Tech Topic | November 2022 Hearing Review
Neurodiagnostic auditory-vestibular findings may result in peripheral and central abnormalities in the migraine population.
By Richard E Gans, PhD and Joseph Sakumura, AuD
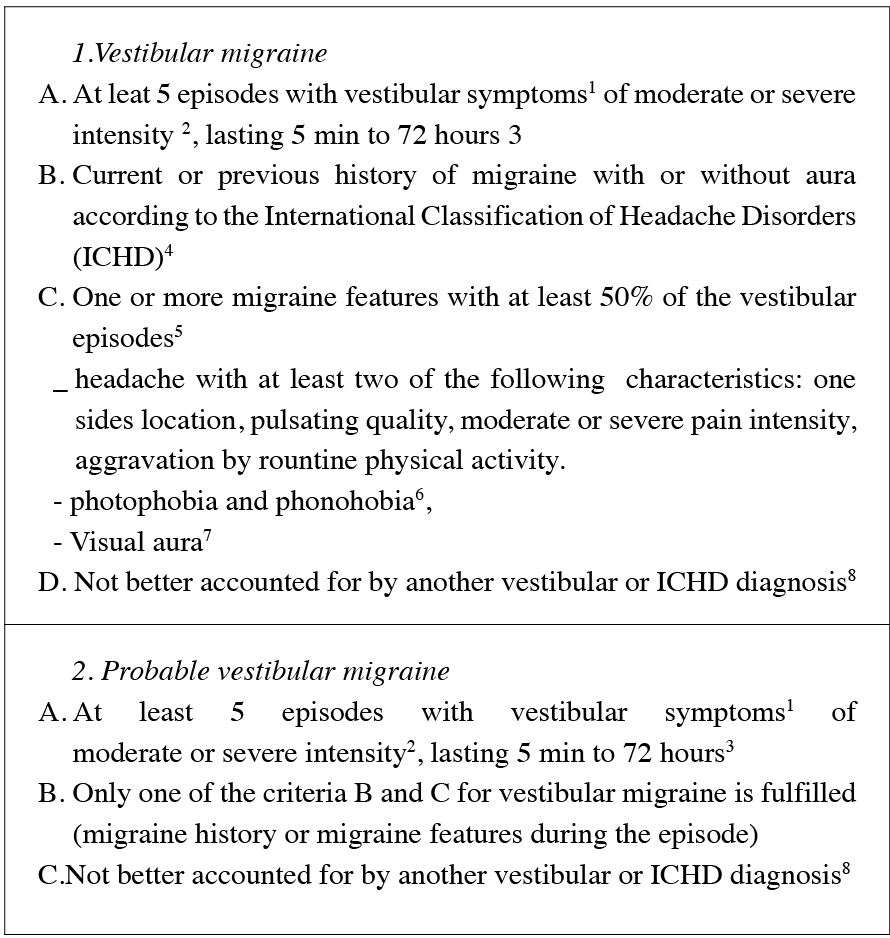
One of the greatest challenges in the evaluation and management of patients with migraine is the diversity in the presentation of symptoms among patients, and the variability in diagnostic testing results. As discussed in Part 1 of this series, patients with migraine often present to audiology and ENT clinics with complaints of acute or chronic dizziness and vertigo either with or without headache.1 Fluctuating hearing loss, as previously discussed, while it does occur, is likely no more than 5% in this population. The audiovestibular symptoms associated with migraine, whether peripheral or centrally mediated, are now described, or classified as vestibular migraine (VM). The diagnostic criteria for VM are shown in Figure 1. Not only can neurologic processes result in audiovestibular symptoms, but migraineurs also have a higher incidence of benign paroxysmal positional vertigo (BPPV), Ménière’s disease, vestibular neuritis, and other otologic comorbidities.2 Understanding the nature of involvement (peripheral vs central, or both) is critically important in determining the best course of treatment (eg, vestibular rehabilitation therapy, pharmacotherapy, and lifestyle modifications) ultimately producing successful outcomes in these patients.3
Just as the symptom profile of patients with migraine can be diverse and complex, neurodiagnostic studies may produce highly variable results in these patients. This article will describe abnormalities in test findings typically associated with migraine patients through anecdotal findings and case studies.
Neurodiagnostic Findings in Patients with Migraine
As with any patient presenting with complaints related to hearing or balance function, we recommend a basic audiological examination, followed by a comprehensive neurodiagnostic evaluation. The assessment protocols should include tests that have high sensitivity, specificity, and a good predictive value. An audiometric evaluation should be completed to identify the presence of any sensorineural loss or middle ear dysfunction. The pattern of hearing loss, if present, is an important indicator providing insight as to the nature of involvement. For example, Ménière’s disease often presents with a pattern of low-frequency hearing loss as opposed to migraine which may very often leave hearing intact, or present with a high-frequency pattern of loss. Retrocochlear or central nervous system (CNS) influence should always be considered, should an asymmetry in hearing be identified.
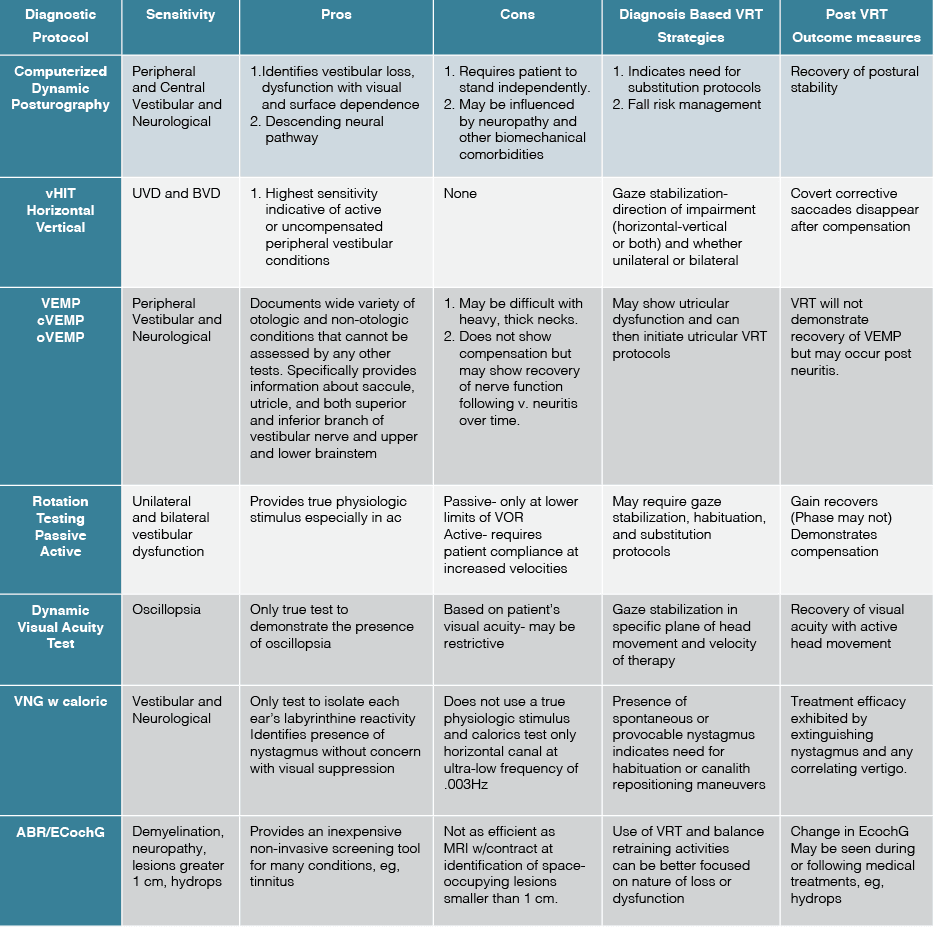
Following traditional audiometric assessment, patients with complaints of dizziness, vertigo, or imbalance will be best served by undergoing a complete neurodiagnostic vestibular evaluation whenever possible. This typically will include postural stability assessment, videonystagmography (VNG), caloric, rotational chair, brainstem auditory evoked potentials, electrocochleography, cervical and ocular VEMP, and video head impulse testing. As migraine, Ménière’s, and multiple sclerosis (MS) may often pose a diagnostic enigma, it is important to not guess at the underlying causation or comorbidities. For example, 50% of all individuals with MS, will have at least one acute attack of vertigo within the course of the disease and are also prone to non-BPPV positional vertigo. Table 1 outlines the most common neurodiagnostic findings associated with vestibular migraine.
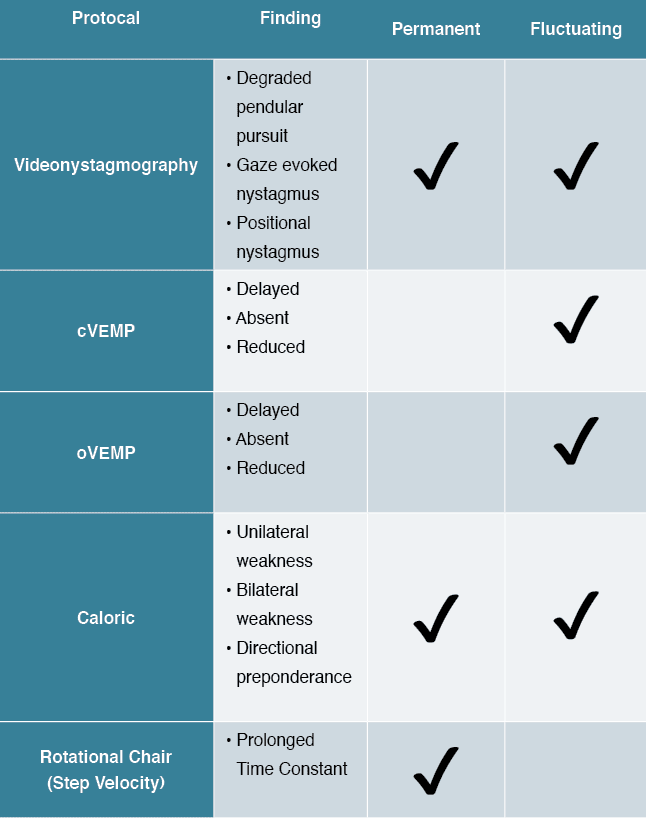
Table 2 summarizes the gold-standard test protocols as well as their sensitivity. It is important to understand that as a variable disorder of nervous system function, migraine can present with many different phenotypes, symptom profiles, and complaints. The results of neurodiagnostic testing in migraineurs may display a wide array of abnormalities including caloric weakness, positional and gaze-evoked nystagmus, VEMP asymmetry, and degraded ocular motility.4,6 Therefore, a combination of peripheral and central nervous system test findings are not uncommon. This is demonstrated in the literature, and anecdotally in clinical practice. Of critical importance is the integration of all findings with the patient’s clinical presentation, pertinent medical history, and other previously obtained medical studies (eg, MRI, CT, etc…). The following case studies illustrate the diversity in patient symptoms and corresponding neurodiagnostic findings across the lifespan.
Case Study One
History: A 50-year-old female patient presented to the American Institute of Balance (AIB) with the primary complaint of episodic vertigo. She is referred by PCP and ENT and has lifelong issues associated with menstrual migraine including motion intolerance. She denies any prior history of otologic, cardiovascular, or neurologic conditions. This patient underwent a hysterectomy approximately 6 months ago, and, subsequently, episodic vertigo began. These episodes typically last 30 minutes to 2 hours in duration and are not accompanied by any hearing loss or otologic complaints. The patient also denies any residual complaints of oscillopsia or balance dysfunction between episodes. She also denies any known triggers and reports episodes seem to be random.
Examination: Neurodiagnostic evaluation included audiologic testing, postural stability (Gans SOP), dynamic visual acuity, VNG, caloric, rotational chair, cervical and ocular VEMP, ECochG, and rate study ABR. All findings were within normal limits apart from a 36% caloric weakness on the right side. It has been reported that up to 30-50% of migraine patients present with a unilateral caloric weakness.6 This may be more related to vestibulo-cerebellar origins than labyrinthine, secondary to migraine. This caloric weakness should be interpreted cautiously. Given the absence of any other abnormalities, the likelihood that this patient has an active, acute, or uncompensated peripheral vestibular dysfunction contributing to complaints is unlikely. Findings collectively suggest a non-labyrinthine etiology to complaints.
Recommendations: The nature of her sudden onset of symptoms and negative ENT and peripheral audiovestibular findings strongly suggested the trigger was likely the “instant menopause effect” and she was encouraged to return to her OB/GYN. As migraine is shown to be heavily hormonally influenced,7 particularly by the sex hormones of estrogen and progesterone, a hormone panel and any medical intervention seen fit by the attending physician is often beneficial in patients with this clinical profile.
Outcomes: The patient was then further evaluated by her OB/GYN and reported to us the following:
“I came to your office, as a last resort, trying to track down the cause of what had become almost debilitating dizziness. After ruling out all other causes, you shared with me that the ‘instant menopause’ I had been experiencing after a recent hysterectomy, and the likely hormone imbalance, was the culprit. As soon as I returned home, I visited my OB/GYN and we found that my estrogen hormone replacement therapy (HRT) needed to be complemented by progesterone as well. Within six days my dizziness and all of the related migraine symptoms I had been experiencing disappeared! I have followed a regimen of daily estrogen/progesterone combined with about 8mg of prophylactic Topamax for the past five months, and I feel like I have my life back. I cannot tell you how grateful I am to you for helping me through the worst health issue I’ve ever faced. Again, please know that I am very, very grateful and that I will continue to spread the word as well. It changed my life to finally have this addressed and I am just so thankful!”
Case Study Two
History: An 8 year, 7-month-old female patient presents to the AIB with the primary complaints of internal motion which is episodic and accompanied by headache and nausea. She denies any known triggers or provoking factors and has normal equilibrium developmental milestones. Of note, her mother and uncle both have a reported migraine history. The mother reported that her daughter may be pre or peripubescent.
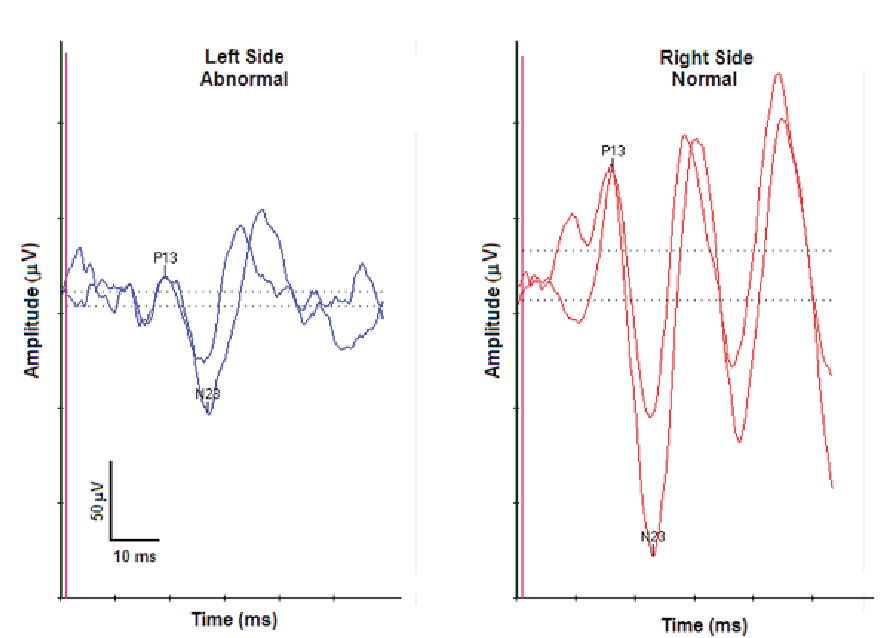
Examination: All audiologic, peripheral vestibular, and equilibrium studies completed were within normal limits except for an asymmetrical cervical VEMP with reduced amplitude on the left side. Figure 2 shows this asymmetry. Abnormal neurodiagnostic results are more common in children with migraine than adults.8 In this case the isolated abnormality of an asymmetrical cVEMP must be interpreted cautiously. This finding in isolation does not indicate a peripheral vestibular involvement but rather is likely influenced by neural substrates involved with migraine.
Recommendations: Results were provided to the pediatrician and a suggestion for referral to pediatric neurology for evaluation and medical management of a possible puberty-onset migraine variant. Lifestyle modifications beyond any recommended medical management, including trigger identification and removal, sleep hygiene, and stress management, were also discussed.9
Outcomes: The patient and her parents worked with her pediatrician on a prophylactic medication regimen, in addition to being mindful of lifestyle modifications, trigger identification, and removal. The parents reported to us a significant improvement in their daughter’s symptoms, but understand, as this is a predominately a hormonal trigger, they will need to stay in close contact with the physicians.
Summary
The purpose of this discussion is to provide the reader with an understanding of how variable the clinical and diagnostic profile of patients with migraine can be. The pathophysiology of migraine is complex, involving cortical and subcortical substrates of the central nervous system, as well as involvement of the peripheral mechanism. Additionally, the genetic factors and cellular dysfunction involved in migraine have expressivity throughout not only the brain, but also the peripheral audiovestibular system. Clinicians must be aware of the mixed findings that may result in neurodiagnostic audiovestibular evaluation and understand how to integrate test results along with the patient’s functional impairment and clinical profile. As migraine is defined as a genetic or familial neurologic disorder, it is important to consider migraine as a potential causation of dizziness and vertigo in both children and adults throughout their lifespan.
Citation for this article: Gans RE, Sakumura J. Part 2: Audiovestibular symptoms related to migraine – What audiologists and ENTs need to know in 2022 for expanding patient care. Hearing Review. 2022;29(11):20-24.
References
- Gans RE. Classification of audiovestibular symptoms related to migraine, Part 1: Overview of migraine. Hearing Review. 2002.
- Lempert T, Olesen J, Furman J, et al. Vestibular migraine: Diagnostic criteria. Journal of Vestibular Research. 2012;22(4):167–172.
- Gans R, Rutherford K. A multidisciplinary approach to the management of the adult balance – dizzy patient. ENT & Audiology News. 2020;29(2):2–4.
- Huang TC, Wang S-J, Kheradmand A. Vestibular migraine: An update on current understanding and future directions. Cephalalgia. 2019;40(1):107–121.
- Beh SC, Friendman DI. Vestibular migraine. Current Neurology and Neuroscience Reports. 2022.
- Lempert T, Bronstein A. Management of common central vestibular disorders. Current Opinion in Otolaryngology & Head & Neck Surgery. 2010;18(5):436–440.
- Cetinkaya A, Kilinc E, Camsari C, Ogun MN. Effects of estrogen and progesterone on the neurogenic inflammatory neuropeptides: Implications for gender differences in migraine. Experimental Brain Research. 2020;.238(11):2625–2639.
- Casani AP, Sellari-Franceschini S, Napolitano A, Muscatello L, Dallan, I. Otoneurologic dysfunctions in migraine patients with or without vertigo. Otology & Neurotology. 2009;30(7):961–967.
- Roberts RA, Watford KE, Picou EM, Hatton K, Trone TH, Brignola EY. Effects of lifestyle modification on vestibular migraine. Otology & Neurotology. 2021;42(10):e1537-e1543.