What audiological tools can we use to provide individualized hearing solutions?
|
| Peggy B. Nelson, PhD, is an associate professor of audiology at the University of Minnesota in Minneapolis; Benjamin Hornsby, PhD, is an assistant professor at Vanderbilt Bill Wilkerson Center in Nashville, Tenn; Brian C. Moore, PhD, is professor of auditory perception at the University of Cambridge in England; and Timothy Trine, PhD, is chief technical officer at Starkey Laboratories, Eden Prairie, Minn. |
The next logical step in our research efforts to improve amplification outcomes seems to be the matching of performance measures specific types of cochlear damage, psychoacoustic ability, or cognitive processing.
In recent years, researchers have uncovered a great deal of information about the physiology of hearing loss of various etiologies. As a result, we have achieved a greater understanding of the cochlear and neural effects of ototoxic drugs,1 noise trauma,2 genetic mutations,3 and aging,4 among others. These physiologic studies demonstrate that, although individuals may have similar audiometric findings, the underlying damage to auditory structures may be considerably different.
In addition, we have a substantial body of information about functional effects of both inner and outer hair cell loss.5,6 When studying performance of listeners with hearing loss, research reports have long noted that there are significant individual speech recognition differences among listeners with sensorineural hearing loss (SNHL). Differences in audibility, even when aided, account for a substantial amount of variability. However, even when differences in audibility among individuals are taken into account, differences in aided speech understanding among listeners with SNHL, particularly in noise, remain.7 At the same time, individual differences in both psychoacoustic and cognitive processing abilities of persons with, and without, hearing loss have been observed for many years.7-9 Specific connections among these physiological and performance findings, however, have been limited.
The next logical step in our research efforts to improve amplification outcomes seems to be the matching of performance measures to specific types of cochlear damage, psychoacoustic ability, or cognitive processing. The following questions arose from our group discussions:
- Apart from audibility differences, to what extent do individual differences affect listeners’ success with amplification?
- If one could screen hearing aid users for their individual differences, would that change our amplification fitting protocol and improve listeners’ success? If so, how?
- Can we use our knowledge of individual performance differences to improve follow-up and rehabilitation services?
Although a thorough review of cochlear pathophysiology is beyond the scope of this article, certain recent findings are highlighted here. Mills and Schmiedt4 have noted that, in animal models of the aging cochlea, abnormal hair cell function seems to result from a reduction in stria vascularis function, resulting in flat SNHL with reduced compression throughout the cochlea. In other studies, cochlear stresses from agents such as noise trauma and toxicity have resulted in cell apoptosis, or programmed outer hair cell (OHC) death.10 Ototoxic drugs such as cis-platin seem to cause similar stress responses in the cochlea,1 while other drugs such as carboplatin may affect inner hair-cell (IHC) function.11 Genetic mutations have been identified as potentially responsible for a variety of disorders, including OHC motility, neuropathy, and many others. Despite this increased knowledge of hair cell function, death, and renewal, few functional and behavioral connections have been made between patterns of hair cell loss and listeners’ performance with amplification or in noise.
The extensive literature on speech recognition by listeners with hearing loss demonstrates clearly that intersubject variability is widespread. Early reports on the use of the articulation index (AI) to predict performance showed that, although the AI predicts average speech recognition performance by hearing-impaired listeners reasonably well, considerable intersubject variability is often found.12 Studebaker et al13 analyzed speech recognition test scores from 2,600 ears with hearing loss and measured the differences between predictions based on the AI (including the effects of the audiogram) and actual speech recognition scores. Analysis of these data showed a standard deviation of the distribution of differences of 13 rau (rationalized arcsine units that approximate percentage points14), suggesting considerable intersubject variability. That is, some hearing-impaired listeners performed much better than predicted from the AI, while others performed significantly worse. They noted that this variability was greater among listeners with hearing loss than among normal-hearing listeners.
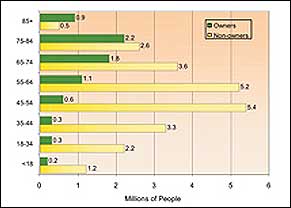
Results from tests of speech recognition in noise (steady and gated) suggest that the variability among listeners with hearing loss may be even greater when listeners are tested in noise than in quiet. Killion et al15 reported wide ranges of abilities among listeners with hearing loss. They reported that listeners with 40 dB to 60 dB pure-tone averages show signal-to-noise ratio (SNR) loss—the improvement in SNR needed to achieve a certain percentage speech recognition—ranging from 2 dB (near normal) to more than 20 dB.
Differences in audibility among listeners could only account for some of this wide variability. Jin and Nelson16 observed that listeners with SNHL showed near-normal performance in steady noise when the speech sounds were amplified to ensure full audibility. However, they noted a significant reduction and large variability in performance among listeners with hearing loss when the noise was interrupted. This reduction in masking release has been attributed to potential differences among listeners in their temporal17 or spectral16 resolution abilities, or in their ability to use temporal fine structure.18 Again, few connections have been established between masking-release performance and hearing aid satisfaction.
Other explanations have been proposed for differences in speech recognition across subjects, including cochlear dead regions (regions with no or very few functioning IHC), effects of aging, and overall cognitive and personality factors. Recent work by Vinay and Moore19 suggests that, when the hearing loss at a given frequency is 70 dB HL or greater, the probability of there being a dead region at that frequency is greater than 50%. Vickers et al20 and Baer et al21 used the threshold-equalizing noise (TEN) test22 and psychophysical tuning curves to diagnose dead regions in listeners with high-frequency hearing loss. They also explored the effect of low-pass filtering on the identification of amplified speech signals. They found that listeners without dead regions were able to make use of the high frequencies in the speech to improve identification, while the listeners with dead regions were not.
Rankovic23 questioned the interpretation of these results, suggesting that the individual results could be accounted for using the version of the AI described in the 1950s by Fletcher,24 which takes into account factors other than audibility. However, Moore25 argued that some aspects of the results could not be accounted for by the Fletcher AI. More recent work by Mackersie et al26 suggests that the benefit of high-frequency amplification for speech identification differs across listeners with and without dead regions (with matched audiograms) when noise is present, but not in quiet. For listeners with low-frequency hearing loss, the amplification of very low frequencies can have deleterious effects on speech intelligibility for listeners with low-frequency dead regions, but does not have such effects on listeners without dead regions.27
Several investigators have focused on the specific effects of aging on auditory function. In particular, elderly listeners seem to have greater difficulty with the representation of the temporal fine structure in signals than do younger listeners with hearing loss.28 A possible result of lack of representation of temporal fine structure is increased difficulty in exploiting temporal dips in fluctuating background sounds.18 Additional investigations of elderly listeners29 show that they demonstrate poorer use of temporal cues in rapid speech than younger listeners. Further investigation of the role of temporal processing in aging listeners seems important.

|
| Mead Killion, PhD, published a three-part series on what he considers hearing aid “myths”: Myths that discourage improvements in hearing aid designs, myths about hearing aid performance and customer satisfaction, and myths about hearing in noise. Access them in the HR 2004 Archives (January, February, and August editions). |
More general cognitive and personality factors may also be related to individual differences in hearing aid success. Cox et al30 suggested that personality types affect hearing aid satisfaction, with more extroverted patients reporting more hearing aid benefit than others. Nabelek and colleagues31 have found wide differences in judgments of acceptable noise levels (ANL), especially between hearing aid users and those who have chosen to be nonusers. The ANL (defined as the separation in dB between most-comfortable level and the highest tolerable noise level) seems to vary significantly among listeners, and may be useful for predicting hearing aid use. Saunders and Forsline32 compared listeners’ measured and perceived ability to understand speech and found that hearing aid dissatisfaction is related to both the listeners’ actual ability and their perception of their ability to hear. Their results suggest that some individual listeners significantly underestimate their ability to understand speech, and so may express significant dissatisfaction with amplification. Thus, it seems that some more global individual differences may also significantly affect success with amplification.
In summary, it is clear that considerable variability exists among listeners with hearing loss. In addition, a number of important questions about individual differences remain: Can we significantly improve hearing aid fittings by knowing more about each person’s abilities and by individualizing the first fit? Do we have evidence that reduced masking release results in reduced performance and satisfaction with hearing aids? Do alternative fitting strategies improve performance of listeners who have demonstrated signs of cochlear dead regions? Should algorithms or technology used to fit elderly people be different from those used with younger people with the same hearing loss? Additional information is needed to match amplification technology and rehabilitative strategies to individual users of hearing aids.
Summit Recommendations
As a result of our discussion and review of the literature, we see a great potential for future investigation and the need for more research into factors other than audibility and comfort that may contribute to hearing aid success, in particular to:
- Provide additional measures of the individual differences seen among listeners with hearing loss and the factors related to those differences.
- Investigate the value of additional speech recognition testing in complex background sounds, and to establish whether this can be used to predict listeners’ performance in daily situations. Additionally, research is needed on the connections between clinical tests of masking release and hearing aid satisfaction in daily life.
- Establish larger population studies of cochlear dead regions and their diagnosis. Determine amplification outcomes and the potential for more effective hearing aid fittings using results of the diagnostic tests.
- Investigate factors related to the aging population, their unique auditory abilities, amplification needs, and hearing aid success.
- Investigate further the extent to which cognitive, personality, and perceptual factors affect amplification outcomes.
- Focus on rehabilitation strategies and treatment planning to accommodate listeners’ individual characteristics. Individual difference assessment should lead to improved individual treatment plans and increased satisfaction.
References
- Rybak L, Whitworth C, Mukherjea D, Ramkumar V. Mechanisms of cisplatin-induced ototoxicity and prevention. Hear Res. 2006: Available via Science Direct at: 10.1016/j.heares.2006.09.015.
- Henderson D, Bielefeld E, Harris K, Hu B. The role of oxidative stress in noise-induced hearing loss. Ear Hear. 2006;27:1-19.
- Liu X, Pandya A, Angeli S, Telischi F, Arnos K, Nance W, Balkany T. Audiological features of GJB2 (Connexin 26) deafness. Ear Hear. 2005; 26:361-369.
- Mills D, Schmiedt R. Metabolic presbycusis: differential changes in auditory brainstem and otoacoustic emission responses with chronic furosemide application in the gerbil. J Assoc Res Otolaryngol. 2004;5:1-10.
- Moore BCJ. Dead regions in the cochlea: diagnosis, perceptual consequences, and implications for the fitting of hearing aids. Trends Amplif. 2001;3:1-34.
- Turner C. Hearing loss and the limits of amplification, Audiol Neurotol. 2006; 11 [Suppl 1]:2-5.
- Humes L. Factors underlying the speech-recognition performance of elderly hearing-aid wearers. J Acoust Soc Am. 2002; 112(3 Pt 1):1112-32.
- Johnson D, Watson C, Jensen J. Individual differences in auditory capabilities. J Acoust Soc Am. 1987;81(2):427-38.
- Divenyi P, Haupt K. Audiological correlates of speech understanding deficits in elderly listeners with mild-to-moderate hearing loss. Correlation analysis. Ear Hear. 1997;18(2):100-113.
- Matsui J, Cotanche D. Sensory hair cell death and regeneration: two halves of the same equation. Curr Opin Otolaryngol Head Neck Surg. 2004;12:418-425.
- Salvi R, Ding D, Wang J, Jiang H. A review of the effects of selective inner hair cell lesions on distortion product otoacoustic emissions, cochlear function and auditory evoked potentials. Noise Health. 2000;2:9-26.
- Rankovic C. An application of the articulation index to hearing aid fitting, J Speech Hear Res. 1991;34:391-402.
- Studebaker G, Gray G, Branch W. Prediction and statistical evaluation of speech recognition test scores. J Am Acad Audiol. 1999;10:355-370.
- Studebaker G. A “rationalized” arcsine transform. J Speech Hear Res. 1985;28:455-462.
- Killion M, Niquette P, Gudmunsen G, Revit L, Banerjee S. Development of a quick speech-in-noise test for measuring signal-to-noise ratio loss in normal-hearing and hearing-impaired listeners. J Acoust Soc Am. 2004;116:2395-2405.
- Jin S, Nelson P. Speech perception in gated noise: the effects of temporal resolution. J Acoust Soc Am. 2006;119:3097-3108.
- George E, Festen J, Houtgast T. Factors affecting masking release for speech in modulated noise for normal-hearing and hearing-impaired listeners, J Acoust Soc Am. 2006; 120:2295-2311.
- Lorenzi C, Gilbert G, Carn H, Garnier S, Moore BC. Speech perception problems of the hearing impaired reflect inability to use temporal fine structure. Proc Natl Acad Sci USA. 2006; 103:18866-18869.
- Vinay, Moore BCJ. Prevalence of dead regions in subjects with sensorineural hearing loss. Ear Hear. 2007;28:231-241.
- Vickers DA, Moore BCJ, Baer T. Effects of lowpass filtering on the intelligibility of speech in quiet for people with and without dead regions at high frequencies. J Acoust Soc Am. 2001; 110:1164-1175.
- Baer T, Moore BCJ, Kluk K. Effects of lowpass filtering on the intelligibility of speech in noise for people with and without dead regions at high frequencies. J Acoust Soc Am. 2002;112:1133-1144.
- Moore BCJ, Huss M, Vickers DA, Glasberg BR, Alcántara JI. A test for the diagnosis of dead regions in the cochlea. Br J Audiol. 2000;34:205-224.
- Rankovic C. Articulation index predictions for hearing-impaired listeners with and without cochlear dead regions. J Acoust Soc Am. 2002; 111:2545-2548.
- Fletcher H. Speech and Hearing in Communication. New York: Van Nostrand; 1953.
- Moore BCJ. Response to “Articulation index predictions for hearing-impaired listeners with and without cochlear dead regions.” Letters. J Acoust Soc Am. 2002;111:2545-2548, 2549-2550.
- Mackersie CL, Crocker TL, Davis RA. Limiting high-frequency hearing aid gain in listeners with and without suspected cochlear dead regions. J Am Acad Audiol. 2004;15: 498-507.
- Vinay, Moore BCJ. Identification of speech as a function of highpass filter cutoff frequency for people with and without low-frequency cochlear dead regions. J Acoust Soc Am. In press.
- Pichora-Fuller K, Singh, G. Effects of age on auditory and cognitive processing: implications for hearing aid fitting and audiologic rehabilitation. Trends Amplif. 2006;10: 29-59.
- Gordon-Salant S, Yeni-Komshian G, Fitzgibbons P, Barrett J. Age-related differences in identification and discrimination of temporal cues in speech segments. J Acoust Soc Am. 2006; 119:2455-2466.
- Cox R, Alexander G, Gray G. Personality and the subjective assessment of hearing aids. J Am Acad Audiol. 1999;10:1-13.
- Nabelek A, Tampas J, Burchfield S. Comparison of speech perception in background noise with acceptance of background noise in aided and unaided conditions. J Speech Lang Hear Res. 2004; 47:1001-1011.
- Saunders G, Forsline A. The performance-perceptual test (PPT) and its relationship to aided reported handicap and hearing aid satisfaction. Ear and Hear. 2006;27:229-242.
Correspondence can be addressed to HR or Peggy Nelson at .