The extent to which HCPs involve family members in audiology appointments depends on the topic being discussed, among other factors, according to the results of an international survey.
Figure 1. An estimation of the percentage of appointments where a family member was present, broken down by country.
By Jennifer Appleton-Huber, MSc; Stacey Rich, MCIAud, AudA; Angela Pelosi, MAud, eMBA; Louise Hickson, PhD; Barbra Timmer, PhD, MBA; Bettina Turnbull, AuD; Gabrielle Saunders, PhD; Gurjit Singh, PhD; Jill Preminger, PhD; Joseph Montano, EdD; Nerina Scarinci, PhD; and Patricia McCarthy, PhD
Family-centered care (FCC) is an approach to hearing healthcare that recognizes the vital role that families play in the hearing intervention process. Family is defined here as any significant communication partner involved in the life of the person with hearing loss. Indeed, there has been longstanding recognition within the audiology community of the negative psychosocial consequences of hearing loss on family members and the third-party disability experienced by significant others.(1,2,3) Research into the implementation of FCC in areas outside of audiology has reached the broad consensus that FCC yields superior health outcomes, particularly with regard to patient well-being, adherence to treatment recommendations, and satisfaction with (4,5) medical services.
Research conducted in audiology has also demonstrated the benefits of FCC, showing that outcomes are improved when family is engaged throughout the rehabilitation process. Specifically, it has been shown that the family of clients with hearing loss encourage help-seeking and advocate for the adoption of hearing instruments,(6,7,8) assist in providing instruction on the proper use and care of devices,(9) increase a person’s confidence in their ability to manage their hearing loss,(10) and reinforce the importance of following treatment recommendations.(11,12) It has also been found that hearing disability decreases when patients are accompanied by family members during audiologic rehabilitation classes.(13) FCC also provides an opportunity to address the third-party disability experienced by family members of adults with hearing loss.(14)
In 2016, Phonak released a position statement,(15) prepared by the FCC Expert Circle on Hearing Healthcare chaired by Professor Louise Hickson. The FCC Expert Circle was convened to provide evidence-based recommendations to HCPs about how to best facilitate family involvement throughout the hearing intervention process. Since then, several articles,(16,17,18,19,20,21) podcasts, and tools(22) have been developed to help HCPs implement FCC in their practice. Most recently, the FCC Expert Circle recommended that a survey be conducted to better understand when and how FCC is being implemented in audiological care. The results of the survey are discussed in this article.
Survey of FCC Use in Audiology
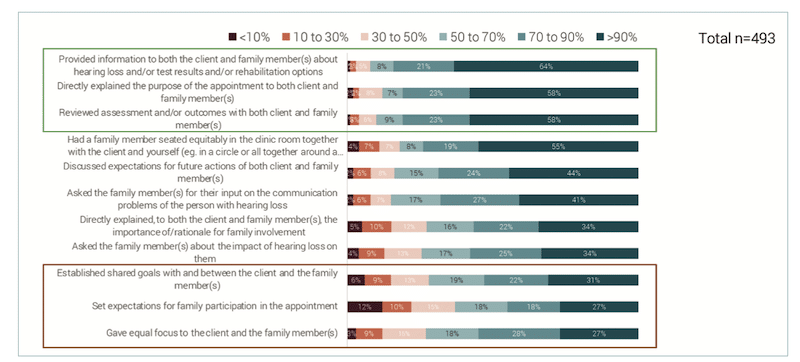
Figure 2. An estimation of how often HCPs involved family members in specific appointment activities.
In the absence of any prior studies, Phonak commissioned a series of interviews with HCPs to find out when, whether, and how elements of FCC were being implemented in clinics with a view to identifying what further resources are needed if FCC is to be broadly implemented, and where to focus efforts on training and support. The survey was based on an FCC checklist of observable family-centered clinical behaviors (see Figure 2) developed by Scarinci and Hickson for use in another study to quantify the number of family-centered behaviors used in a hearing care appointment. The 20-item FCC checklist was based on research evidence and the behaviors targeted in an FCC intervention trialed in Australia to increase the family-centeredness of hearing care appointments.
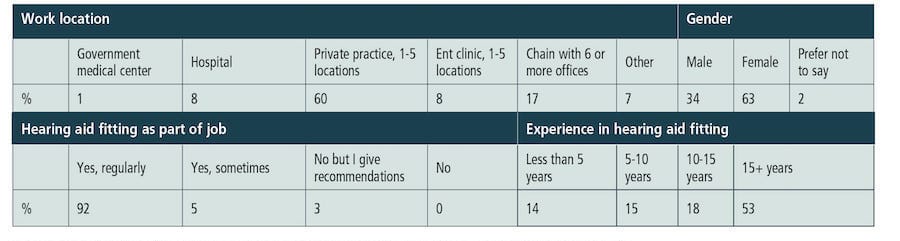
Table 1. Relative distribution of HCPs with regards to work location, gender, hearing aid fitting as part of their job and experience in hearing aid fitting.
Online semi-structured interviews lasting between 8 and 12 minutes were conducted with 493 HCPs from seven different countries (USA, Germany, France, UK, Australia, Canada, and New Zealand). Table 1 shows the distribution of HCPs with regard to work location, gender, hearing aid fitting as part of their job, and experience in hearing aid fitting. The surveys took place in October and November 2021 in the USA and in January and February 2022 in the other countries. As COVID-19 restrictions were in place to varying degrees in all countries, this may have impacted the results.
How Often HCPs Practice FCC
HCPs were first asked to think about the office appointments that had taken place with adults with hearing loss over the prior month. They were asked to estimate the percentage of appointments in which a family member (friend, caregiver, guardian) had been present in the clinic room. Figure 1 shows the results separated by country. A family member was reported to attend in more than 50% of appointments in France, New Zealand, and the USA, as compared to less than 25% of the time in Germany and Australia.
For appointments in which a family member was involved, HCPs were asked to estimate how often they involved the family member in specific appointment activities. Figure 2 shows that HCPs mostly involved family members when providing information about hearing loss and reviewing test results. It was less common for HCPs to give equal focus to the client and family member and to involve them in setting expectations and establishing shared goals.
When broken down by country, HCPs in the USA, UK, and Canada appeared to involve the family member in many of the appointment activities, whereas those in Germany less so. When the data were examined in terms of the age of the HCP, it was observed that HCPs aged 30 years and younger more often reported involving family members when providing information about hearing loss and reviewing test results, while HCPs aged 50+ years were more likely than younger HCPs to ask the family member about the impact of hearing loss on them and to directly explain the rationale for family involvement.
HCPs who reported working in a hospital were much more likely to have a family member sit in an equitable position in the clinic room, and to directly explain the purpose of the appointment to both client and family member, than those who reported working in private practice or an ENT clinic.
How Comfortable Are HCPS with FCC?
In response to the question “How comfortable are you having a family member in the clinic room for appointments with adult clients?” More than 90% said they were very or rather comfortable. This was the case for HCPs in all countries.
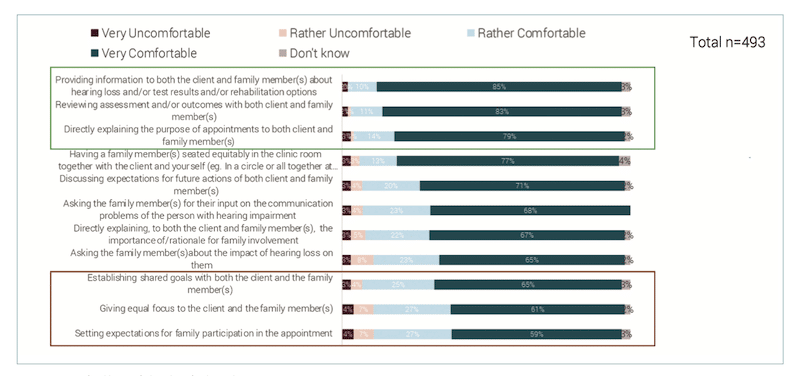
Looking at comfort in closer detail, HCPs were asked to describe the activities in which they felt comfortable involving a family member. Figure 3 shows that HCPs feel most comfortable providing information about hearing loss and reviewing tests with both the client and a family member. They felt least comfortable with giving equal focus to the client with hearing loss and family member and when setting expectations for family participation in the appointment.
When broken down by country, HCPs in the USA, Canada, and UK were comfortable involving family members in most appointment activities (Figure 3). Further analysis showed that younger HCPs (30 years and younger) and less experienced HCPs (less than 5 years in practice) seemed to be slightly less comfortable involving family members. This finding is interesting as the younger age group reported often involving family members, at least when providing information about hearing loss and reviewing test results. The work location (private practice/small chain/large chain/ government) didn’t seem to influence how comfortable the HCP was with FCC.
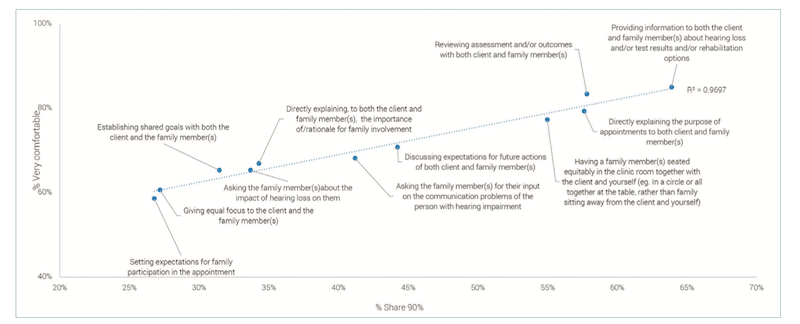
Comfort, Application Highly Correlated
A high correlation (.97) was found between how comfortable HCPs felt with FCC and how often they reported that family members were involved, for the various aspects of the appointment (Figure 4).
FCC for Different Client Groups
HCPs were asked to think about the client groups for which they would involve family members. They were provided with a list of client groups including the option of ‘other’. Figure 5 shows that HCPs reported family members being most commonly involved when the clients with hearing loss have cognitive impairment or if they speak a different language than the HCP.
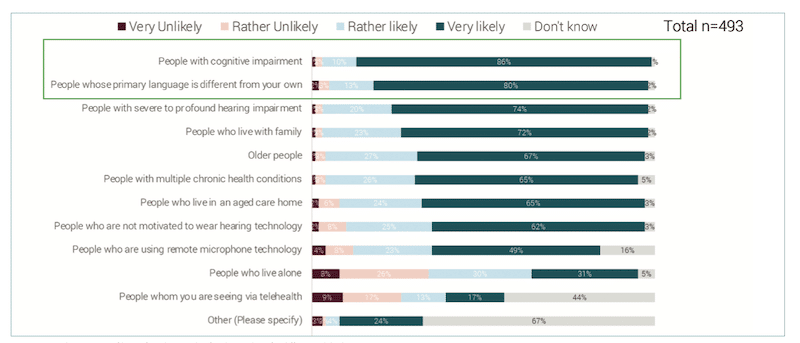
When broken down by country, the pattern was mostly the same. With the exception of clients with cognitive impairment, clients who spoke a different language, and clients with severe-profound hearing loss, HCPs in Germany involved family members less than the other countries. Further analysis of client group data showed that older HCPs were more likely than younger ones to involve family members for older clients and for those clients who lived alone.
Discussion
This survey highlights that HCPs see many benefits to FCC and find it has a positive impact on their practice. The survey indicated that HCPs are likely to involve family members in aspects of an appointment if the HCP is comfortable doing so. Although 90% of HCPs reported being comfortable having a family member present at the appointment, many reported not being comfortable giving equal focus to client and family members or developing shared goals. Importantly, this survey highlights the areas where more work is needed in supporting HCPs to successfully implement comprehensive FCC.
References:
- Kamil RJ, Lin FR. The effects of hearing impairment in older adults on communication partners: A systematic review. J Am Academy Audiol. 2015; 26(2): 155-182.
- Meyer C, Scarinci N, Ryan B, Hickson L. There is a partnership between all of us: Audiologists’ perceptions of family member involvement in hearing rehabilitation. Am J Audiol. 2015; 24: 536-548.
- Ekberg K, Timmer BH, Francis A, & Hickson L. Improving the implementation of family-centred care in adult audiology appointments: a feasibility intervention study. Int. J. Audiol. 2023; 62(9): 900-912. https://doi.org/10.1080/14992027.2022.2095536
- Stewart M, Brown J, Donnar A, McWhinney I, Oates J, Weston W, Jordan J. The impact of patient-centered care on outcomes. J Family Practice. 2000; 49: 796- 804.
- Rathert C, Wyrwich MD, Boren SA. Patient-centered care and outcomes: a systematic review of the literature. Med Care Res Rev. 2013; 70: 351-379.
- Laplante-Lévesque A, Hickson L, Worrall L. Predictors of rehabilitation intervention decisions in adults with acquired hearing impairment. J Sp Lang Hear Res. 2011; 54(5): 1385-1399. doi: 10.1044/1092- 4388(2011/10-0116)
- Mahoney CFO, Stephens SDG, Cadge BA. Who prompts patients to consult about hearing loss?. Brit J Audiol. 1996; 30(3): 153-158.
- Laplante-Lévesque A, Hickson L, Worrall L. Factors influencing rehabilitation decisions of adults with acquired hearing impairment. Int J Audiol. 2010; 49: 497-507.
- Manchaiah VK, Stephens D. Perspectives on defining ‘hearing loss’ and its consequences. Hearing, Balance and Commun. 2013; 11(1): 6-16.
- Meyer C, Hickson L, Lovelock K, Lampert M, Khan A. An investigation of factors that influence helpseeking for hearing impairment in older adults. Int J Audiol. 2014; 53(1): 3-17.
- Carson AJ. “What brings you here today?” The role of self-assessment in help-seeking for age-related hearing loss. J Aging Studies. 2005; 19(2): 185-200.
- Lockey K, Jennings MB, Shaw L. Exploring hearing aid use in older women through narratives. Int J Audiol. 2010; 49(8): 542-549.
- Preminger JE. Should significant others be encouraged to join adult group audiologic rehabilitation classes? J Am Acad Audiol. 2003; 14(10): 545-555.
- Scarinci, N. Family-Centered Care in Adult Audiologic Rehabilitation. In J. J. Montano & J. B. Spitzer (Eds.), Adult Audiologic Rehabilitation (3rd ed.). San Diego, CA: Plural Publishing; 2020.
- Singh G, Hickson L, English K, Scherpiet S, Lemke U, Timmer B, Buerkli-Halevy O, Montano J, Preminger J, Scarinci N, Saunders G, Jennings MB, Launer S. Family-Centered Adult Audiologic Care: A Phonak Position Statement. Hearing Review. 2016. 23(4): 16.
- English K, Jennings M, Lind C, Montano J, Preminger J, Saunders G, Singh G, Thompson E. Family-centered Audiology Care: Working with Difficult Conversations. Hearing Review. 2016. 23(4): 14.
- Turnbull B. How Do I Implement Family-centered Care in my practice? Hearing Review. 2016. 23(12): 22-24.
- Singh G, Barr C, Montano J, English K, Russo F, Launer S. Family-Centered Audiology Care: Emotion and Reason in Hearing Healthcare. Hearing Review. 2017. 24(5): 30-32.
- Hickson L, Lind C, Preminger J, Brose B, Hauff R, Montano J. Family-centered Audiology Care: Making Decisions and Setting Goals Together. Hearing Review. 2016. 23(11): 14-19.
- Saunders G, Preminger J, Scarinci N. Family-centered Care: Working with Partners Reporting “Incongruent” Hearing Aid Outcome, Hearing Review 2017. 24(2): 26-30.
- Timmer B, Jennings MB. I am already family-centered, so what’s the hype? Hearing Review. 2018
- Hearing Aid Counseling Tools for Family-Centered Care | Phonak, available at www.phonak.com/en-int/professionals/audiology-hub/family-centered-care, accessed on 18.10.2023





You will forgive me, but when you dehumanize people with labels or letters or function, the whole process you are trying to explain falls to pieces on the ground, like a broken window pane. All of that research is just wasted, the outcomes worthless, these are people, not HCP or PCP or anything like that. Show some wisdom with your knowledge.