Researchers at UC Davis School of Medicine have for the first time shown that a polysialylated glycoprotein that regulates neurodevelopment exists on the surface of cells in the adult inner ear. This biomarker of early cells allows researchers to identify immature cells so that they can be used for further research and possible treatment. The research, published online in the May 17 edition of Biochemical and Biophysical Research Communications, opens the door to developing stem cell replacement treatments in the inner ear to treat certain hearing disorders.
“Hearing loss is a complex process and is usually regarded as irreversible,” said Frederic A. Troy II, principal investigator of the study and professor emeritus of biochemistry and molecular medicine, and a member of the UC Davis Comprehensive Cancer Center. “Finding this molecule in the inner ear that is known to be associated with early development may change that view.”
Having a biomarker for immature stem cells could make it possible to isolate neural stem cells from the adult inner ear in a person with hearing loss, induce their replication and maturation in the laboratory, and then re-introduce them back into the inner ear as functioning neurons. It is postulated that they may recolonize and establish themselves, thereby improving hearing.
During development, certain glycoproteins (carbohydrate-protein linked molecules) that are expressed on cell surfaces serve critical functions essential to the normal growth and organization of the brain. One member of the class of cell-surface glycoproteins is an unusual molecule called polysialic acid (polySia). Its large size fills up spaces between cells and its strong electric charge repels other molecules—qualities that help to prevent cells from adhering or attaching to one another and thereby promoting cell movement to other areas.
The predominant carriers of polySia in the brain are neural cell adhesion molecules (NCAMs), which are glycoproteins expressed on neuronal cell surfaces. As their name suggests, NCAMs by themselves are important in helping cells stick together and stay in one place. But when an NCAM becomes modified with polysialic acid (becomes “polysialylated”), the cells gain the ability to migrate to new areas. Re-expression of the “anti-adhesive” polySia glycan on the surface of many adult human cancer cells, for example, facilitates their detachment, thus enhancing their metastatic spread. PolySia found on human leukocytes also modulates immune function.
Neural stem cells with these polySia-NCAMs on their surfaces are important in embryonic development because they are able to travel throughout the body where they can differentiate into specialized cells. During adulthood, neural stem cells with polySia-NCAMs may migrate to injured areas and promote healing.
“The landscape of the cell surface of developing cells is decorated with a bewildering array of informational-rich sugar-protein molecules of which polysialylated NCAMs are of chief importance,” explains Troy. “During the life of a cell, these surface molecules are critical to cellular proliferation, self-renewal, differentiation and survival—essential processes for normal embryonic development and tissue regeneration in adults.”
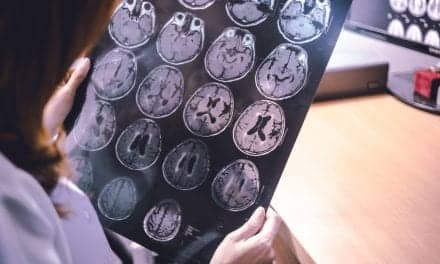
Although it was already well known that cells expressing polySia-NCAM exist in the central nervous system, this study is the first to document that they are also in the peripheral nervous system, specifically in the spiral ganglia, groups of nerve cells located in the inner ear that are essential to hearing.
Working with adult cells isolated from the inner ear spiral ganglia of guinea pigs, Troy’s team was able to show that they expressed both polySia and NCAM. The polySia component was abundantly present on neural stem cells but markedly reduced on mature cells, implicating the polySia-NCAM complex as being present on immature cells and able to serve as a biomarker to identify these cells.
“Finding polySia-NCAM— a functional biomarker that modulates neuronal differentiation— on adult inner ear neural stem cells after differentiation gives researchers a ‘handle’ to identify and isolate these cells from among the many cells taken from a patient,” said Jan Nolta, PhD, director of the UC Davis Stem Cell Program and the university’s Institute for Regenerative Cures. “This discovery will enhance research into spiral ganglion neurons and may bring treatments closer to patients with hearing deficits.”
The article is titled “Expression of polysialylated neural cell adhesion molecules on adult stem cells after neuronal differentiation of inner ear spiral ganglion neurons.”
Lead author Kyoung Ho Park, a professor at Catholic University College of Medicine in Seoul, Korea, initiated the research for this article while on sabbatical leave in Troy’s laboratory at UC Davis. With his colleague and co-author, Sang Won Yeo, he is now planning clinical trials, based on the findings, in Korea with individuals who suffer from hearing disorders.
The work was supported by the Catholic Institute of Cell Therapy Basic Science Programs Foundation, Research Fund Of Catholic University ENT Alumni, the National Institutes of Health Grant GM 55703 and Mizutani Glycoscience Foundation #130097.
Source: UC Davis Health System