Converting dBHL to dBSPL is an important step when using instant-fit tips/domes
In-situ audiometry has been shown to be both efficient and effective. However, this study suggests that—due to low-frequency energy leakage from the ear canal—in-situ conduction thresholds measured in dBHL with instant-fit tips show significantly higher degrees of low-frequency hearing loss than conventionally measured thresholds. Therefore, in clinical use, either the fitting software or the clinician should make the necessary conversions to ensure that averaged or individually measured REDD correction figures are applied to in-situ threshold requirements.
Many hearing aids are equipped with an onboard tone generator that frequently is used to guide the hearing aid wearer through program changes and to alert them when the battery is running low. In a few cases, manufacturers provide the software module required to use the onboard tone generator as an audiometer to measure hearing thresholds through the hearing aid and the selected coupling to the ear.1,2
Hearing assessments conducted via a hearing aid are generically termed in-situ audiometry.3,4 In-situ audiometry is attractive because it requires less equipment and resources, and may save on clinical time used when transferring threshold data between different test modules. One serious downfall is that in-situ audiometry is currently limited to measurements of air conduction thresholds. The cost-saving potential of using in-situ audiometry for assessment, however, means that hearing services could be provided to non-complex cases in areas where they are currently limited by remoteness of location or economic disadvantage.
Previous work has concluded that the test-retest reliability of in-situ thresholds measured on normal-hearing listeners was equivalent to that of conventional audiometric procedures.5 It has further been reported that in-situ thresholds were within 5-10 dB of conventional thresholds measured on children with moderately severe hearing loss.6
In a recent study conducted at the National Acoustic Laboratories (NAL), the validity and reliability of in-situ air conduction thresholds measured on hearing-impaired listeners were explored further.7 This was done by comparing thresholds measured through a hearing aid coupled to the ear using the newer style closed and open instant-fit tips with thresholds measured conventionally using insert earphones. It was found that the in-situ thresholds, measured in dBHL, varied significantly from the conventionally measured thresholds due to low-frequency energy leaking from the ear canal.
However, the in-situ measurements were found to be as reliable and valid as conventional methods after transducer and coupling specific real-ear to dial difference (REDD) values were applied to convert threshold levels from dBHL to dBSPL at the eardrum. Without the correction, low-frequency leakage from the open instant-fit tip resulted in significantly higher average threshold levels of 29, 23, 13, and 10 dB at 250, 500, 1000, and 1500 Hz, respectively, relative to the conventionally measured thresholds.
Such differences in dBHL are assumed to result in fitting results so different that it would severely affect the auditory experience with the hearing aid. Therefore, average or individually measured REDD values must be applied to in-situ thresholds before extracting target if they are measured with an open instant-fit tip.
There was also a significant loss of low-frequency energy from the closed instant-fit tip. The loss was, in this case, limited to 250 and 500 Hz, and amounted to an average of 9 and 7 dB, respectively. At higher frequencies, in-situ thresholds measured with the closed instant-fit tip were, on average, within 2 dB of the conventionally measured thresholds. In this case, it was less clear to what extent the fitting error introduced by using an uncorrected in-situ threshold would affect perception.
As a result, following on from the main study, the investigation reported in this paper addressed the following two questions:
1) For what proportion of the study participants did the NAL-NL1 targets derived from the conventionally measured dBHL threshold values and the uncorrected in-situ threshold values obtained with the closed instant-fit tip differ significantly?
2) For the cases where there was a significant difference in target, was the difference perceptually noticeable by the hearing aid wearer in a range of common listening situations?

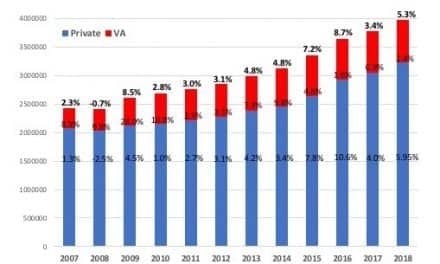
FIGURE 1. Participants’ average threshold in dB HL. For clarity, thresholds for right and left ears are shown shifted. Whiskers indicate ± 1 standard deviation.
Methodology
A total of 24 hearing-impaired volunteers ages 43 to 82 years (mean age: 73 years) completed the main study during which their thresholds were measured in a conventional way using insert earphones, and in-situ through a hearing aid coupled to a closed and an open instant-fit tip. Figure 1 shows the participants’ average thresholds measured at the beginning of the study using insert earphones.
The hearing aids used for the in-situ measurements were Siemens’ Centra HP behind-the-ear (BTE) devices. Custom software was developed to enable presentation of puretones of 1-second duration in 1.5 dB steps through this device. To save time and reduce participant fatigue, all testing after the initial “full” audiogram was performed unilaterally. The left ear was selected for odd-numbered participants and the right ear for even-numbered participants. Full details of the main study can be found in the recently published article by O’Brien et al.7
After the main study, NAL-NL1 targets for 50, 65, and 80 dBSPL inputs were calculated for both the conventional (“insert”) and in-situ with closed instant-fit tip (“in-situ closed”) uncorrected audiograms using the NAL-NL1 stand-alone software (v1.40). Targets that differed by more than 3 dB RMS (root mean square, a measure of the long-term overall level of the signal) across all frequencies at any input level, or by more than 10 dB at a single frequency, were considered to be significantly different from each other in that we expected they would provide the hearing aid user with different listening experiences.
Participants for whom the targets were found to be sufficiently different according to the above criteria were invited to return for another appointment to listen to a hearing aid adjusted to each set of targets. At this appointment, a hearing aid was fit to the two NAL-NL1 targets minus 3 dB (an anticipated modification for NAL-NL2) and the responses saved into two program memories of the Centra HP BTE hearing aid. The device was coupled to the participant’s test ear using the closed instant-fit tip. Real-ear insertion gain (REIG) measurements, using a broadband speech-weighted noise presented at 50, 65, and 80 dBSPL, were used to verify the fittings.
Paired comparison testing involved presenting short segments of speech in quiet, speech in babble-noise (+5 dB SNR), and classical music at 60, 65, and 70 dBSPL Leq, respectively, from a loudspeaker in the free field. Each stimulus was presented three times, using an “odd one out” paradigm in which the “insert”-based program was presented twice and the “in-situ closed”-based program once, in an order that was balanced across participants and stimuli.

FIGURE 2. Difference between conventional insert and in-situ closed based NAL-NL1 targets for 50 dBSPL input. Blue lines represent participants for whom the differences were within 3 dB RMS, and red lines represent the eight participants for whom the differences exceeded 3 dB RMS.

FIGURE 3. The percentage of time the two responses were audibly different from each other when listening to each of three stimuli.
Activation of the programs was controlled by the experimenter via the Connexx software. For each trial, the forced-choice task of the listener was to decide which of the three presentations was different to the other two. They were also asked to rate how different (very different, moderately different, slightly different, not at all different) their chosen program was. Each participant made 30 comparisons (3 stimuli x 10 repetitions).
Results
Of the 24 participants who completed the main study, the difference in threshold measurements averaged across 250 Hz and 500 Hz obtained under the “insert” and “in-situ closed” conditions exceeded 10 dB for nine (Figure 2). For eight of these listeners, the difference in NAL-NL1 prescribed targets for the two uncorrected thresholds exceeded 3 dB RMS. For seven of these listeners, the difference was seen at all three input levels. The one listener with a difference in threshold measurements of more than 10 dB, but little difference in prescribed target, had normal hearing across the low frequencies as measured with insert earphones, and therefore the low frequency gain prescribed on the basis of the two threshold measures was minimal.
The negative difference values in Figure 2 indicate that in-situ thresholds measured with the closed instant-fit tip generally called for higher prescribed gain than did the conventionally measured thresholds. Not surprisingly, the main difference in targets was seen across the low frequencies, especially around 250 and 500 Hz, where the greatest deviation in thresholds was evident.
Seven of the eight participants for whom different targets were prescribed based on the two sets of threshold measurement agreed to come back for another appointment during which they completed the paired comparison test. Figure 3 shows the percentage of times the participants were able to correctly identify the “in-situ closed” program as being different to the “insert” program for each stimulus. It can be seen that, irrespective of the stimulus, the participants correctly identified the odd one out of three on a fairly consistent basis. Consequently, it may be concluded that the two responses were generally perceptually different.
According to the binomial distribution, the perceptual difference between the two responses is considered significant if the “in-situ closed” response is correctly identified in at least 9 out of 10 presentations. The shaded cells in Table 1 show when there was a significant perceptual difference between responses for each participant and stimulus. It can be seen that the responses were significantly different across all stimuli for three participants, while this was the case for only one stimulus each for two participants.

TABLE 1. The average difference strength between the two responses by participant and stimulus (max = 4.0). Shaded cells indicate cases for which the two responses were deemed significantly different from each other.
The number in the cells in Table 1 refers to the average strength of the perceived difference. Four, three, and two points were allocated to the identification, if the “in-situ closed” response was found to be very different, moderately different, or slightly different from the “insert” response, respectively. On this basis, the two responses were considered between slightly (2.0) and moderately (3.0) different for each stimulus for all but two participants (4 and 5).
Summary
Research has shown in-situ audiometry to be efficient and effective. However, in-situ air conduction thresholds measured in dBHL with open and closed instant-fit tips show significantly higher degrees of low-frequency hearing loss than conventionally measured thresholds due to leakage of low-frequency energy from the ear canal.7 Even though the low-frequency leakage from the closed tip was significantly less than that observed from the open tip, data presented in this paper suggest that the resulting shift in threshold can result in a target that is increased by more than 3 dB RMS from actual target for about one-third of hearing aid users with mild or moderate hearing loss. For at least two-thirds of these users, the difference in prescription will affect the auditory experience with the hearing aid.
Therefore, in terms of clinical use, the necessary steps should be taken to ensure that average or individually measured REDD correction figures are applied to in-situ threshold measurements by the manufacturer or by the clinician. The average correction factors would depend on the calibration of the transducer and the selected coupling to the ear.
References
- Ludvigsen C, Topholm J. Fitting a wide range compression hearing instrument using real ear threshold data: a new strategy. In: Kochkin S, Strom KE, eds. High Performance Hearing Solutions (Vol 2). Hearing Review. 1997;(Suppl)4(11):37-39.
- Bostock S, Reber M, Scheller L. In situ audiometry and open fitting: can venting affect test results? Audiology Insight. 2004;2:26-31.
- Kiessling J. In situ audiometry (ISA): a new frontier in hearing aid selection. Hear Instrum. 1987;38(1):28-29.
- Valente M, Potts LG, Valente M. Differences and intersubject variability of loudness discomfort levels measured in sound pressure level and hearing level for TDH-509P and ER-3A earphones. J Am Acad Audiol. 1997;8:59-67.
- Smith-Olinde L, Nicholson N, Chivers C, Highley P. Test-retest reliability of in situ unaided thresholds in adults. Am J Audiol. 2006;15:75-80.
- Winter M, Kuk F. Using a DSP instrument fitting protocol for pediatric cases. Hearing Review. 1998;15(10):27-28, 71-73.
- O’Brien A, Keidser G, Yeend I, Hartley L, Dillon H. Validity and reliability of in-situ air conduction thresholds measured through hearing aids coupled to closed and open instant-fit tips. Int J Audiol. 2010;49(12):868-876.
Correspondence can be addressed to HR or Gitte Keidser, PhD, at .
Citation for this article:
Keidser G, Yeend I, O’Brien A, Hartley L. Using in-situ audiometry more effectively: How low-frequency leakage can effect prescribed gain and perception. Hearing Review. 2011;18(3):12-16.