We can do great things to ameliorate a patient’s hearing loss. But despite the technological marvels, patients should understand that the hearing they have lost will remain lost. Concomitantly, they should also be aware that, in most cases and in most environments, their residual auditory capacity will allow them to hear conversation quite well and remain a vibrant, functional part of their social world. The terms mild, moderate, or severe loss mean very little to anyone. Our counseling efforts need to focus on residual auditory capacity (the glass half full) and what can be done via amplification to maximize its use and its preservation.
It has always been difficult to describe an audiogram to a patient using the comparative terms of “mild,” “moderate,” “severe,” and “profound” hearing loss. These are all relative terms, as they “scale” our professional assessments of what most people would call “deafness.” No one can actually simulate total deafness, in terms of what it actually portends for the lifestyle of an individual who is deaf, so why should we be using these relative terms when describing a patient’s audiogram?
Most patients are in the first stage of the six stages involved in “loss” when they first have their audiogram explained to them. This first stage is the “denial” stage. It is during this stage, in particular, patients commonly translate the terms “mild” and “moderate” as “not that bad,” and they continue choosing to cope and/or suffer with the disability, rather than to progress to the other stages of loss—toward “acceptance” and “doing something about it.” It’s incumbent on the dispensing professional to tell them that action on their part can help forestall a further decrease in their hearing capabilities and even forgo a possible withdrawal from social activities due to a hearing problem.
As hearing care professionals, we need to present our patients with a more accurate portrayal of their auditory condition. After all, electroacoustic stimulation via hearing instruments simply does not “correct” the hearing loss; it only stimulates the remaining (residual) capacity of their damaged auditory system. Even though we have an array of means in which to help them hear better, the hearing “loss” is permanently lost! Not only is the intensity-at-frequency information gone, but so too is information about temporal sequencing, transitions from vowels to consonants, prosody, and the “fullness” of speech (or music). If you are hesitant to accept this fact, ask yourself if you would rather listen to a concert by the philharmonic or on a calliope.
Dynamic Range and the “Fence” for Counseling
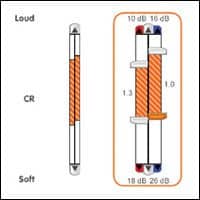
When threshold results are described to patients, we should present the results as their “fence” between damaged hearing and their remaining hearing ability. We traditionally call that fence “threshold,” and we have generations of experience trying to modify this threshold. Over the decades, we have finally learned that ameliorating hearing loss is not about simply “moving the fence.” Instead, making maximum use of a patient’s residual hearing requires that we optimize the capabilities between “threshold” (below which they can’t hear the sound) and UCLs at frequencies (above which they can’t endure the sound). This area of variable shape—beginning at 250 Hz and going out to 6000Hz—defines the range of the residual auditory areal capacity.
One effective counseling method involves getting the patient, who has already indicated their thresholds at these frequencies, to also give us tonal indicators of MCL and UCL at each frequency. These points are then plotted on the audiogram form or on a plain graph which will represent dB SPL (if the measured numbers are corrected for each frequency). It is explained that hearing instruments are made with these specifications in mind and their performance is measured in dB SPL.
Draw a “normal” undamaged dynamic range “hearing ability” box onto an audiogram. Mark horizontal lines at 0 dB and 100 dB HL, and attach the horizontal lines with vertical lines at 200 Hz and 6000 Hz. Now, plot the patient’s thresholds within this box. “Shadow” or “X” out the area of the box where no hearing ability could be measured. The non-shadowed area within the box represents the patient’s residual hearing ability (ie, the hearing that the patient has left and can utilize). The shadowed area is the permanent hearing loss. It needs to be understood that this area is gone forever, and cannot be “restored.”
This information can be presented as a “bad news” vs “good news” type of scenario. The bad news is the hearing damage; the good news is the amount of residual auditory ability still available to the patient. In the majority of cases—including most steeply sloping hearing losses—the patient’s auditory capacity in the 1500-2500 Hz area is usually significant enough for him/her to gain access to the most important speech elements, such as voicing and suprasegmentals, F2 vowels and transitions, F3 vowels, fricative bursts, etc. This, in fact, is very good news!
Digital and advanced programmable technology allows us to “fill” the measured residual auditory area in a more precise manner. We also need to protect that upper limit of hearing with appropriate compression. To prevent accidental “harm” to the patient’s residual hearing, we can now test for and adjust digital aids in 1 dB (as opposed to 5 dB) increments.
However, it is the filling of the residual auditory area that creates the perception of that much desired “fullness” of sound. Success in optimizing whatever “fullness” that is achievable in any given fitting relies on both the skill of the dispensing professional and the commitment of the patient in describing the pros/cons of the fitting—as well as the patient’s commitment to acclimate to a new world of sound that squeezes the appropriate (and, to some extent, subjective) amount of auditory information within that reduced residual hearing range.
Moving the patient across the “fence” results in the patient taking ownership and becoming more proactive in taking care of their residual hearing ability. It creates at once an awareness of their powerful ability (in most cases) to understand speech and conversation, their limitations in receiving all of the various frequency/intensity information that exists in all the different listening environments, and the need to conserve whatever residual hearing they have left so their hearing loss is less likely to get worse. This allows the patient to move over to the functioning side of the fence, and they will be more willing to listen to your suggestions for appropriate methods for each ear’s care.
Summary
Post-fitting performance-based measures should be discussed relative to the patient’s residual hearing ability—not their hearing loss or what can be, at times, a ridiculous (and self-defeating) comparison to a normal-hearing person’s abilities. Our goal for individuals who have hearing impairment is a more normal hearing ability. Realistic expectations based on the patient’s measured residual auditory ability should be the basis for counseling and the auditory rehabilitation for that patient. In this context, our terms “mild,” “moderate,” and “severe” mean very little to anyone—even to hearing care professionals!


|