Chaired by Dr Louise Hickson, the objective of this group is to facilitate family involvement throughout the hearing remediation process. The group proposes an audiologic treatment shift from a site-of-lesion focus to a family-centered care perspective as a means of increasing the value of our services and the uptake of hearing devices. This paper is the third in a series of several common (mis-)beliefs about the approach, which will be challenged by the authors. Click here to access Mythbusters #1 and Mythbusters #2.

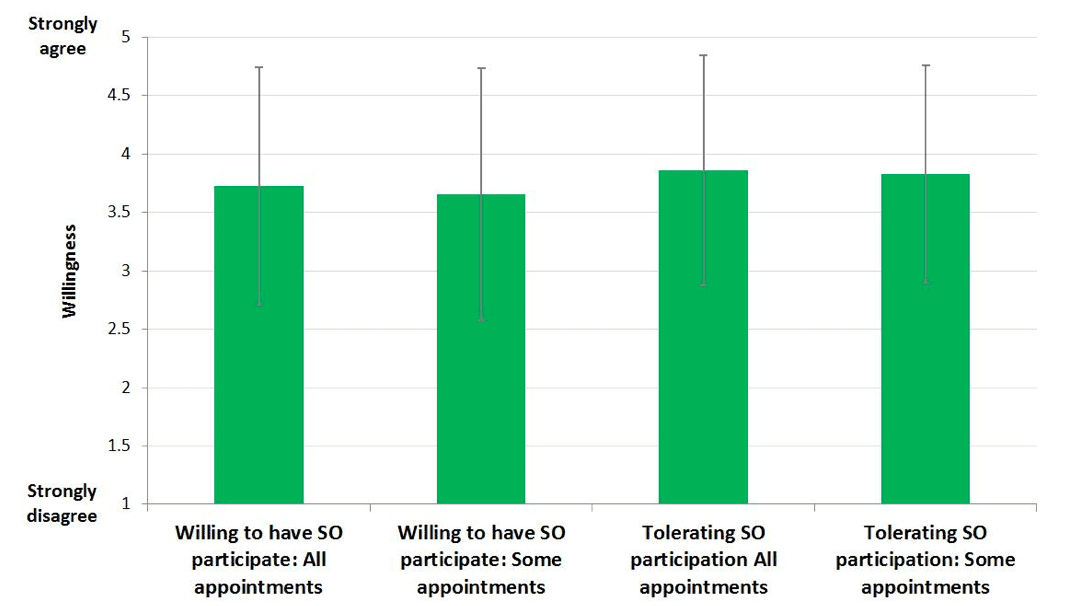
Figure 1. [Click on image to enlarge.] Mean (SD) of patients’ desired involvement of family in audiology appointments. SO = Significant Other.
- Be willing to have a significant other participate in ALL of my audiology appointments,
- Be willing to have a significant other participate in SOME of my audiology appointments,
- Tolerate a significant other participating in ALL of my audiology appointments (if required),
- Tolerate a significant other participating in SOME of my audiology appointments (if required).
Responses to the survey (Figure 1) were captured on a 5-point scale with the following response options (1 = “strongly disagree,” 2 = “disagree,” 3 = “neither agree nor disagree,” 4 = “agree,” and 5 = “strongly agree”). In contrast to the myth, we observed broad support for the claim that patients support the inclusion of their family in audiology appointments. Specifically we found that only 15.8% and 13.7% of the participants indicated low willingness (ie, a response of “1” or “2” to involve family in either all or some of their appointments, respectively). Furthermore, when we asked patients if they would tolerate family involvement in appointments, this number drops to 11.6% and 7.4%, respectively. Hence, in the vast majority of cases, patients report a clear preference for greater involvement family members during the audiologic care process.
Naturally, it will be the case that a small proportion of patients will not want family members involved in audiology appointments, and consistent with the principles of family-centered care, we espouse that clinicians should respect these wishes. However, given the improved outcomes observed for the patient, their family, the clinician, and business by including family members in clinical care4 and patients’ desire for the inclusion of family involvement in audiology care, it is time to dispel the myth that “many patients do not want their family in the room.”
The Challenge
Invite family members to come into the audiology appointment by greeting both the patient and the family in the waiting room (eg, “Good morning Mr and Mrs Smith—great to see you both”). Use positive and welcoming verbal and nonverbal signals. If either patient or family member is reluctant or unsure then don’t push it straight away. When you have the patient in the clinic room, explain why it would be useful to have a family member join in the appointment. If the patient agrees, then return to the waiting room and bring the family in. Remember, the evidence is that you will get better outcomes for the patient and the family if you do this!
References
1.Laplante-Lévesque A, Hickson L, Worrall L. Rehabilitation of older adults with hearing impairment: A critical review. J Aging Health. 2010.22(2)143-153.
2.Laplante-Lévesque A, Hickson L, Worrall L. Predictors of rehabilitation intervention decisions in adults with acquired hearing impairment. J Sp Lang Hear Res. 2011;54:1385-1399.
3.Poost-Faroosh L, Jennings MB, Cheesman MF. Comparisons of client and clinician views of the importance of factors in client-clinician interaction in hearing aid purchase decisions. J Am Acad Audiol. 2015;26(3):247-259.
4.Singh G, Hickson L, English K, et al. Family-Centered Adult Audiologic Care: A Phonak Position Statement. Hearing Review. 2016;23(4):16.
Louise Hickson, PhD, is Professor of Audiology, Head of the School of Health and Rehabilitative Sciences, and Director of the Communication Disability Centre at the University of Queensland in Australia. Gurgit Singh, PhD, is a Senior Research Audiologist at Phonak Canada, and an adjunct professor at Ryerson University and adjunct lecturer at the University of Toronto.
Correspondence can be addressed to Hearing Review or Dr Hickson at: [email protected]