Knowing the auditory, vestibular, and cognitive issues associated with chronic illnesses can help hearing care professionals better treat patients with these conditions.
By Robert M. DiSogra, AuD, and Douglas L. Beck, AuD
Featured image caption: A wide range of chronic illnesses can affect a person’s hearing and cause other problems. For people with asthma, accumulated effects of recurrent hypoxia attacks may result in cochlear dysfunction at higher frequencies. Photo: 33257165 © Alexander Raths | Dreamstime.com
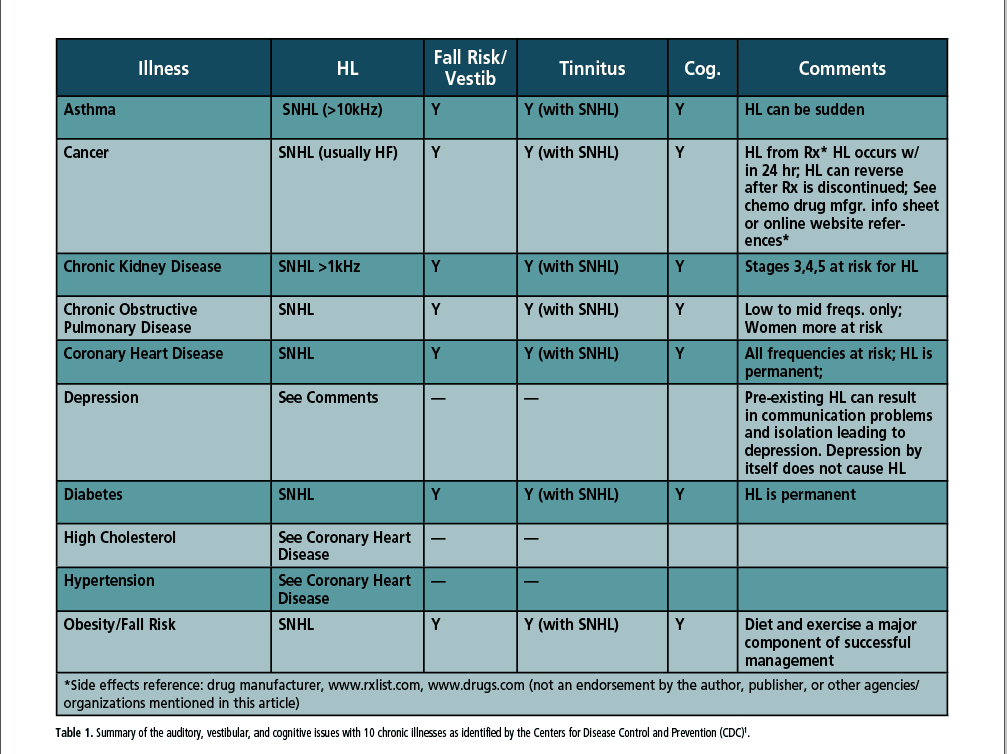
In 2024, the Centers for Disease Control and Prevention (CDC) listed each of the following 10 medical conditions as chronic illnesses: asthma, cancer (excluding skin cancer), chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), coronary heart disease, depression, diabetes, high cholesterol, hypertension, and obesity/fall risk.1,2 (See Table 1.) Hearing loss, tinnitus, and fall risk can be associated with each of these illnesses likely due to ototoxicity, microangiopathy, genetics, and other etiologies. This article examines the risk, type, and degree of auditory-vestibular and cognitive symptoms which may occur in parallel with these chronic illnesses.
The Audiology Project (www.theaudiologyproject.com) was formed in 2016 to promote audiology-based diagnosis and treatment for patients with diabetes or other chronic illness, and the organization continues to work to share this message.3 Familiarity with typical symptoms associated with chronic illnesses can help hearing care professionals know which tests to conduct and how to better manage and treat these patients.
Asthma
According to the Asthma and Allergy Foundation of America, nearly 28 million people in the United States have asthma.4 Asthma affects children and adults. It is a long-term disease that causes airways to become swollen and inflamed, making it difficult to breathe. Although there is no cure for asthma, it can generally be managed and controlled with bronchodilators or steroids.
Because asthma is primarily a pulmonary disorder with generally reversible airway obstruction, the impact of hypoxia (low blood oxygen) may be less than that of other chronic lung diseases. However, the accumulated effects of recurrent hypoxia attacks may potentially result in cochlear dysfunction at higher frequencies (10–20 kHz) in asthma patients, as this frequency range is tonotopically allocated to the basal turn of the cochlea, making it more susceptible to hypoxic injuries.5
Bozek et al noted that although an increased risk of falls in patients with chronic obstructive pulmonary disease (COPD) exists, this has not been conclusively studied in elderly asthmatic patients despite a higher incidence of falls in elderly patients diagnosed with bronchial asthma as compared to subjects with COPD.6
The authors concluded that elderly asthmatic patients presented a high rate of falls, which is comparable to that of patients with COPD.
In a meta-analysis of the effects of asthma on cognition (n = 2,017) the researchers found that cognitive deficits associated with asthma were vast. The strongest associations involved academic achievement and executive functioning and additional impact on processing speed, global intellect, attention, visuospatial functioning, language, learning, and memory.7 Severe asthma was associated with greater cognitive deficits.
Cancer (excluding skin cancer)
Each year, the CDC and the National Cancer Institute (NCI) produce updated U.S. Cancer Statistics data.8 These data are the official federal cancer statistics for the United States and are referred to as U.S. Cancer Statistics, which provide cancer information about the U.S. population. Information about new cancer cases (incidence) comes from CDC’s National Program of Cancer Registries (NPCR) and NCI’s Surveillance, Epidemiology, and End Results (SEER) Program. Information about cancer deaths comes from CDC’s National Center for Health Statistics (NCHS).9
For audiologists, it is important to know that patients with some cancers (i.e., head and neck, lung, testicular, bladder, ovarian) often receive platinum-based chemotherapy. The side effects often include sensorineural hearing loss, tinnitus, and/or vestibular problems). However, the benefits of these drugs often outweigh the side effects. Hearing loss from chemotherapy is usually high frequency, bilateral, and can be short-term or long-term depending on the dosage and duration of the drug. Ototoxicity from cancer medications is well documented.
Cancer and oncology treatments often impact risk factors for falls including muscle weakness, poor balance and proprioception, cognitive impairment and functional disability. Age-related impairments of lower limb neurologic function are commonly exacerbated by neurotoxic chemotherapy, resulting in gait disturbance and balance deficits.10
Chemotherapy-induced cognitive impairment (CICI) spans a variety of prevalent cancers including lung, colorectal, and gynecological.11 As of this writing (December 2024), there are no clinical guidelines for the identification and management of CICI. The applicability of the National Institute on Aging/Alzheimer’s Association criteria for mild cognitive impairment has been successfully applied to patients treated with chemotherapy for breast cancer. The mechanisms by which anticancer therapies may cause cognitive impairment are diverse and heterogeneous.12
Chronic Kidney Disease (CKD)
CKD is a progressive disease with degradation of kidney function over time. Hearing loss, tinnitus, and vertigo are the most common audiologic symptoms in patients with CKD. Of note, there are ultrastructural, immunological, and pathophysiological similarities between the nephron of the kidney and stria vascularis of the cochlea.13
According to the Alport Syndrome Foundation, CKD has five stages based on the glomerular filtration rate (GFR).14 GFR is a measure of how well the kidneys filter blood. The five stages are defined below:
Stage 1: Kidney damage with a normal or increased GFR (≥90)
Stage 2: Kidney damage with a mild decreased GFR (60-89)
Stage 3: Moderate to severe reduction in GFR (30-59)
Stage 4: Severe reduction in GFR (15-29)
Stage 5: Kidney failure (GFR < 15 or dialysis or transplant)
In a 2013 study of 84 CKD patients, hearing loss typically occurred at Stage 3 and higher.15
Elderly individuals with CKD often experience balance problems due to the impact of CKD on the nervous system and muscle function, leading to a higher risk of falls, particularly as CKD progresses to advanced stages, largely because CKD may impact peripheral nerve function, impacting sensory input crucial for maintaining balance.
Patients with CKD have an elevated risk of cognitive decline. Unfortunately, CKD patients are generally not monitored for hearing loss. Pepin et al suggest that kidney function tests should be included in a comprehensive assessment of patients presenting with cognitive impairments, especially in older individuals.16
Chronic Obstructive Pulmonary Disease (COPD)
According to the CDC, chronic obstructive pulmonary disease (COPD) is a group of lung diseases which generally get worse over time. The most common COPD types are emphysema and chronic bronchitis. There is no cure for COPD, but it can be treated. Nearly 16 million U.S. adults have COPD.17
Aarhus, et al followed 12,082 adults over 20 years as part of a population-based cohort study in Norway (the HUNT study) with baseline measurements in 1996 to 1998 and follow-up from 2017 to 2019.18 403 subjects were diagnosed with COPD. Hearing loss (after 20 years) was more prevalent in low to mid frequencies for the entire group, and of note, women seem to be more susceptible to COPD-related hearing loss at higher frequencies. Their findings support the association between COPD and hearing loss. Pure tone audiometry, DPOAEs, and ABR assessments often indicate these same trends.19
In a pilot study, Bozek et al noted that, although an increased risk of falls in patients with chronic obstructive pulmonary disease (COPD) exists, this has not been studied in elderly asthmatic patients.6 All participants were monitored on the following parameters: falls, comorbidities, drug therapy, and The Berg Balance Scale. Over a 12-month period, the authors found a higher incidence of falls in elderly patients diagnosed with bronchial asthma compared to subjects with COPD.
Coronary Artery/Heart Disease
According to the CDC, coronary artery disease (CAD) (including hypertension and high cholesterol levels) is the most common type of heart disease in the United States. CAD is caused by a build-up of plaque inside the walls of arteries which supply blood to the heart.20
Przewoźny, et al reported hearing loss was often found in higher frequencies for people with CAD.21 The authors stated current evidence linking hypertension to sensorineural high-frequency cochlear hearing loss in humans may be confounded by other concomitant diseases or risk factors such as age, coronary artery disease, diabetes, obesity, hyperlipidemia, smoking, and noise exposure.
Balance problems are common in older adults and can be caused by many health conditions. These issues can include inner ear problems, muscle loss, poor circulation, neural degradation, medication side effects, and more.22 A thorough review of the patient’s medical history is needed to determine if a cardiac patient would be at risk for balance problems.
A meta-analysis of four studies (n = 940,771) and six cross-sectional studies (n = 680,349) found stroke, coronary artery disease, and cardiovascular disease (CVD) were strongly associated with hearing loss, although “epidemiological associations remain unclear.”23
van Nieuwkerk, et al, noted cognitive impairment is common in patients with cardiovascular disease.24 One in three patients presenting at cardiology clinics have some degree of cognitive impairment, depending on the cardiac condition, comorbidities, and age. The high prevalence of cognitive impairment in patients with cardiac disease is likely due to shared risk factors indicating the need for a comprehensive audiometric evaluation and appropriate treatment prior to a cognitive screening or assessment.
Depression
As a chronic illness, depression can be the result of hearing loss and social distancing or isolation which often accompanies untreated hearing loss. The American Academy of Audiology (AAA) reports depression and hearing loss are linked25 and hearing loss may be the cause of depression in some people. AAA also notes that hearing loss can lead to decreased social engagement and may contribute to an overall poorer quality of life.
Culpepper et al noted cognitive impairment is a common, often persistent symptom of major depressive disorder (MDD) that is disproportionately represented in patients who have not returned to full psychosocial functioning.26 They note the ultimate goal of treatment of depression is full functional recovery, and assessing patients for cognitive impairment and selecting treatments that address cognitive dysfunction should lead to improved functional outcomes. Such treatment often includes antidepressants, cognitive-behavioral therapy, and exercise.
Diabetes
Statistics from the American Diabetes Association (ADA) website indicate more than 38 million people in the United States have diabetes.27 Also, of the nearly 98 million adults in the United States who have prediabetes, the rate of hearing loss is 30% higher than in those with normal blood glucose (blood sugar).
In diabetic patients, microangiopathy (damage to small blood vessels) often occurs. Microangiopathy of the eye is called retinopathy and in the kidney it is called nephropathy. The cause of microangiopathy appears to be a build-up of sugar-based substances on the attenuated vessel walls, thereby reducing blood flow throughout the body. In the ear the impact of microangiopathy is found in the stria vascularis and spiral ligament.28
Diabetic retinopathy can be an indicator of microangiopathy in the ear since the vascularization of both senses is similar. As visual problems reduce a person’s mobility and increase fall risk, a person with diabetes (PWD) will often seek help for their visual impairment sooner than their hearing impairment because the hearing impairment does not impair mobility.
Hearing loss from diabetes is sensorineural and may impact all frequencies, depending on the duration and degree of diabetes. Low blood glucose levels may also affect balance, which places some PWDs at risk for falls.
In 2022, The Audiology Project successfully contributed to the CDC’s recognition of audiology as one of five key professions with whom a PWD should have an ongoing relationship. The other four professions are pharmacy, podiatry, optometry, and dentistry.29
The goal of The Audiology Project is to bring greater awareness to PWDs and their professional caregivers of the importance of comprehensive audiometric evaluation and treatment.30 See NOTE at the end of this section to learn more about diabetes educators.
PWDs have an increased risk of falling due to complications such as peripheral neuropathy which can affect balance and sensation, leading to instability and a higher likelihood of falls; other factors include poor vision, autonomic neuropathy causing postural hypotension, and fluctuations in blood sugar levels, as occurs with hypoglycemia.31
Cognitive deficits may occur at early stages of diabetes and are further exacerbated by the metabolic syndrome. The duration of diabetes and glycemic control may have an impact on the type and severity of cognitive impairment. Both type 1 (T1DM) and type 2 diabetes mellitus (T2DM) have been associated with reduced performance on multiple domains of cognitive function and with evidence of abnormal structural and functional brain magnetic resonance imaging (fMRI).32 Again, a hearing assessment (including an auditory processing evaluation) should be completed prior to a cognitive screening.
NOTE: Diabetes Education and Care – Diabetes educators are usually the first professionals a PWD will see after the diagnosis. The Association of Diabetes Care & Education Specialists (www.adces.org) is solely dedicated to diabetes care and education for patients with diabetes.33 Diabetes educators can be found at local hospitals or medical centers. See also the American Association of Clinical Endocrinology (AACE) (www.aace.com) and the American Diabetes Association (www.diabetes.org) for additional patient management.
High Cholesterol – see Coronary Heart Disease
Hypertension – see Coronary Heart Disease
Obesity
The World Health Organization identifies obesity (having a body-mass-index—BMI—of 30 or higher) as a chronic complex disease defined by excessive fat deposits which may impair health and may lead to increased risk of type 2 diabetes and heart disease (see Coronary Heart Disease).34 Obesity is also a major factor that can affect quality of life for many people.
In a Japanese study, the authors concluded that being overweight and obesity are associated with an increased risk of hearing loss, and metabolically unhealthy obesity may confer additional risks,35 such as falls.34
In another study, Nguyen et al found that obesity can increase the risk of developing mild cognitive impairment in the form of short-term memory and executive function deficits, as well as dementia and Alzheimer’s disease.36
A 2008 study evaluated the influence of obesity on falls and quality of life.37 The obese group had almost twice as many falls and stumbling events as the normal weight group. The authors concluded that in middle-aged and older adults, obesity was associated with a higher prevalence of falls and stumbling during ambulation.
Conclusion
Hearing loss, tinnitus, vestibular problems, fall risk, and cognitive issues often occur across the 10 chronic illnesses identified by the CDC. The onset, type, and degree of the hearing loss varies widely from patient to patient often due to comorbidities and other pre-existing and often undiagnosed auditory-vestibular problems.
Nonetheless, in the presence of chronic illness, we recommend comprehensive audiometric evaluations in accordance with AAA and ASHA Best Practice statements, with additional tinnitus, balance, cognitive, and other assessments as indicated, to assure proper and early diagnosis, and appropriate and patient-centered treatment as soon as possible, to preserve and enhance quality of life for the patient.
Robert M. DiSogra, AuD, is an audiology consultant in Millstone, NJ. He is a board member of The Audiology Project, a non-profit organization that promotes audiology-based diagnosis and treatment for patients with diabetes or other chronic illness (www.theaudiologyproject.com). He was the 2020 recipient of the Clinical Excellence in Audiology Award from the American Academy of Audiology.
Douglas L. Beck, AuD, is an author, consultant, peer-reviewer, lecturer, clinician, and academic. He is an adjunct clinical professor of Communication Disorders & Sciences at State University of New York at Buffaloand a host of the Hearing Matters Podcast. He is also the author of The Consumer’s Guide to Hearing Care (2024) and the winner of the 2024 AIHHP Award for Outstanding Services to Audiology.
References
1. Centers for Disease Control and Prevention (CDC) (2024). Chronic Illness. (www.cdc.gov). Accessed online November 18, 2024
2. Benavidez GA, Zahnd WE, Hung P, Eberth JM. (2024). Chronic disease prevalence in the US: Sociodemographic and Geographic Variations by Zip Code Tabulation Area. Prev Chronic Dis. 2024;21:E14. Published 2024 Feb 29. doi:10.5888/pcd21.230267
3. The Audiology Project. 2024. www.theaudiologyproject.com
4. Asthma and Allergy Foundation of America. 2024. Asthma. www.aafa.org
5. Rauch SD. Clinical practice. Idiopathic sudden sensorineural hearing loss. N Engl J Med. 2008;359(8):833-840. doi:10.1056/NEJMcp0802129
6. Bozek A, Jarzab J, Hadas E, Jakalski M, Canonica GW. Fall episodes in elderly patients with asthma and COPD – A pilot study. J Asthma. 2019;56(6):627-631. doi:10.1080/02770903.2018.1474365
7. Irani F, Barbone JM, Beausoleil J, Gerald L. Is asthma associated with cognitive impairments? A meta-analytic review. J Clin Exp Neuropsychol. 2017;39(10):965-978. doi:10.1080/13803395.2017.1288802
8. Centers for Disease Control and Prevention. 2024. Highlights from 2021 cancer incidence with comparisons to previous years. (www.cdc.gov/united-states-cancer-statistics/publications/uscs-highlights.html)
9. National Center for Health Statistics. NHIS* Adult Summary Health Statistics. Data accessed October 7, 2024. Available from https://data.cdc.gov/d/25m4-6qqq *National Health Interview Survey
10. Morris R, Lewis A. Falls and Cancer. Clin Oncol (R Coll Radiol). 2020;32(9):569-578. doi:10.1016/j.clon.2020.03.011
11. Fleming B, Edison P, Kenny L. Cognitive impairment after cancer treatment: mechanisms, clinical characterization, and management. BMJ. 2023;380:e071726. Published 2023 Mar 15. doi:10.1136/bmj-2022-071726
12. Gifford AR, Lawrence JA, Baker LD, et al. National Institute on Aging /Alzheimer’s Association criteria for Mild Cognitive Impairment applied to chemotherapy treated breast cancer survivors. J Oncol Research. 2017;1(1):101.
13. Arnold W. Inner ear and renal diseases. Ann Otol Rhinol Laryngol Suppl. 1984;112:119-124. doi:10.1177/00034894840930s420
14. Alport Syndrome Foundation. 2024. Stages of kidney disease. https://alportsyndrome.org.
Accessed online November 24, 2024
15. Peyvandi A, Roozbahany NA. Hearing loss in chronic renal failure patient undergoing hemodialysis. Indian J Otolaryngol Head Neck Surg. 2013;65(Suppl 3):537-540. doi:10.1007/s12070-011-0454-9
16. Pépin M, Klimkowicz-Mrowiec A, Godefroy O, et al. Cognitive disorders in patients with chronic kidney disease: Approaches to prevention and treatment. Eur J Neurol. 2023;30(9):2899-2911. doi:10.1111/ene.15928
17. Centers for Disease Control and Prevention (CDC). 2024. About COPD. (www.cdc.gov/copd/about/index.html#cdc_disease_basics_overview-what-it-is). Accessed online November 24, 2024
18. Aarhus L, Sand M, Engdahl B. COPD and 20-year hearing decline: The HUNT cohort study. Respir Med. 2023;212:107221. doi:10.1016/j.rmed.2023.107221
19. el-Kady MA, Durrant JD, Tawfik S, Abdel-Ghany S, Moussa AM. Study of auditory function in patients with chronic obstructive pulmonary diseases. Hear Res. 2006;212(1-2):109-116. doi:10.1016/j.heares.2005.05.018
20. Centers for Disease Control and Prevention (CDC). 2024. About coronary artery disease (CAD). www.cdc.gov/heart-disease/about/coronary-artery-disease.html. Accessed online November 24, 2024
21. Przewoźny T, Gójska-Grymajło A, Kwarciany M, Gąsecki D, Narkiewicz K. Hypertension and cochlear hearing loss. Blood Press. 2015;24(4):199-205. doi:10.3109/08037051.2015.1049466
22. National Institutes of Health, National Institute on Aging. 2024. Older adults and balance problems. Accessed online (www.nia.nih.gov/health/falls-and-falls-prevention/older-adults-and-balance-problems#symptoms-of-balance-disorders)
23. Tan CJ, Koh JWT, Tan BKJ, et al. Association Between Hearing Loss and Cardiovascular Disease: A Meta-analysis. Otolaryngol Head Neck Surg. 2024;170(3):694-707. doi:10.1002/ohn.599
24. van Nieuwkerk AC, Delewi R, Wolters FJ, et al. Cognitive Impairment in Patients With Cardiac Disease: Implications for Clinical Practice. Stroke. 2023;54(8):2181-2191. doi:10.1161/STROKEAHA.123.040499
25. American Academy of Audiology (AAA). 2024. Depression and hearing loss. Accessed online November 28, 2024
26. Culpepper L, Lam RW, McIntyre RS. Cognitive Impairment in Patients With Depression: Awareness, Assessment, and Management. J Clin Psychiatry. 2017;78(9):1383-1394. doi:10.4088/JCP.tk16043ah5c
27. American Diabetes Association (ADA) 2024. Diabetes and hearing loss. www.diabetes.org/about-diabetes/complications/hearing-loss/diabetes-and-hearing-loss. Accessed online November 28, 2024
28. Fukushima H, Cureoglu S, Schachern PA, Paparella MM, Harada T, Oktay MF. Effects of type 2 diabetes mellitus on cochlear structure in humans. Arch Otolaryngol Head Neck Surg. 2006;132(9):934-938. doi:10.1001/archotol.132.9.934
29. Centers for Disease Control and Prevention (CDC). Hearing loss. www.cdc.gov/diabetes/diabetes-complications/diabetes-and-hearing-loss.html. Accessed online November 24, 2024
30. The Audiology Project. 2024. Educational Materials (www.theaudiologyproject.com/education-materials). Accessed online November 24, 2024
31. Freire LB, Brasil-Neto JP, da Silva ML, et al. Risk factors for falls in older adults with diabetes mellitus: systematic review and meta-analysis. BMC Geriatr. 2024;24(1):201. Published 2024 Feb 28. doi:10.1186/s12877-024-04668-0
32. Zilliox LA, Chadrasekaran K, Kwan JY, Russell JW. Diabetes and Cognitive Impairment. Curr Diab Rep. 2016;16(9):87. doi:10.1007/s11892-016-0775-x
33. Association of Diabetes Care & Education Specialists (www.adces.org)
34. World Health Organization. Obesity and overweight. www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed online November 24, 2024
35. Hu H, Tomita K, Kuwahara K, et al. Obesity and risk of hearing loss: A prospective cohort study. Clin Nutr. 2020;39(3):870-875. doi:10.1016/j.clnu.2019.03.020
36. Nguyen JC, Killcross AS, Jenkins TA. Obesity and cognitive decline: role of inflammation and vascular changes. Front Neurosci. 2014;8:375. Published 2014 Nov 19. doi:10.3389/fnins.2014.00375
37. Fjeldstad C, Fjeldstad AS, Acree LS, Nickel KJ, Gardner AW. The influence of obesity on falls and quality of life. Dyn Med. 2008;7:4. Published 2008 Feb 27. doi:10.1186/1476-5918-7-4
Additional Resource: National Library of Medicine (NLM), PubMed (selected topics)





