Dear Editor:
I found the article, “A Perspective on the Indiana University OTC Outcome Study,”1 by John Tecca, PhD, in the July edition of The Hearing Review to be timely and interesting. I appreciate the many positive comments he had about our recently published research2 on hearing aid service delivery models, and our summary article3 in the June edition of HR. This brief response just serves to address some of the concerns expressed by Dr Tecca in his article, especially pertaining to his comments regarding the various study limitations we noted in our report.
Regarding the demographics of the subjects in our study, it is the case, as noted in that original report and by Dr Tecca in his article, that the study sample was highly educated compared to the US population of older adults. According to the 2015 US Census Bureau, the population demographics for our study in Bloomington, Ind, are actually quite similar to those of Portage, Mich, the location of Dr Tecca’s practice. Moreover, the demographics of our study sample differ from those of the Bloomington, Ind, community in general. I suspect that the sources for such differences may be attributable to at least two factors. First, it is known that first-time hearing aid wearers tend to have higher education levels than those who do not adopt hearing aids.4 Second, some of this difference in demographics between our study sample and the general community, especially regarding level of education, may be due to the recruitment of participants via newspaper and community ads in which subjects were invited to participate in an NIH-funded clinical trial of hearing aids. Participation in such a trial might be particularly attractive to a well-read, highly educated audience. There is evidence that among older adults, volunteers for clinical trials are more highly educated than non-participants in such trials.5 Both factors noted above, however, are just speculation. Nonetheless, as noted in our article and reiterated by Dr Tecca, these demographics must be kept in mind when evaluating the viability of the specific consumer-decides (CD) service-delivery model we used before broader application to the general population of older Americans.
Next, Dr Tecca speculates that actual OTC devices will be quite different from the high-quality hearing aids used for all subjects in our study. He further states that contemporary PSAPs will be more representative of future OTC devices. I believe that a wide range of devices and service-delivery models will co-exist when the OTC devices are approved, but this too is just speculation. If OTC devices become a reality, only then will we have a clearer idea regarding the nature of these devices.
Dr Tecca also questions whether the audiology-based (AB) best practices group in our study truly received best practices, as there were no follow-up sessions during the 6-week trial. He quotes a statement in our publication pertaining to “true best practices” and the need for inclusion of follow-up sessions. Although the quotation is accurate as quoted by Dr Tecca, in the context of the sentences both preceding and following the quote, a different interpretation is revealed. Specifically, we were not endorsing follow-up visits as a part of best practices, as might be inferred from the quotation of this lone sentence from our article. When the AB participants were offered an additional 4 weeks of trial after adjustment of their hearing aids, only 4 of 53 opted to do so (5 returned their hearing aids and 44 were content with them as they were). Rather, as noted in the subsequent sentence in our article, practice guidelines for hearing aid delivery in adults from both ASHA and AAA do not include follow-up during the trial period as a part of best practices. Moreover, it is important to note, as was noted in our article, that even some of the best-practices elements recommended by ASHA and AAA and incorporated into our study protocol—such as real-ear measures for verification of fit—are known not to be “common practices.”6
Next, Dr Tecca suggests that the observation in our study that 88% of participants had twisted or kinked tubing is an “astounding” observation and that inclusion of follow-up visits would remedy this problem. I suspect this high prevalence, however, was simply due to a very rigorous physical inspection of the devices and a low criterion for noting any physical abnormalities in the devices when worn. I know of no other reports of the frequency of such observations to which we can compare these findings. I also doubt that the minor twists in tubing observed would lead to any functional consequences, but that is speculation on our part. All we know, and reported, was that the combined effects of all abnormalities noted during the physical inspections in the as-worn state of the hearing aids, including cerumen occlusion, weak or dead batteries, etc, resulted in slightly but significantly-reduced performance with the hearing aids. Reduced “as worn” gain and patient performance at follow-up, however, is a common observation even when best practices have been followed.7-9
Dr Tecca also suggests that this lack of follow-up may be why we had a 19% return for credit (RFC) rate. He notes that recent HIA data suggest that this is about average for the industry, but audiology best practices including follow-up visits would produce lower RFC rates. He cites his practice’s excellent RFC rate of 2.1% as an illustration. This is truly excellent and this, together with other outcomes for Dr Tecca’s practice provided in his report, clearly illustrate that his practice provides outstanding hearing aid services to his patients. However, given the industry average RFC rate cited by Dr Tecca of 20% and the fact that most hearing aids are delivered by audiologists, for every practice with a RFC rate of 2.1% such as his, there must be others that are closer to 30-35%. It should also be noted that the actual RFC rate for our study, as reported in the publication, was 5 of 53 for the AB group or about 9%. Clearly, not as good as Dr Tecca’s practice, but also considerably better than the industry average.
Again, I appreciate Dr Tecca’s many positive comments about our research. I also laud him for having an exemplary practice with outstanding outcomes. I look forward to continued discussions about a variety of options for service provision to the millions of older Americans with hearing loss, only about 20% of whom are currently being served by existing service-delivery models.
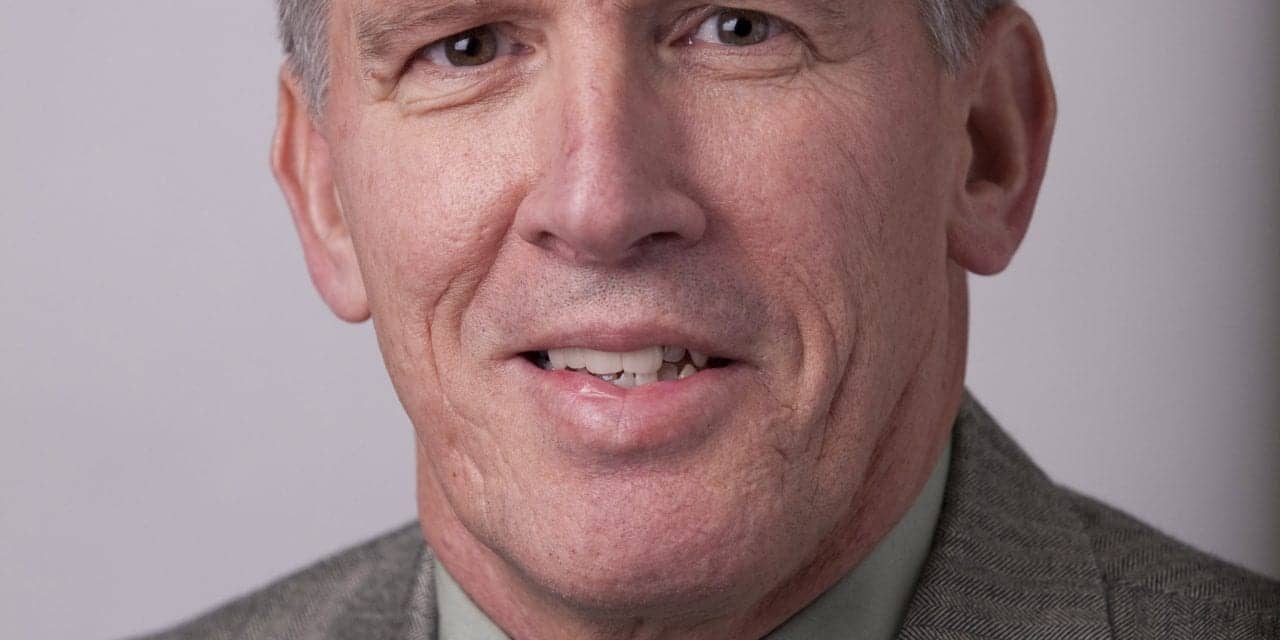
— Larry Humes, PhD, Indiana University
References
-
Tecca JE. A perspective on the Indiana University OTC outcome study. Hearing Review. 2017;24(7):18-24.
-
Humes LE, Rogers SE, Quigley TM, Main AK, Kinney DL, Herring C. The effects of service-delivery model and purchase price on hearing–aid outcomes in older adults: A randomized double-blind placebo-controlled clinical trial. Am J Audiol. 2017; 26: 53-79.
-
Humes LE, Rogers SE, Quigley TM, Main AK, Kinney DL, Herring C. The effectiveness of two service-delivery models in older adults: A randomized double-blind placebo-controlled clinical trial. Hearing Review. 2017;24(5);12-19.
-
Fischer ME, Cruickshanks KJ, Wiley TL, Klein BEK, Klein R, Tweed TS. Determinants of hearing aid acquisition in older adults. Am J Public Health. 2011;101, 1449-1455.
-
Martinson BC, Crain AL, Sherwood NE, Hayes MG, Pronk NP, O’Connor PJ. Population reach and recruitment bias in a maintenance RCT in physically active older adults. J Phys Activity Health. 2010;7:127-135.
-
Mueller HG, Picou EM. Survey examines popularity of real-ear probe-microphone measures. Hear Jour. 2010;63(5):27-32.
-
Humes LE, Barlow NN, Garner CB, Wilson DL. Prescribed clinician-fit versus as-worn coupler gain in a group of elderly hearing aid wearers. J Speech Lang Hear Res. 2000;43:879-892.
-
Peek BF, Rosenfeld MAL, Bratt GW, Williams DW. NIDCD/VA hearing aid clinical trial and follow-up: Coupler and real-ear measurement. J Amer Acad Audiol. 2007;18:282-291
-
Boymans M, Dreschler WA. Audiologist-driven versus patient-driven fine tuning of hearing instruments. Trends Amplif. 2012;16, 49-58.