Practice Management | April 2021 Hearing Review
Although disruption brings anxiety about the future, tremendous opportunities are emerging
Even before the worldwide pandemic, inevitable developments in our field were approaching, presenting both threats and opportunities. This article identifies six of the major developments and highlights the opportunities that could be nurtured for both patients and audiology practices.
By David DeBonis, MS, PhD
Partly due to the worldwide pandemic, and partly due to inevitable developments that preceded it, the hearing care landscape has changed and many audiologists appear to believe these changes could threaten the viability of the profession. Survey data of 2,172 audiologists indicated that 90% expressed moderate to great concern regarding their professional future.1 Although there are clear reasons for concern, this article highlights just six areas of opportunities—for both patients and audiology practices—that can be nurtured in this new landscape.
1) Greater Awareness of Hearing Healthcare as a Public Health Issue
More than ever, hearing loss is being viewed as a public health issue. Hearing loss impacts greater numbers of people than those who have heart disease, diabetes, and mental illness,2 and its potential negative physical, psychological, and cognitive impacts have been well documented. Researchers have found that even those with mild hearing loss demonstrate signs of cortical reorganization that could be related to increased risk of mental health challenges3 and others describe associations between hearing loss and increased falls, hospitalization, and even institutionalization.4 Some have noted that health authorities warn that hearing loss is the single factor that accounts for the largest proportion of risk for dementia occurring in middle-to-later life.5 The National Institutes of Health are currently funding a randomized control study of older adults to assess whether use of hearing aids can reduce the risk of cognitive decline. Findings are expected in 2022.
Opportunity: The argument in support of hearing loss as an issue of public health is backed by evidence, and this evidence continues to underpin actionable initiatives.6,7 With the necessary support of professional hearing-related groups and individual audiologists, this information can eventually demonstrate that hearing loss in the adult population is a chronic medical condition that must receive greater urgency in the traditional medical model of care. The results would be greater numbers of individuals receiving audiological services through referrals from primary healthcare providers and improved insurance coverage.
2) Availability of Screenings
This greater recognition of the negative impact of hearing loss, along with improvements in technology, has led to new screening options. Research assessing the potential benefits of a 10-minute telephone hearing screening involving digits embedded in noise taken by 30,981 individuals revealed sensitivity values of .81 and specificity of .65.8 Good validity, sensitivity, and specificity have also been noted using available screening apps with appropriate transducers.9 Finally, associations between hearing loss and mental health have led for some to call for universal cognitive screenings of all individuals age 70 years or older who have hearing loss and/or listening difficulties.10
Opportunity: Convenient, cost-effective screenings could lead to increased interest in diagnostic hearing testing and greater opportunities for hearing care professionals to discuss the value of amplification. Including time-efficient cognitive screenings in hearing care practices could add a valuable service for patients, provide relevant diagnostic data for those patients who have unexplained listening difficulties, and help to broaden the role of the audiologist as a healthcare provider.
3) OTC Hearing Aids
The changing hearing care landscape is, without question, related to concerns about affordability and accessibility of hearing aids. Because up to 80-90% of the income of many dispensing audiologists may come from hearing aid sales,11 legislation allowing for the production and sale of over-the-counter (OTC) hearing aids has created anxiety among HCPs.
Opportunity: In addition to the potential benefit to those patients who can obtain amplification that they would otherwise not be able to afford, audiologists may also benefit from this development. Although some research has suggested that an OTC delivery model is feasible,12 other research raised concerns about patients’ abilities to make decisions about their candidacy and selection of device features.13 The same research found that the overwhelming majority of participants believed that assistance with these decisions would be helpful.
These data suggest that there will be a need for audiologists to integrate services related to OTC hearing aids into their practices. Regarding concerns of the loss of income, audiologists with experience in private practice hearing aid dispensing have suggested that we should consider joining together into one buying group to reduce the cost to purchase hearing aids and use the revenue to offer competitive prices, manage the buying group, better inform the public of our role, and push for changes in legislation that expand hearing healthcare.11
4) Greater Attention to Addressing the Public’s Awareness of Audiology
Some have noted that the real threat to audiologists is not new competition or creation of a new category of hearing device, but rather that the audiology brand has not been sufficiently established in the mind of the public.14 Others have compared the public’s strong recognition of the role of optometrists and ophthalmologists in vision care with the comparatively weak association held between audiologists and hearing care.15
Opportunity: Anxiety among audiologists regarding our own viability may motivate the profession to address this issue. Experts in the field have called for outreach to allied health professionals who serve people at risk for hearing loss, including optometrists, physical and occupational therapists, home care providers, and diabetes educators, with a focus on audiologists’ broad expertise, rather than just hearing aids.14,15 In addition, audiologists should support their professional organizations through increased participation in activities such as World Hearing Day on March 3 and Better Hearing and Speech Month in May, among other opportunities.
5) Telepractice
Even prior to the worldwide pandemic, interest in telepractice among audiologists was growing. International survey data revealed that 15.5% of 269 audiologists reported having experience with teleaudiology16 and ASHA survey data suggested that large majorities of audiologists want more information regarding telepractice.17 As described by a major health institute, .the pandemic has resulted in a “rapid and unprecedented change in healthcare delivery” with telepractice now established as “an increasingly important method of care delivery with potential to significantly impact patient, payers, and providers.”18 Both the value and reliability of telepractice across a variety of audiological services has been established.19-23 Regarding hearing aid follow-up services done remotely, research suggesting that large majorities of participants are able to install the necessary software quickly, with no technology problems, and more than 90% indicated that they would recommend this service.24
Opportunity: The well-documented imbalance between the number of people who need audiological services and the number who receive them,25,26 exacerbated by the clinic-based model that requires patients to travel to the audiologist for care, can be addressed through telepractice and expand the practitioner client base to those who have barriers to service access. Telepractice can also create more time for the audiologist to address neglected aspects of care, such as counseling and hearing aid orientation.27 Finally, due to the current widespread need to use remote service technologies, greater attention is being paid to the issues of reimbursement and will very likely lead to increased coverage for telepractice.
6) Greater Awareness of Listening Difficulties
Audiologists regularly see patients who report considerable listening and hearing difficulties, particularly in noise, whose pure-tone thresholds fall within the “normal range.” Traditionally, many audiologists have viewed these individuals as unimpaired and, therefore, not requiring intervention. This is now changing.
Several possible causes for this “hidden hearing loss” have recently been summarized in the literature.28,29 One such cause, synaptopathy, a condition involving a reduction in the synapses that carry information from the inner hair cells (IHCs) to auditory neurons,30 has been demonstrated in animal studies but is not yet established in humans.31 Other possible causes include undiagnosed extended high-frequency hearing loss,32,33 auditory processing disorders,34 speech-in-noise disorder,35 auditory neuropathy spectrum disorders,36 and impairments in memory or attention.29,37
Opportunity: Addressing listening issues could provide needed support to patients who have been neglected and could open up opportunities for audiologists to serve a new base of clients, estimated to be over 20 million people in the United States alone.28 It also could establish audiologists as the professionals who provide services to those with listening difficulty (see Table 1).
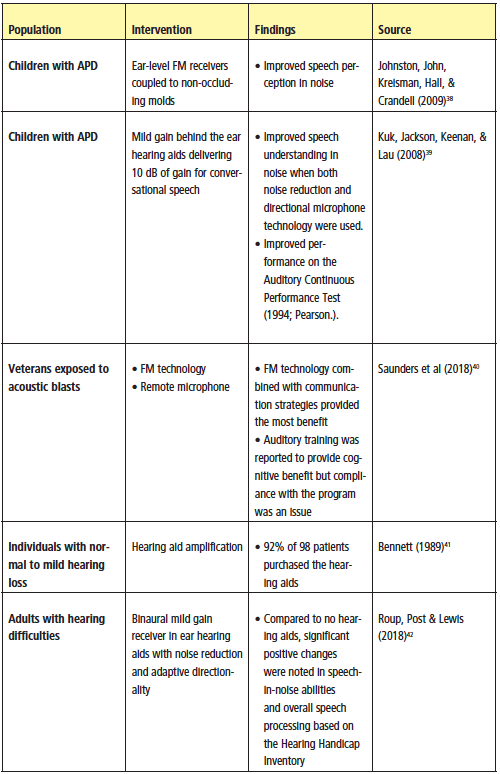
Table 1. Summary drawn from the work of Beck et al (2018)28 of select studies that have been performed assessing interventions for those with hearing difficulties in the absence of pure-tone hearing loss.
Audiology Self-Study: Assessing Readiness for a New Audiology Landscape
The need to embrace the new audiology landscape and carefully consider what adjustments need to be made in our practices existed before COVID, but certainly has been accelerated by it. The very changes that could be threatening to audiologists, could also create new opportunities to review our current procedures, revise them, as needed, and creatively plan for what is ahead. To assist in this process, Table 2 provides an example of a self-study form based specifically on the themes identified in this paper.
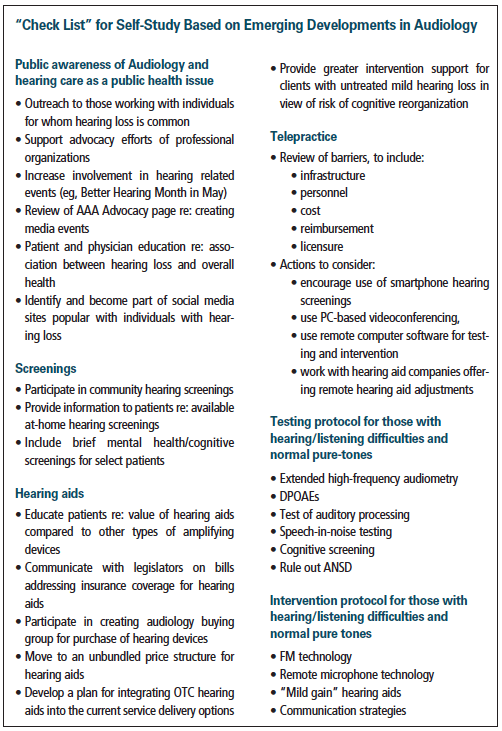
Table 2. New areas for professional development. Clinicians could develop a matrix with these items and track: if they already have these areas covered, if they are actively working on them, if there is a need for further development, or if the area is not feasible or applicable.
Acknowledgements
Thanks to Diane Flynn, AuD, Margie Halinski, AuD, and Kevin Ihrman, AuD, for their advice during the writing of this article.
Citation for this article: DeBonis D. A changing audiology landscape: Six opportunities for patients and audiologists. Hearing Review. 2021;28(4):18-22.
Correspondence to Dr DeBonis at: [email protected].
References
1. American Speech-Language-Hearing Association (ASHA) website. Aligned sense of purpose for the audiology profession. https://www. asha.org/uploadedFiles/Aligned-Sense-of-Purpose-for-the-Audiology-Profession.pdf. Published January 2019.
2. Leppla M. Hearing health coverage in the US and why there should be more. Hearing Health. 2016; Fall:16-19.
3. Glick H, Sharma A. The brain on hearing aids: Can treatment with hearing aids improve neurocognitive function in age-related hearing loss? Hearing Review. 2021;28(1):28-32.
4. Lin FR. Hearing loss and healthy aging. CaptionCall LLC white paper. https://captioncall.com/assets/uploads/images/Dr.Lin_0118_Hearing-Loss-and-Healthy-Aging_32487_FINAL2.pdf.
5. Hampton D. Nine risk factors associated with dementia. Hearing Review. 2017;25(8):22.
6. World Health Organization (WHO) website. World Report on Hearing. https://www. who.int/publications/i/item/world-report-on-hearing. Published March 3, 2021.
7. Hearing loss recognized in American Diabetes Association’s Standards of Medical Care. https://hearingreview.com/hearing-loss/health-wellness/diabetes-and-loss-are-linked-says-american-diabetes-association. Hearing Review. Published December 16, 2020.
8. Watson CS, Kidd GR, Preminger J, Miller JD, Makai D, Crowley A. Benefits of a telephone-administered national screening test. Audiology Today. 2015;27(6):42-49.
9. Barczik J, Serpanos YC. Accuracy of smartphone self-hearing test applications across frequencies and earphone styles in adults. Am J Audiol. 2018;27(4):570-580.
10. Beck DL, Weinstein BE, Harvey M. Issues in cognitive screenings by audiologists. Hearing Review. 2016; 23(2):36-40.
11. Frazer G. The future of independent practice in audiology. Audiology Today. 2017;29(4):57-61.
12. Humes LE, Herring C, Kinney DL, Main AK, Quigley TM, Rogers SE. The effectiveness of hearing aids and two service- delivery models in older adults: A randomized, double-blind, placebo-controlled clinical trial. Hearing Review. 2017;24(4):12-19.
13. Tedeschi TJ, Kihm J. Implications of an over-the-counter approach to hearing health care: A consumer study. Hearing Review. 2017:24(3):14-22.
14. Sydlowski S. Audiology pre-OTC: Changing the conversation of impending disruption. Hear Jour. 2019;72(3):44-49.
15. Myers B, Carroll B. I’m an audiologist. Come again? The Public Un-Awareness of Audiology Audiology Today. 2017;29(4):38-45.
16. Eikelboom RH, Swanepoel DW. International survey of audiologists’ attitudes toward telehealth. Am J Audiol. 2016;25(3S):295-298.
17. American Speech-Language-Hearing Association (ASHA) website. New York Telepractice Requirements for Audiologists and Speech-Language Pathologists. https://www.asha.org/Advocacy/state/info/NY/New-York-Telepractice-Requirements/.
18. Colorado Health Institute website. Value and impact of telemedicine during the COVID-19 response. https://www.coloradohealthinstitute.org/research/value-and-impact-telemedicine-during-covid-19-response. Published November 4, 2020.
19. Ciccia AH, Whitford B, Krumm M, McNeal K. Improving the access of young urban children to speech, language, and hearing screening via telehealth. J Telemedicine and Telecare. 2011;17(5):240-244.
20. Prieve BA, Schooling T, Venediktov R, Franceschini N. An evidenced-based systematic review on the diagnostic accuracy of hearing screening instruments for preschool- and school-age children. Amer J Audiol. 2015;24(2):250-267.
21. Ramkumar V, Hall JW, Nagarajan R, Shankarnarayan VC, Kumaravelu S. Tele-ABR using a satellite connection in a mobile van for newborn hearing testing. J Telemedicine Telecare. 2013;19(5):233-237.
22. Wesendahl T. Hearing aid fitting: Application of telemedicine in audiology. Int Tinnitus J. 2003;9(1):56-58.
23. Wesarg T, Wasowski A, Skarzynski H, et al. Remote fitting in Nucleus cochlear implant recipients. Acta Otolaryngol (Stock). 2010;130(12):1379-1388.
24. Angley GP, Schnittker JA, Tharpe AM. Remote hearing aid support: The next frontier. J Amer Acad Audiol. 2017;28(10):893–900.
25. Margolis RH, Morgan DE. Automated pure-tone audiometry: An analysis of capacity, need, and benefit. Amer J Audiol. 2008;17(2):109-113.
26. Windmill IM, Freeman BA. Demand for audiology services: 30-yr projections and impact on academic programs. J Amer Acad Audiol. 2013;24(05):407-416.
27. Mueller HG, Swanepoel DW. 20Q: Audiology to the people-Combining technology and connectivity for services by telehealth. AudiologyOnline. https://www.audiologyonline.com/articles/audiology-to-people-combining-technology-12183. Published October 7, 2013.
28. Beck DL, Danhauer JL, Abrams HB, et al. Audiologic considerations for people with normal hearing sensitivity yet hearing difficulty and/or speech-in-noise problems. Hearing Review. 2018;25(10): 28-38.
29. Moore D. What’s new in auditory processing? ENT and Audiology News. 2016;25(2).
30. Liberman MC, Epstein MJ, Cleveland SS, Wang H, Maison SF. Toward a differential diagnosis of hidden hearing loss in humans. PLOS One. 201611(9);e0162726.
31. Guest H, Munro KJ, Prendergast G, Millman RE, Plack CJ. Impaired speech perception in noise with a normal audiogram: No evidence for cochlear synaptopathy and no relation to lifetime noise exposure. Hear Res. 2018;364:142-151.
32. Somma G, Pietroiusti A, Magrini A, et al. Extended high-frequency audiometry and noise induced hearing loss in cement workers. Amer J Industr Med. 2008;51(6):452-462.
33. Sulaiman AH, Husain R, Seluakumaran K. Evaluation of early hearing damage in personal listening device users using extended high-frequency audiometry and otoacoustic emissions. Euro Arch Oto-Rhino-Laryngol. 2014;271:1463–1470. 10.1007/s00405- 013-2612-z
34. Musiek FE, Chermak GD, Bamiou D-E, Shinn J. CAPD: The most common ‘hidden hearing loss.’ ASHA Leader. 2018;23(3).
35. Vermiglio AJ. On the clinical entity in audiology: (Central) auditory processing and speech recognition in noise disorders. J Amer Acad Audiol. 2014;25(09):904- 917.
36. Norrix LW, Velenovsky DS Auditory neuropathy spectrum disorder: A review. J Speech Lang Hear Res. 2014;57(4):1564-1576.
37. Singh G. Why cognition matters for hearing care professionals. Hearing Review. 2015;22(9):28.
38. Johnston KN, John AB, Kreisman NV, Hall JW, Crandell CC. Multiple benefits of personal FM system use by children with auditory processing disorder (APD). Int J Audiol. 2009;48(6):371-383.
39. Kuk F, Jackson A, Keenan D, Lau C-C. Personal amplification for school-age children with auditory processing disorders. J Am Acad Audiol. 2008;19(6):465-480.
40. Saunders GH, Frederick MT, Arnold ML, Silverman SC, Chisolm TH, Myers PJ. A randomized controlled trial to evaluate approaches to auditory rehabilitation for blast-exposed veterans with normal or near-normal hearing who report hearing problems in difficult listening situations. J Amer Acad Audiol. 2018;29(1):44-62.
41. Bennett CD. Hearing aid use with minimal high-frequency hearing loss. Otolaryngol– Head Neck Surg. 1989;100(2):154-157.
42. Roup CM, Post E, Lewis J. Mild-gain hearing aids as a treatment for adults with self-reported hearing difficulties. J Amer Acad Audiol. 2018;29(6):477-494.