Research | February 2021 Hearing Review
Aligning effective approaches and benefit for the psychosocial needs of adult patients
“Certainly in my case, the word is withdrawal. You withdraw back in yourself more and you don’t realize you’re doing it, but you are in effect hiding from the problem because you can’t accommodate it, you can’t handle it, you can’t change it and you just let it happen. Like a tide coming in it’s going to happen, so just sit back and do nothing.”
—Ms B, hearing aid owner, 2020
By Rebecca J. Bennett, PhD
Hearing loss is a complex and unique experience for each individual who develops it. Hearing loss not only compromises a person’s ability hear, but also to communicate, thus affecting their ability to effectively succeed in social activities and emotionally engage within social interactions.
Emotional distress is common in people with hearing loss and can take the form of frustration, anger, embarrassment, inferiority, shame, loss of identity, rejection, and loneliness. As hearing loss often gradually increases, people tend to unconsciously adopt both helpful and unhelpful coping behaviors. These can include avoidance behaviors such as non-attendance at social events or staying silent in group conversations.
At the same time, significant others can develop unsupportive behaviors, such as ignoring requests for repeats or excluding the hearing-impaired individual from complex conversations. Together, these unhelpful behavioral patterns drive social disconnection. The combined effects that a persons’ emotional experiences and social environment have on their physical and mental wellness is described as psychosocial well-being.
Psychosocial well-being is rarely addressed by audiological rehabilitation services. Despite the complex nature of hearing loss, and its wide-ranging impact on a person’s well-being beyond hearing sensitivity, current audiological practices tend to focus on technology (eg, hearing aids) to address the hearing deficit, rather than considering the clients lived experience of hearing loss and their psychosocial well-being.1
While hearing aids are effective in their ability to improve hearing sensitivity and communication,2 they do not fully address the psychosocial impacts of hearing loss3; adults with hearing loss are too often left bearing the burden of hearing loss even after accessing hearing rehabilitation services.
Although audiologists self-report a positive preference towards addressing their clients’ psychosocial needs relating to hearing loss, they also report lacking the knowledge, skills, and resources to do so.4,5 To better understand current practices, an international group of researchers and clinicians launched a research project exploring the ways in which audiologists currently provide psychosocial support to their clients.
Identifying Approaches Used to Address the Psychosocial Impacts of Hearing Loss
We asked an international sample of 65 audiologists to develop a list of ways in which audiologists address the psychosocial needs of their adult clients within their work setting.6 There was a variety of approaches described that included techniques, such as the development of personalized goals, exploration of psychosocial impacts of hearing loss, involvement of communication partners, promotion of self-management/ self-efficacy, promoting support groups, and referral to allied health and medical professionals. Specifically, audiologists identified 93 individual approaches in 7 conceptual clusters (Figure 1):
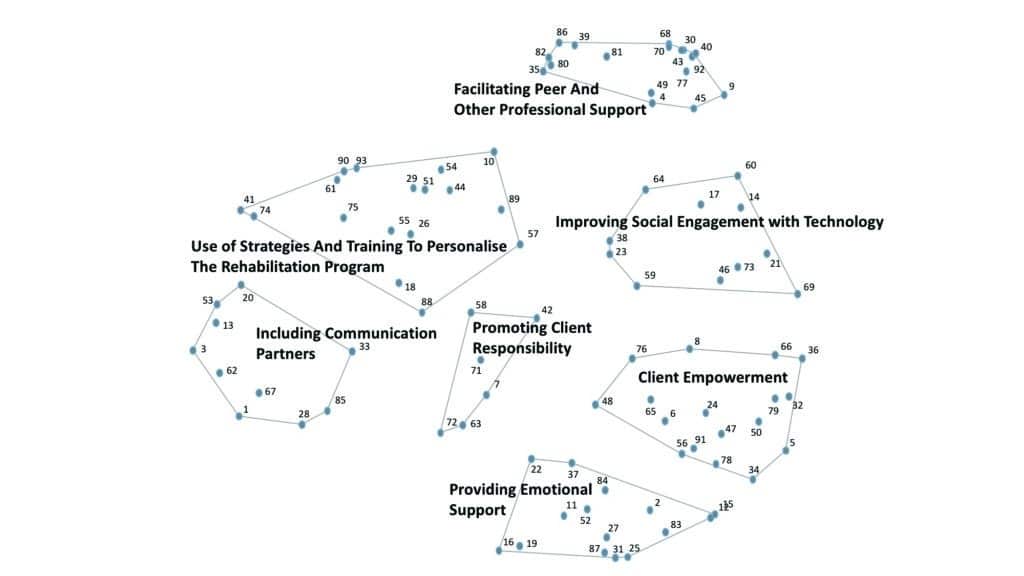
1) Client empowerment. Assisting the client to establish their rehabilitative goals based on individual needs. This included helping the client determine their wants, needs, and barriers, and tailoring the rehabilitation program to account for these personalized goals.
2) Use of strategies and training to personalise the rehabilitation program. The provision of individualized training and education to suit the client’s individual rehabilitation needs, such as communication strategies and use of assistive listening devices.
3) Facilitating peer and other professional support. Encouraging clients to become involved with the community and other people living with similar experiences (eg, attending support groups or via social media). Clients were also recommended to seek help from other professional health service providers to address specific needs, such as professional counseling support service.
4) Providing emotional support. Addressing and supporting the emotional needs of the client beyond technology, for example, by encouraging and supporting the client to express their thoughts and feelings.
5) Improving social engagement with technology. The audiologist’s role in improving social participation via amplification and other technological solutions;
6) Including communication partners. Incorporating tasks that include the clients’ significant others throughout their rehabilitation journey, such as educating them and encouraging them to share their perspectives.
7) Promoting client responsibility. Reinforcing the role that a client has in their own rehabilitation journey, such as promoting self-management of their hearing loss and self-advocacy (assertiveness) in social situations.
Interestingly, the majority of approaches put forward by participants in the current study were described informally and lacked an evidence-base—even though many evidence-based approaches do exist. The Ida Institute (www.idainstitute.com) has formalized several clinical approaches designed to provide psychosocial support, including the Communication Rings,7 the Goal-sharing for Partners Strategy,8 and the Group Rehabilitation Online Utility Pack (GROUP).9 Available evidence-based approaches to helping clients improve their communication and social skills include the Listening and Communication Enhancement program (LACE),10 and the Active Communication Education (ACE) program.11
Perceived Benefit and Likely Use of Approaches
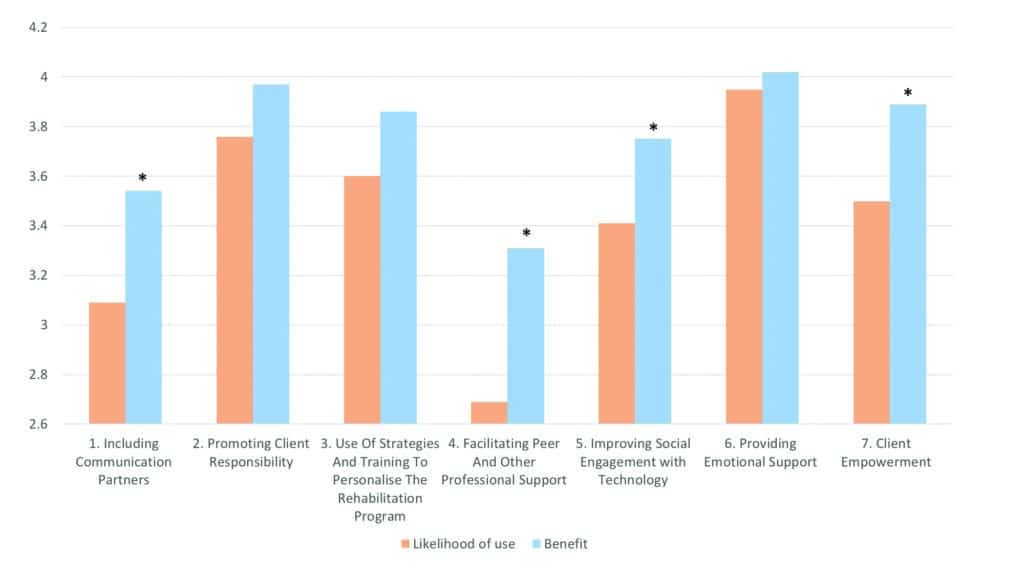
We further examined the clinical utilization of the approaches identified by surveying 52 adults with hearing loss and 19 audiologists.12 Participants rated the individual approaches on two scales: 1) Perceived benefit, and 2) Perceived likelihood of using.
Overall, both adults with hearing loss and audiologists rated the benefit and the likelihood of use of the approaches relatively positively, suggesting that they value addressing psychosocial well-being within audiology appointments. The highest-ranked theme was Providing Emotional Support, emphasizing the role that audiologists play in helping their clients adjust to the psychosocial impacts of their hearing loss.
We observed the overall trend that benefit was generally rated higher than likelihood of use (Figure 2). This discrepancy was highest for approaches relating to involvement of significant others, and referral support beyond the audiologist. It is possible that although audiologists consider the strategies beneficial, they may not be viewed as easy to implement into clinical practice. These results may point towards important needs of audiologists, and may highlight the strategies for which they require more support for implementation into daily practice.
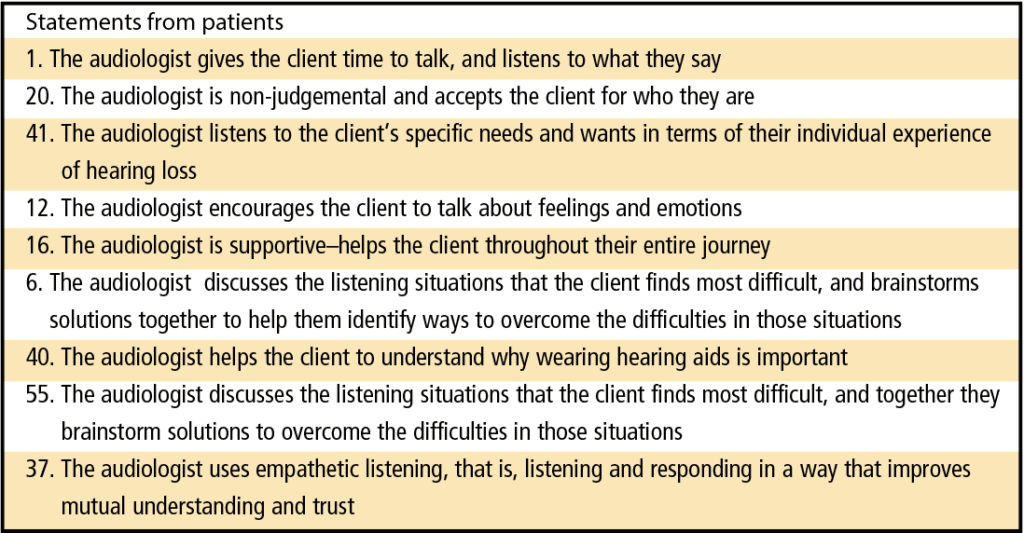
We plotted the two rating scales against each other to generate a scatter plot, resulting in a visual representation of participants’ ratings data for each individual approach (Figure 3). This enabled us to see the specific approaches that clients and audiologists deemed to be the most beneficial and more likely to be used.
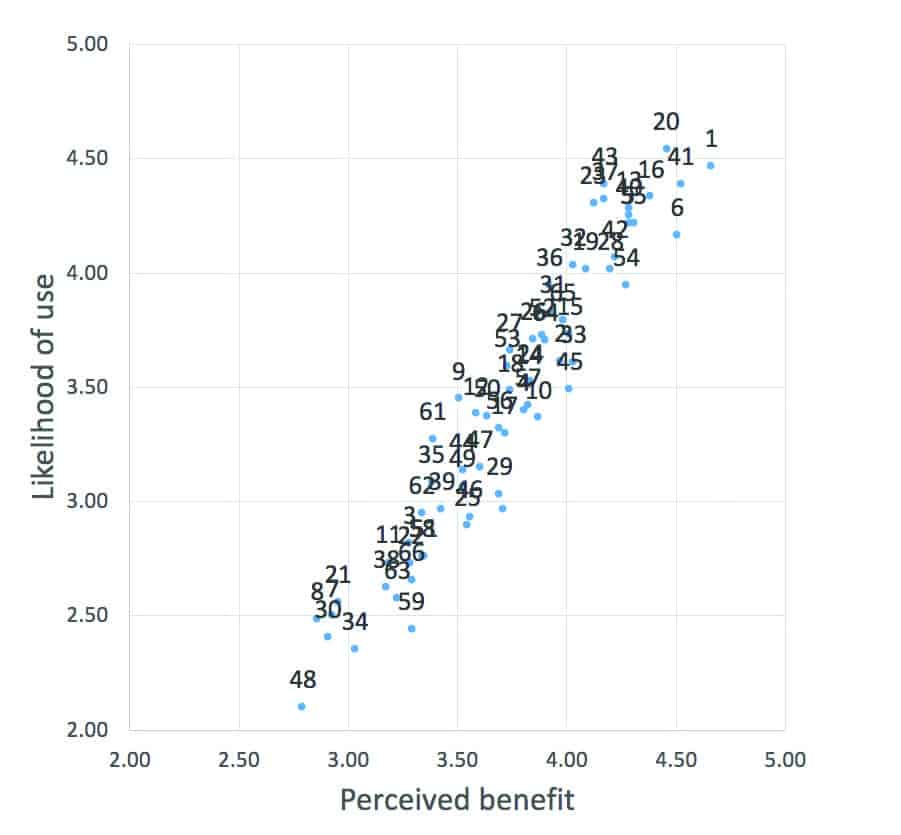
Table 1 provides the statements located in the top-right corner of the scatter plot (ie, the most beneficial and most likely to be used). It is clear to see that the majority of these relate to Providing Emotional Support. Although provision of emotional support is perceived to be both beneficial and desirable, it is rarely observed in the clinical setting,5,13 with audiologists describing reluctance providing mental health support driven by a lack of skill, time, and uncertainty about scope of practice.3 This may be influenced by the fact that counseling and emotional support skills have not previously been included and/or formalized in many audiology training programs. As such, practicing clinical audiologists require more training in this area.14,15
A recent Delphi study by Meibos et al16 described the range of knowledge, skills, and attitudes audiologists should adopt in order to become good counselors. Clinical audiologists could use this as a guide to support continued professional education in these areas.
In conclusion, there are a diverse range of ways in which audiologists can help their adult clients address the psychosocial impacts of hearing loss. Yet, clinical audiologists need to be proactive in identifying and addressing their own personal training needs. We need to challenge ourselves to expand the audiology toolbox. I would suggest setting a personal goal of selecting two strategies that were previously unfamiliar to you and work on incorporating them into your daily practice. For the full list of clinical strategies, visit the IJA website.6
Acknowledgements
The author thanks Sonova AG and Ear Science Institute Australia for funding this work, and the participants for their contributions. I am grateful for the guidance and support of my co-authors on this project: Caitlin Barr, Alex Cortis, Rob Eikelboom, Mel Ferguson, Daniel Gerace, Eithne Heffernan, Louise Hickson, Lisette van Leeuwen, Joe Montano, Jill Preminger, Marieke Pronk, Gaby Saunders, Gurjit Singh, Barbra Timmer, Barbara Weinstein, and Sandra Bellekom.

Citation for this article: Bennett B. addressing clients’ social and emotional distress relating to hearing loss. Hearing Review. 2021;28(2):14-16.
Correspondence can be addressed to Dr Bennett at: [email protected].
References
- Montano J. Overdependence on technology in the management of hearing loss. In: Goldfarb R, ed. Translational Speech- Language Pathology and Audiology. 1st ed. Plural Publishing; 2012:97-106.
- Ferguson MA, Kitterick PT, Chong LY, Edmondson-Jones M, Barker F, Hoare DJ. Hearing aids for mild to moderate hearing loss in adults. Cochrane Database Syst Rev. 2017(9):CD012023.
- Weinstein BE, Sirow LW, Moser S. Relating hearing aid use to social and emotional loneliness in older adults. Am J Audiol. 2016;25(1):54-61.
- Bennett RJ, Meyer CJ, Ryan B, Barr C, Laird E, Eikelboom RH. Knowledge, beliefs, and practices of Australian audiologists in addressing the mental health needs of adults with hearing loss. Am J Audiol. 2020;29(2):129-142.
- Bennett RJ, Meyer CJ, Ryan BJ, Eikelboom RH. How do audiologists respond to emotional and psychological concerns raised in the audiological setting? Three case vignettes. Ear Hear. 2020;41(6):1675-1683.
- Bennett RJ, Barr C, Montano J, et al. Identifying the approaches used by audiologists to address the psychosocial needs of their adult clients. Int J Audiol. 202060(2):104-114.
- Montano JJ, Al-Makadma H. The communication rings: A tool for exploring the social networks of individuals with hearing loss. Sem Hear. 2012;33(01):046-052.
- Preminger JE, Lind C. Assisting communication partners in the setting of treatment goals: The development of the Goal Sharing for Partners Strategy. Sem Hear. 2012;33(01):053-064.
- Montano JJ, Preminger JE, Hickson L, Gregory M. A new web-based tool for group audiologic rehabilitation. Am J Audiol. 2013;22(2):332-334.
- Sweetow RW, Sabes JH. Listening and Communication Enhancement (LACE). Sem Hear. 2007;28(2):133-141.
- Hickson L, Worrall L, Scarinci N. A randomized controlled trial evaluating the active communication education program for older people with hearing impairment. Ear Hear. 2007;28(2):212-230.
- Bennett RJ, Barr C, Cortis A, et al. Audiological approaches to address the psychosocial needs of adults with hearing loss: Perceived benefit and likelihood of use. Int J Audiol. 2020. DOI: 10.1080/14992027.2020.1839680.
- Ekberg K, Grenness C, Hickson L. Addressing patients’ psychosocial concerns regarding hearing aids within audiology appointments for older adults. Am J Audiol. 2014;23(3):337-350.
- Whicker J, Muñoz K, Schultz JC. Counseling in audiology: AuD students’ perspectives and experiences. Sem Hear. 2018;39(01):067-703.
- Whicker JJ, Muñoz KF, Butcher GM, Schultz JC, Twohig MP. Counseling training in AuD programs: A syllabi review. Hear Jour. 2017;70(8):36-39.
- Meibos A, Muñoz K, Twohig M. Counseling competencies in audiology: A modified Delphi study. Am J Audiol. 2019;28(2):285-299.