Loss of vestibular function due to industrial chemicals or even life-saving drugs is not uncommon and poses unique challenges for healthcare providers as well as patients.
By Richard E. Gans, PhD
Vestibulotoxicity is best defined as permanent damage to the vesibular system caused by industrial chemicals or pharmacological agents within prescribed medical treatments.(1) Acquired medical conditions affecting vestibular function (e.g., vestibular neuronitis) are predominately unilateral, temporary, and recoverable. However, as the chemical and pharmacologic causes of vestibulotoxicity are systemic, the effects are more often bilateral, and permanent. This poses challenges to clinicians, therapists, and the patients themselves in their evaluation, rehabilitation strategies, therapy protocols, and adjustment in lifestyle.
The vestibular system may be described as a finely tuned set of gyroscopes housed inside each inner ear. Its job is to detect gravity and velocity and send the signals through the central nervous system to the motor control portion of the brain. It is this role which makes the vestibular system the primary sensory contributor to normal equilibrium function. It is estimated that the vestibular system is responsible for at least 75% of the sensory information required to maintain normal balance function. The near or total loss of vestibular function results in a significant declinein physical activities, limited function in everyday activities, and poses a challenge to a person’s safety.
Common Causes of Vestibulotoxicity
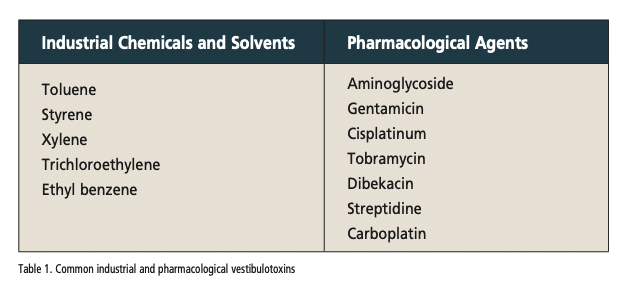
There are two main categories of agents that have vestibular toxicity:(2) chemicals and solvents used in manufacturing and industry, and pharmacological agents used to treat serious and oftentimes life-threatening medical conditions. The list of common agents both industrial and pharmacological with known vestibular toxicity are shown in Table 1. The impact of the toxicity may be increased by such variables as exposure time, concentrations or dosage, influence of polypharmacy, as well as complicating medical comorbidities like diabetes or cardiovascular disease.
The majority of the industrial chemical vestibulotoxins are used in grease cutting and as solvents including commonly used toluene. Auto mechanics, elevator repair persons, and equipment operators often use this chemical to clean their hands and machine parts. Another chemical, styrene, is a byproduct of fiberglass production. These chemicals are ingested into the bloodstream by osmosis through the skin as well as by inhalation. These chemicals may damage hair cells within all parts of the
peripheral vestibular system including the saccule, utricle, and all of the semicircular canals, in addition to damaging the balance centers in the brain.
Two of the most common vestibulotoxic medications are in the aminoglycoside antibiotic and cisplatin families. This category of drugs is used to combat difficult-to-treat and even life-threatening bacterial infections. This is most often a result of sepsis, commonly acquired during a hospital or nursing home stay. According to the Centers for Disease Control and Prevention,(3) sepsis accounts for one in three hospital deaths. Sepsis may be either bacterial or viral but is most usually bacterial, and that is the reason for the use of strong antibiotics. The sepsis may spread throughout the body through the bloodstream, damaging the vital organs.
Further reading: Fall Risk Management in Audiology and ENT Practice: The Role of Cognitive, Vestibular, and Auditory Function
The cure rate for many cancers is now estimated to be above 70%,(4) due in part to the use of highly effective drugs. One of these is Cisplatin, an effective anticancer drug commonly used in the treatment of tumor malignancies. It is delivered only through IV and does not exist in a pill form. While it is more associated with causing hearing loss and tinnitus, it can also cause neuropathy, which will affect the individual’s balance. Equilibrium is often referred to as a three-legged stool with the legs being vestibular, vision, and somatosensory. A neuropathy of the lower extremities and feet requires the other two remaining sensory systems to do more of the work, through the mechanism of substitution. However, just like a stool, if the remaining two legs are damaged or impaired or completely missing, then normal balance function will be difficult if not impossible.
Symptoms
Vestibulopathy caused by industrial solvents will be slow and insidious, over many years. A patient with this condition will unlikely be able to pinpoint a specific time or event that was a marker to the onset of their symptoms. They may report that over time, they noticed difficulty walking in the dark or riding a bicycle or some discoordination with higher level activities like playing tennis or golf.
Patients, however, who have been hospitalized or spent time in a skilled nursing facility usually can pinpoint that they noticed their balance problems after their release from the facility. Oftentimes they attribute this to being deconditioned or weak following their illness and they assume their balance will recover with return to home and normal activities. Unfortunately, it does not. They are rarely informed by the attending practitioners that the drugs that were used to save a limb from amputation or save their life have side effects, and that one of those side effects is loss of vestibular function.
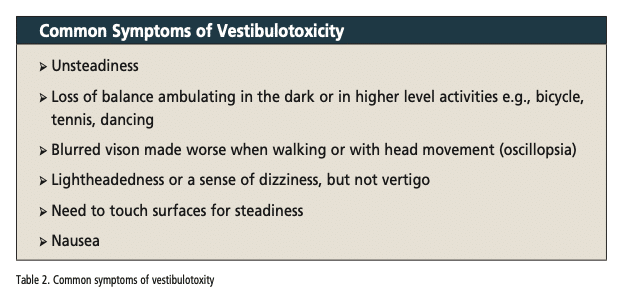
The patient may notice a wide array of symptoms, depending where on the spectrum of difficulty a particular activity or situation falls, when they will experience diminished function. Since vestibulotoxins typically cause a slower and bilateral hypofunction of both vestibular mechanisms, vertigo is rarely reported by the patient. A listing of the symptoms most commonly reported during a patient case history is presented in Table 2.
Evaluation and Management
The manifestations of vestibulotoxicity are most readily seen in assessment of balance function under challenging conditions, e.g., no, or conflicted vison and dynamic surfaces. Bedside screening procedures such as the Gans Sensory Organization Test to advanced technologies like Computerized Dynamic Posturography (CDP) are all highly sensitive to bilateral vestibular hypofunction. Simple and easily administered tests of Dynamic Visual Acuity (DVA) demonstrate the presence of blurred vision (oscillopsia) with head movement in horizontal and vertical planes and at various frequencies. This provides guidance as to the extent of the oscillopsia and what intervention strategies may be best.
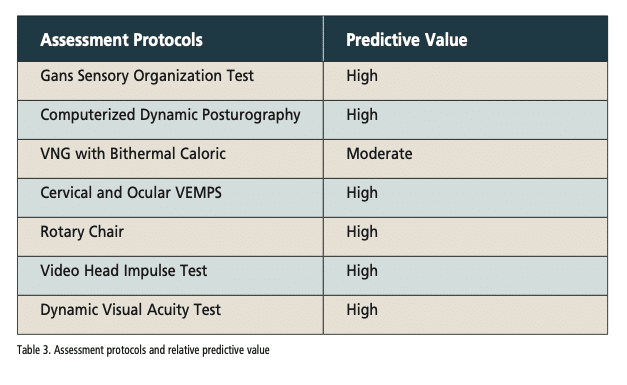
The most objective and sensitive neurodiagnostic vestibular tests are those that directly measure function of the vestibular-ocular reflexes (VOR) and vestibular evoked myogenic potentials (VEMP).(5) These range from a fairly low- cost electrophysiologic protocols such as the video head impulse test (vHIT), cervical and ocular VEMP, to the more costly rotary chair testing. A list of assessment protocols and their predictive value is shown in Table 3.
The management of the patient with bilateral vestibular hypofunction or loss will usually include vestibular rehabilitation therapy (VRT) with modification, balance retraining, and fall risk management. These are important to help keep the patient safe both inside and outside the home. The objective of VRT with the typical acquired unilateral vestibular hypofunction or loss is to train and recalibrate the brain to recognize the loss and resolve it with central compensation.(6)

Figure 1: Balance retraining on a dynamic surface helps vestibulotoxicity patients develop their substituted sensory systems.
Figure 2 (top of page): Vestibular rehabilitation therapy using virtual reality provides the patient with real-world experiences, but in a safe environment and under the supervision of their therapist. Photos by Richard E. Gans, PhD.
With one intact vestibular system, and proper treatment, and if full central compensation occurs, then the patient may have a full recovery for everyday activities. However, the reduction or loss of both systems will not allow the patient a recovery of normal balance function. Substitution protocols will include the use of a range of dynamic and challenging surfaces e.g., standing on foam, walking on a trampoline with eyes open and closed and with head movement at various speeds and direction. Virtual reality, if available, is also an excellent tool, as it provides the patient with real-world experiences, but in a safe environment and under the supervision of their therapist. Figures 1 and 2 depict these therapy protocols respectively.
Perhaps one of the most annoying symptoms for the vestibulotoxicity patient is oscillopsia. In some individuals it is so debilitating that even chewing will destabilize their vision. Oscillopsia is one of the cardinal complaints and will need to be addressed using gaze stabilization therapy protocols in the direction and speed that is causing the blurred vision.(7) Fortunately, this therapy has been shown to be highly effective.
The vestibulotoxicity patient will become visually and surface dependent. Substitution will be a primary therapeutic intervention strategy, as they are essentially keeping their balance with their eyes and sense of touch. Therefore, it’s critically important to evaluate and know the status of these back-up or substituted sensory systems. If the patient also has a diabetic retinopathy and neuropathy of the feet, now there are co-morbidities and compounding challenges. This is where an interdisciplinary approach is imperative to helping the patient enjoy an improved quality of life. Collaboration with rehabilitation specialists, physical and occupational therapists, and physiatrists will be important in guiding the patient to once the diagnostic evaluation is complete. It is important to counsel the patient extensively as to lifestyle adjustments and the importance of ongoing evaluation and intervention if needed to their vision and somatosensory systems. Even an outdated eyeglass prescription may be problematic.
Summary
Vestibulotoxicity is a condition that damages the vestibular system, which is responsible for balance and spatial orientation. It can be caused by industrial chemicals and solvents and pharmacological agents. Symptoms of vestibulotoxicity may include unsteadiness, difficulty with ambulation, blurred vision with head movement, dizziness, and nausea. In many cases, vestibulotoxicity can be permanent. There is no cure for this condition. Vestibular rehabilitation therapy (VRT), balance retraining, and fall risk management can help reduce the functional impairment and maintain an improved quality of life.
Since many patients may be unaware of the cause of their symptoms, it is incumbent on the clinician to remember to ask those questions about employment, type of work environment, exposure to solvents and chemicals, as well as medical treatments in hospital or cancer treatments as part of the patient’s case history if possible vestibulotoxicity is suspected. Patient counseling as to lifestyle modifications and ongoing maintenance of sensory modalities is an integral part of the patient’s journey to an active and safe life.
Richard E. Gans, PhD, is the founder and CEO of the American Institute of Balance (AIB). He is a past president of the American Academy of Audiology, a research scientist member of the American Academy of Neurology, and a scientific fellow member of the American Academy of Otolaryngology Head and Neck Surgery.
References:
1. Gans RE, Rauterkus G; Research Associate 1. Vestibular Toxicity: Causes, Evaluation Protocols, Intervention, and Management. Semin Hear. 2019 May;40(2):144-153. doi: 10.1055/s-0039-1684043. Epub 2019 Apr 26. PMID: 31036991; PMCID: PMC6486364.
2. Handelsman JA. Vestibulotoxicity: strategies for clinical diagnosis and rehabilitation. Int J Audiol. 2018 Sep;57(sup4):S99-S107. doi: 10.1080/14992027.2018.1468092. Epub 2018 May 9. PMID: 29741128.
3. Sepsis. Centers for Disease Control and Prevention. Available at https://www. cdc.gov/sepsis/index.html. Published July 20, 2018.
4. Brenner H. Long-term survival rates of cancer patients achieved by the end of the 20th century: a period analysis. Lancet. 2002 Oct 12;360(9340):1131-5. doi: 10.1016/S0140-6736(02)11199-8. PMID: 12387961.
5. Gans RE, Sakumura JA. Assessment of vestibular function. In: Atcheson, S. ed. Audiology: Diagnosis. 3rd. Edition New York: Thieme; 2023 IN PRESS
6. Gans R. Vestibular rehabilitative therapy. In: Handbook of Clinical Audiology Seventh Edition. Katz J, Chasin M, English KM, Hood LJ, Tillery KL, eds. Lippincott William & Wilkins; 2015:425–433
7. Roberts RA, Gans RE. Comparison of horizontal and vertical dynamic visual acuity in patients with vestibular dysfunction and nonvestibular dizziness. J Am Acad Audiol. 2007;18(03):236–244