The first-ever placebo-controlled, double-blind, randomized clinical trial—generally considered the highest standard for methodology in clinical trials—of hearing aid outcomes shows that older adults benefit from hearing aid use, according to the American Speech-Language-Hearing Association (ASHA). The study was published in the March 2 edition of the American Journal of Audiology, an ASHA publication.
Led by researchers at Indiana University, the study sought to compare patient outcomes when hearing aids are delivered via an audiology “best practices” model compared with an “over-the-counter” (OTC) model. In the context of this study, the OTC model meant that patients received a high-quality, pre-programmed hearing aid that was not fitted by an audiologist.
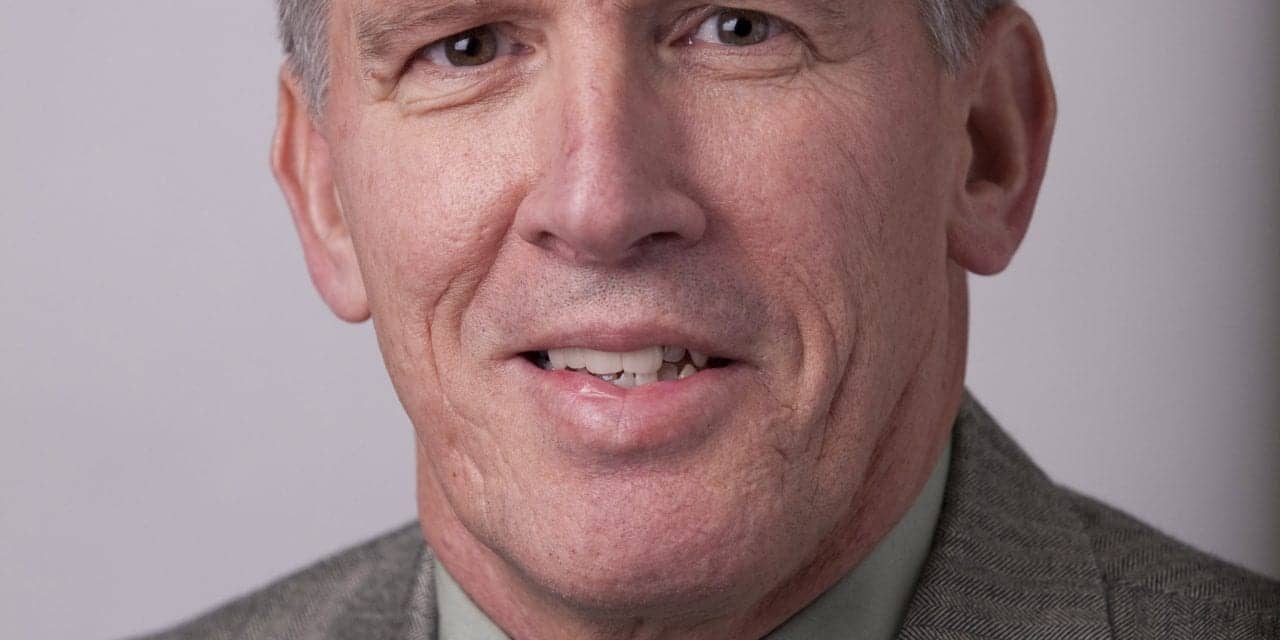
“The research findings provide firm evidence that hearing aids do, in fact, provide significant benefit to older adults,” said Larry Humes, PhD, CCC-A, a distinguished professor in the Department of Speech and Hearing Sciences at Indiana University Bloomington and the study’s lead author. “This is important because, even though millions of Americans have hearing loss, there has been an absence of rigorous clinical research that has demonstrated clear benefits provided by hearing aids to older adults. Consequently, the US Preventive Services Task Force has not been able to support widespread hearing screening for adults over age 50. This study, along with others to follow, will help establish the evidence base needed to foster better hearing health care for many older Americans.”
A summary of the outcomes of the study is provided by Dr Humes in an ASHA video available on YouTube:
The study. The researchers looked at 154 adults ages 55-79 years with mild-to-moderate hearing loss. All participants received the same high-end digital mini hearing aids fitted in both ears. Subjects were divided into three groups:
- The best practices group) received “best practices” services from audiologists that included professional fitting and counseling
- The OTC group received no professional fitting by an audiologist and selected their own pre-programmed hearing aids; and
- The placebo group received a professional fitting but used a hearing aid that was programmed to provide no acoustical benefit.
The researchers found that hearing aids are effective in older adults for both the audiology best practices model and the OTC model. There were no significant differences in outcome between these two service-delivery approaches for 5 of the 6 outcome measures, but the OTC group fared somewhat worse when it came to satisfaction with their hearing aids. Fewer OTC participants were also likely to purchase their hearing aids after the trial (55% for the OTC group vs 81% for the best practices group, with 36% for the placebo group).
Following the initial 6-week trial, both the OTC and placebo groups were offered hearing aids under the best practices model. Satisfaction significantly increased for patients in both groups who chose to continue under audiologist care, and more participants opted to purchase their hearing aids after this continued period of care than after the initial trial. The groups also were provided with the choice of two purchase prices; purchase price had no effect on outcomes, but a high percentage (85%) of those who rejected hearing aids paid the typical price.
“Efficacious over-the-counter service-delivery models (and devices) may increase accessibility and affordability of hearing aids for millions of older adults,” the authors write. “Further research is required to evaluate various devices and approaches, as well as to examine the generalization of the findings from this clinical trial.”
In the United States, a large discrepancy exists between the number of people who could benefit from hearing aids and those who actually wear them. Close to 29 million US adults could benefit from using hearing aids, according to National Institute on Deafness and Other Communication Disorders (NIDCD). Yet, among adults aged 70 and older with hearing loss who could benefit from wearing hearing aids, fewer than 1 in 3 (30%) have ever used them. Even fewer adults aged 20-69 (approximately 16%) who could benefit have ever used them.
In the study, researchers noted that NIDCD has prioritized identifying research areas that could lead to the improvement of hearing health care for adults with mild-to-moderate hearing loss—in particular, enhancing the accessibility and affordability of hearing healthcare. This study helps answer a high-priority research question of how current delivery systems can be used or modified to increase accessibility and affordability of hearing health care, according to study authors.
“More studies are needed to assess the generalization of the results obtained here to other patient populations, other devices, and other models of OTC service delivery,” said Humes. “All of the devices used in this study were of high quality as opposed to the simpler, less expensive devices many associate with an OTC model. Also, all patients received a complete audiologic evaluation prior to treatment—another potential difference from some OTC models under consideration. These factors could impact patient outcomes. However, the results of this study should serve as a yardstick for comparing outcomes of future hearing aid studies.”
The study was co-authored by Dr Humes, Sara E. Rogers, Tera M. Quigley, Anna K. Main, Dana L. Kinney, and Christine Herring, and it was funded with support (Grant No. R01 DC011771) from the NIDCD. The authors dedicated the paper in AJA to the memory of Dr Gordon Blackistone Hughes, MD, clinical trials coordinator for the NIDCD from 2008-2015.
According to the NIDCD, the study is one of 27 clinical and translational research projects throughout the United States that the NIDCD funds to develop and test novel strategies to overcome barriers to hearing health care. In addition to supporting clinical and basic research studies, the NIDCD cosponsored a consensus study conducted by the National Academies of Sciences, Engineering, and Medicine (NAS) to identify priorities for improving access and affordability of hearing health care for adults. Released June 2, 2016, the report provides a thorough analysis of the state of hearing health care for adults in the U.S. and puts forth 12 recommendations to direct hearing health care reform.
Study citation: Humes LE, Rogers SE, Quigley TM, Main AK, Kinney DL, Herring C. The effects of service-delivery model and purchase price on hearing-aid outcomes in older adults: A randomized double-blind placebo-controlled clinical trial. Am J Audiol. 2017; Published online March 2, 2017. doi:10.1044/2017_AJA-16-0111. Available at: http://aja.pubs.asha.org/article.aspx?articleid=2608398
Summary article: Also see the summary article by Humes et al in The Hearing Review.
Sources: ASHA, NIDCD




29 million people is a lot of people that could potentially benefit from hearing aids. I guess more people need to get their hearing tested. The brain loses its ability to interpret sound information is the physical ability to hear diminishes.
I have to disagree with the comment stating that there were “no significant differences in outcome between these two service-delivery approaches”. I consider “satisfaction with their hearing aids and likeliness to purchase the aid after the trial” to be a significant difference.
I think this article proves that the counselling/support provided by Audiologists is very important and that OTC models need to somehow incorporate that if they are going to be successful. Otherwise stop offering aids OTC. This point was also reiterated when “Satisfaction significantly increased for patients in both groups who chose to continue under audiologist care, and more participants opted to purchase their hearing aids after this continued period of care than after the initial trial.”
The desired end result is not the sale of the aid, but the wearing of the aid by the individual to improve their quality of life. Studies in the past have already shown that using hearing aids improve the individual’s health and emotional well being. If you do not consider acceptance and continued use of device as important, then it doesn’t matter what the other factors of comparison are.
Well said ! Thanks
The most surprising outcome? 36% of people using a placebo with “no acoustic benefit” opted to KEEP their devices. So just purchasing and wearing it creates enough subjective improvement for 1/3 of users? Folks, we have more work to do than we ever realized!
My explanation is that those people have realized it’s not such a burden to wear a hearing aid, so decided to buy one. They probably have never tried a hearing aid before, so this was for them an opportunity to test one. The fact that it actually didn’t help was only secondary. -Nicky
In general, placebos will work on 30% of people from sugar pills to fake surgeries. In essence this study is saying that people are willing to purchase OTC products at a rate of 55% compared to 36% who got a placebo device. The difference of 36% and 55% is considered “efficacious”.
I think what’s more surprising is they consider this a “rigorous” double-blind study. The person fitting the hearing aids knows whether or not the hearing aid is a placebo or not- thus making it single-blind.
It seems to me there is an agenda pushing OTC. Most people reading this would interpret this study as showing how far superior audiology best practice (81%) is over OTC (55%) as far as patient satisfaction and hearing aid usage is concerned.
Also the fact that purchase price had no effect on outcomes was surprising as well.
Could you expand on this sentence?
“The groups also were provided with the choice of two purchase prices; purchase price had no effect on outcomes, but a high percentage (85%) of those who rejected hearing aids paid the typical price.”