By Barbara Roe Beck, MA
| Individuals with CAPDs comprise a heterogenous group with various processing strengths and weaknesses that influence their auditory learning. The deficits of their CAP can be determined by using a battery of tests with known sensitivity to lesions in various regions of the brain. This article details how these deficits can be remediated using a three-pronge approach of skill-building, environmental modifications and compensatory strategies. |
Central auditory processing (CAP) disorders are receiving attention from hearing care professionals, parents, physicians, educators and other professionals. In part, similarities in symptoms between patients with central auditory processing disorders (CAPDs) and those with ADD, ADHD and language disorders may be responsible for the renewed interest in CAPDs.
Increasingly, hearing care professionals are called upon to identify and manage patients with suspected CAPDs. Audiologists are also asked about effective strategies for managing CAPDs, with the goal of minimizing the impact of CAPDs on a child’s educational performance. Unfortunately, many hearing care professinals are uncertain what tests should be included in a CAP test battery. Further, once the diagnosis is made, the question of appropriate remediation arises.
In this article, the CAP battery and intervention program used in the Department of Communication Disorders at Saint Louis Univ. will be discussed. It is hoped this model will serve as a starting point for hearing care professionals interested in working with people who have CAPDs. Although our caseload is comprised exclusively of children to date, these techniques can be modified for use with adults as well. As in many areas of hearing care, there is more than one “right” approach to this subject. The opinions and practices expressed are those of the author, who takes sole responsibility for them.
Defining CAP
The American Speech-Language-Hearing Association (ASHA) Task Force on Central Auditory Processing arrived at this definition of CAP in 19961: “Central Auditory Processes are the auditory mechanisms responsible for the following behavioral phenomena: sound localization and lateralization, auditory discrimination, auditory pattern recognition… and temporal aspects of audition, including temporal resolution, temporal integration, temporal masking, temporal ordering…” The ASHA definition also states that CAP can be defined by “auditory performance decrements with competing or degraded acoustic signals.”1
Note this definition does not include higher cognitive functions, such as memory. Indeed, as the term implies, central auditory processing is a lower neurologic function: “Memory, learning, attention, long-term phonological representation, and other higher neurocognitive processes are considered in the definition only as they relate to the processing of acoustic signals.”2 For this reason, CAP tests which rely heavily on memory of auditory information are not included in the Saint Louis Univ. CAP battery.
Anatomy and Physiology: Starting Points
Although a detailed description of the anatomy and physiology of the central auditory system is beyond the scope of this article, a few points should be articulated as background. First, the central auditory nervous system has plasticity, defined as the ability to make organizational changes as a result of internal or external processes. If there is not agreement on this, many of the remediation techniques are pointless. Auditory processing is a skill much like musical ability: all of us have some aptitude at birth, all of us can improve with training (due, in part, to neural plasticity), but not all of us will reach the same level of proficiency.
Secondly, there is relative strength and efficiency in the contralateral CNS pathways when compared to the ipsilateral pathways. This becomes important when interpreting performance on dichotic tasks.
Third, myelination of the corpus callosum in humans is not complete until age 11 or 12 years. This can lead to a right ear advantage (REA) on dichotic tasks in younger patients. This is because the information presented to the left ear goes along the stronger contralateral acoustic pathways to the right hemisphere. The information then has to cross the (not fully myelinated) corpus callosum to the language-dominant left hemisphere to be expressed as a verbal response. Keith3 has described a strong REA in older children as representation of an “immature” auditory system.
Validity of CAP tests
One of the concerns in the identification of any disorder is “What are the best tools to use? Can one or two tests confirm the diagnosis, or is a test battery approach necessary? How is the validity of the tests determined?”
Musiek4 suggested the following: “…Test efficiency must be validated on proven lesions involving the CANS. There is no other way to determine the validity of a central auditory test; validity of a particular test cannot be obtained by testing children with learning disabilities, primarily because not all children with LD have CAPD.” At Saint Louis Univ., the test battery used for the identification of a CAP disorder is comprised only of tests that have been shown to be sensitive to physiologic lesions of the auditory pathways.5,6,7,8
In addition, “One way to improve the diagnostic specificity of CAPD is to determine that the observed perceptual deficits are indeed modality-specific…In the case of CAPD, the deficit should occur primarily when the subject deals with acoustic information and not when similar information is presented in other sensory modalities (e.g., visual, tactile or olfactory).”9 For this reason, the test battery we use does not include tests with printed materials.
Finally, in determining our battery, we have chosen tests that target the various processes that contribute to effective auditory processing. These processes include:
- Binaural integration, defined as the ability to discriminate different messages presented to each ear simultaneously;
- Auditory closure, defined as the ability to “fill-in” auditory information when a portion of the message is missing or distorted;
- Tests of the prosodic aspects of speech such as rhythm, intonation, syllabic stress and key word detection, and
- The ability to discriminate speech in the presence of background noise.
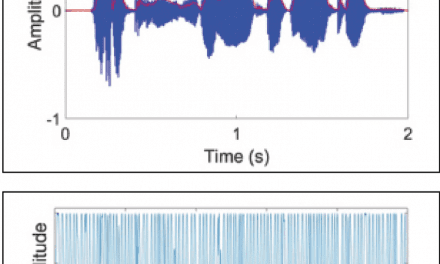
It is also important to recognize that recent literature10 has shown electrophysiologic tests to play an increasingly important role in our understanding of central auditory function.
CAP Battery
As previously stated, a battery of tests is used by St. Louis Univ. that have been proven to be sensitive to lesions of the auditory system. Closer examination of the tests will reveal what kinds of information they contribute to knowledge about an individual’s CAP abilities.
- Staggered Spondaic Word (SSW) Test: The SSW involves the presentation of spondees such that the second syllable of the first spondee is dichotically presented with the first syllable of the second spondee. The first syllable of the first spondee and the last syllable of the second spondee are presented in isolation. The listener is asked to repeat everything heard, making this a test of binaural integration. The SSW test has been shown to be sensitive to brainstem and cortical lesions.5 It is relatively quick to administer, and can be used for patients with some degree of peripheral hearing loss, or patients who have less than normal cognitive ability.
- Dichotic Digits: This test involves a dichotic presentation of single digits. Tests of double digits and triple digits are available, but these are actually groups of single digits presented serially. Lists of double or triple digits are not utilized because these would require the patient to rely more heavily on auditory memory. Since the dichotic digits are in fact numbers, they carry less “linguistic load” than do the words used in the SSW. Therefore, the Dichotic Digits test is less susceptible to maturational effects of a corpus callosum that may not yet be fully myelinated, evidenced by a right ear advantage. The Dichotic Digits test has been shown to be sensitive to lesions of the brainstem, auditory cortex and corpus callosum.6 It is a test of binaural integration.
- Time-Compressed Speech at 30% and 60% Compression: This is designed such that the taped stimuli have been digitally sampled and a portion of the acoustic information removed, resulting in a stimulus with altered temporal characteristics but normal frequency characteristics. This test is a monaural low-redundancy task, assessing auditory closure. Time-compressed speech materials have been shown to be sensitive to lesions involving Heschl’s gyrus.7
- Frequency Tone Patterns: The patient hears 30 presentations of three tones that are either 1,122 Hz (high) or 880 Hz (low). The patient is instructed to speak or hum the pattern (high-high-low, low-high-low, etc). This test has a demonstrated sensitivity to lesions of the cerebral hemisphere. Patients who have corpus callosum damage will be able to hum, but not verbalize their responses.
- Duration Tone Patterns: In this test, the patient hears three 1000 Hz tones that are either 250 msec (short) or 500 msec (long) in duration. The patient has to repeat the pattern (long-short-short, short-long-short, etc.). Duration patterns can help diagnose the presence of cerebral lesions.8 Both duration patterns and frequency patterns give the hearing care professional information about the patient’s ability to process prosodic aspects of speech, such as rhythm, intonation, syllabic stress and key word detection.
- Speech with Ipsilateral Speech Noise at SNRs of +10 and 0 dB: Although widely used, this test is not widely standardized. It is used in our clinic as a way to gauge one ear against the other (so-called “binaural interference”).
In addition to the above tests, it is recommended that parents be asked to fill out the CHAPPS (Children’s Auditory Processing Performance Scale), a questionnaire which allows them to compare their child’s auditory performance to children of the same age, considering six different conditions: quiet environment, noise environment, ideal listening conditions, multiple (auditory) inputs, auditory memory and auditory attention span.
Post-Scoring: Now What?
Remediation techniques are based on a three-pronged approach described by Bellis2 which includes skill-building, environmental modifications and use of compensatory strategies when the message is still not perceived. Specific strategies designed to build or improve auditory processes will be examined first.
Skill-Building Exercises
- SSW: Katz11 has devised a scoring paradigm that takes into account both the number of errors (NOE) and response biases (Order Effect, Ear Effect, Reversals and Type A responses) of the patient. Errors outside the limit of those allowed by age are considered significant. Katz identifies four major categories of central auditory processing problems, and suggests specific remediation strategies for each category. The reader is referred to previously published educational materials geared toward clinicians who regularly perform the SSW for this information.11
- Dichotic Digits: Poor scores on the Dichotic Digits test suggest difficulties with binaural integration. These difficulties can be addressed by teaching the patient attending strategies, increasing the signal-to-noise ratio and having the patient undergo a systemized program of speech-in-noise desensitization.
For noise desensitization exercises, we read to the child through the earphones (being careful not to provide visual cues) while they listen to ipsilateral speech noise at a level 10 dB softer than the speech. Reading materials may include parts of their school curriculum, a book they’re reading for fun or sentence materials that match the child’s reading level. The child is then asked questions about the content of the materials. If the child answers all or most of the questions easily, the task can be made more difficult by systematically decreasing the signal-to-noise ratio or reducing the amount of context given. Obviously, storybooks provide more context than sentences, and sentences provide more context than single words.
We also utilize speechreading with all our CAPD clients. After all, if they have trouble processing information through the auditory channel, why not strengthen the visual channel?
Speechreading can be done through a variety of “homemade” materials, including a bingo game where the words are “mouthed” rather than spoken, a “silent scavenger hunt” and identification of “mouthed” nursery rhymes. In addition, we use standard speechreading exercises such as modeling placement of articulators with a mirror. The parent is instructed to help the child practice at home.
- Time-Compressed Speech: Poor scores with time-compressed speech signify difficulty with auditory closure. Remediation includes pre-teaching new concepts and vocabulary, providing written outlines or study notes before the lecture, use of a tape-recorder for meetings or lectures, speechreading, teaching prefixes, suffixes and word roots, and use of large-group FM systems to maximize the signal to noise ratio for individuals. To teach them to build on context, we may provide “silly sentences” where one word does not make sense (e.g., “Do you want jam on your roast?”). This gives the child practice “mis-hearing” the actual utterance and using context to self-correct.
- Frequency Tone Patterns and Duration Tone Patterns: Children who have difficulty recognizing “high” versus “low” and “long” versus “short” tones may have difficulty with temporal patterning. To improve this, a variety of exercises is used. One way to start is by having the child clap or repeat back increasingly difficult rhythmic patterns.
Another goal is to get the child in the habit of recognizing the key word and the emotional tone of a sentence. For example, we may begin having the child identify the stressed word in the sentence, “I can’t believe he did that!” At this stage, the child is simply telling us which word was louder or otherwise “stood out” in the sentence. After reaching a certain level of proficiency at this task, we might ask the child to interpret the sentence (e.g., “He did something amazing; no one can believe it”). Then we say the exact same words, but change the stressed word and the intonation (“I can’t believe he did that”). The child is asked first to identify the stressed word and then to explain how the change in stress and tone changed the meaning of the sentence (“He did something even after he was told not to. Boy, is he in trouble!”).
- Speech with Ipsilateral Speech Noise at SNRs of +10 and 0 dB: Difficulties with speech in noise lend themselves to remediation through noise desensitization as previously described.
Environmental Modifications
A list of environmental modifications may be what audiologists and educators are most familiar with when it comes to recommendations for CAPD. Multiple versions of these lists are in use in every major city of the U.S. They include recommendations that would benefit virtually any child, but are particularly important for children with CAPD: provide preferential seating (toward sound source and away from noise sources); attempt to reduce reverberation in the room with sound-absorbing materials; gain the child’s attention by calling his name or tapping him on the shoulder before addressing him; make sure the room lighting is adequate; check frequently for auditory comprehension; break up complicated or multi-step directions into smaller steps, and rephrase or repeat misunderstood information. Use of FM systems in educational settings is increasing and is very beneficial for many kids with CAPD, providing attenuated headsets are used to avoid overamplifying these normally-hearing children.
Compensatory Strategies
For each child who is presented to us for CAP remediation, several sessions are devoted to learning compensatory strategies. Many of our strategies originated with more standard aural rehabilitation programs geared toward hearing-impaired individuals. The focus of these sessions is preparing for difficult situations.
Role-playing is often used to simulate difficult listening environments. For example, when the teacher is speaking at the same time he or she is writing on the board, children are unlikely to say, “Excuse me, but I didn’t hear you after you turned” unless given polite ways to do it and lots of practice!
Children and parents are also asked to think of successful communication situations and to write down (or dictate to us) exactly what made it successful. Who was there? What was the topic of conversation? Where did it take place? What kind of rules were used concerning conversational “turn-taking”? How can the specifics of this situation be generalized to other listening environments?
A favorite activity is “15 Possible Solutions,” modified from a guide for improving the communication of adult cochlear implant users.12 In this activity, a recent communication event that was not successful is targeted. Then, as many “solutions” as possible are brainstormed and written down as a reference for the child in the future.
Finally, we reinforce realistic expectations. It is important for children to know that no one hears everything all the time. It is also important for them to take responsibility for getting assignments and completing them on time, avoiding the temptation of using CAPD as an excuse for doing less than their best.
Although the specifics regarding the role of other professionals in CAP remediation have not been covered here, it goes without saying that parents, teachers, speech-language pathologists, psychologists and neurologists are often partners in the management of the effects of a CAPD on any given individual. It is only through a sense of mutual respect and professional cooperation that any treatment plan for patients can be optimized.
Summary
Individuals with CAPD comprise a heterogeneous group who are best defined by their strengths and weaknesses with the various processes that contribute to auditory learning. These relative strengths and weaknesses can be determined using a battery of tests with known sensitivity to lesions in various auditory portions of the brain.
Once determined, deficits can be remediated using a three-pronged approach of skill building, environmental modifications and compensatory strategies. Specific techniques to accomplish this were presented and can be incorporated into an individualized intervention program.

References
1. American Speech-Language Hearing Assn. (ASHA): Central auditory processing: Current status of research and implications for clinical practice. Amer Jour Audiol 1996; 5: 2.
2. Bellis J: Assessment and Management of Central Auditory Processing Disorders in the Educational Setting: From Science to Practice. San Diego: Singular Publishing Group, 1996: 32.
3. Keith RW, Rudy J, Donahue PA & Katbamna B: Commparison of SCAN results with other auditory and language measures in a clinical population. Ear and Hear 1989; 10: 382-386.
4. Musiek F, Gollegly KM, Lamb LE & Lamb P: Selected issues in screening for central auditory processing dysfunction. Sem in Hear 1990; 11: 372-384.
5. Katz J: The use of staggered spondaic words for assessing the integrity of the central auditory nervous system. Jour Auditory Res 1962; 2: 227-327.
6. Musiek FE: Assessment of auditory dysfunction: the Dichotic Digits Test revisited. Ear & Hear 1983; 4: 79-83.
7. Mueller HG, Beck WG & Sedge RK: Comparison of the eficiency of cortical level speech tests. Sem in Hear 1987; 8: 279-298.
8. Musiek FE, Baran AJ & Pinheiro ML: Duration pattern recognition in normal subjects and patients with cerbral and cochlear lesions. Audiology 1990; 29: 302-313.
9. McFarland D & Cacace A: Modality specificity as a criterion for diagnosing central auditory processing disorders. Amer Jour Audiol 1995; 4: 36-48.
10. Kraus N, McGee TJ, Ferre J, Hoeppner J, Carrell T, Sharma A & Nicol T: Mismatch negativity in the neurophysiologic/behavioral evaluation of auditory processing deficits: A case study. Ear & Hear 1993; 14: 223-234.
11. Katz J, Smith P & Kurpita B: Categorizing test findings in children referred for auditory processing deficits. SSW Reports 1992; 14: 1-6.
12. Wayner DS & Abrahamson JE: Learning to Hear Again with a Cochlear Implant: An Audiologic Rehabilitation Curriculum Guide. Austin, TX: Hear Again, 1998: 3.8.
Correspondence can be addressed to HR or Barbara Roe Beck, MA, St. Louis Univ., Dept. of Communication Sciences and Disorders, 3660 Vista Ave., St. Louis, MO 63110.