Patient Care | February 2022 Hearing Review
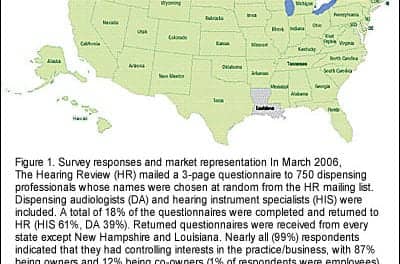
Good clinicians treat the hearing loss; great clinicians treat the patient who has hearing loss
By John Greer Clark, PhD, and Michael A. Harvey, PhD, ABPP
Dr Clark is an audiologist who has long encouraged colleagues to expand their counseling beyond content or information transfer in order to better assist adult patients and their caregivers, and parents of pediatric patients. Dr Harvey is a clinical psychologist with a private practice that includes extensive work with patients and families grappling with hearing loss and tinnitus related issues. Much of their professional writings aim at broadening audiologists’ awareness of the emotional support needs of patients and families with hearing disorders. This conversation explores these themes more fully.
We could both list a number of areas in which audiologists could provide greater support to their patients and our hope is to touch on some of the more important areas in this article. But to start, let’s look at patients’ motivation in addressing their hearing problems. As we all know, patient follow through on hearing aid recommendations is poor, as evidenced by the relatively low numbers of those who are fit with hearing aids.1 We have both written a considerable amount on empowering patients by helping them to examine their own levels of internal motivation to improve communication and their views toward their abilities to succeed in tackling perceived barriers to their success.2-7
Clark: So, to get things rolling, let’s start with the question: What keeps so many audiologists from more fully embracing the practice of motivational engagement with their patients?
Harvey: Permit me to digress a bit before I answer your question. There’s an old story about a seasoned therapist who decided to get training in treating patients who have been sexually abused. Thankfully, he took this training in the nick of time, because immediately afterward, his patients began disclosing their sexual abuse history. Obviously, the truth is that when the therapist was finally comfortable with that topic, patients followed suit.
The practice of motivational engagement with patients necessarily involves eliciting their feelings about everything that hearing loss affects—which is everything. I’m reminded of an audiologist who, while eliciting a patient’s motivation for hearing aids, felt overwhelmed by the patient suddenly crying uncontrollably. Like many healthcare providers, including audiologists, she didn’t have the requisite training to manage emotional aberrations. In addition to not knowing what to do, the patient crying triggered painful childhood memories of her mother’s untreated bipolar disorder. So a partial answer to your question is that we human beings, including hearing care professionals, tend to stick with familiar and comfortable behaviors.
And of course, there’s the omnipresent challenge of managing time constraints: why should you open a “can of worms” that is not only unfamiliar territory, but also that you fear may not be contained within the allotted appointment time. As you well know, practicing new skills can be difficult while coping with the numerable imposed stresses by the current healthcare system: EMR, insurance company denials, online reviews, declining reimbursement, and so on.
Stated differently, it may be easier to venture into unfamiliar emotional territory when not simultaneously deluged by all these external pressures. By necessity, one’s tenuous struggle to remain balanced takes priority.
Clark: I would agree that many are reluctant to step out of their comfort zones and embrace motivational engagement practices with their patients. As you and I have discussed before, audiologists ask their patients to move beyond their comfort zones every day when broaching the use of hearing aids. Hopefully, more audiologists will recognize they sometimes need to step out of their own comfort zones if they want to be more successful with those patients who are very reluctant to accept your recommendations for hearing aids. The references cited above give details on this approach with patients, as well as the time actually saved in many cases.
I know that we both agree that hearing care professionals are often uncertain as to how far their counseling endeavors can go before they cross professional boundaries. Through motivational engagement, as well as audiologic counseling aimed more at personal adjustment, clinicians can assist patients with many of their roadblocks and the normal emotional responses that accompany a hearing loss, which is very much like grieving.
This, of course, is done with a vigilance for unrelenting blockage toward success, persistent emotional distress, or harmful personal or family dynamics that would necessitate referral to a mental health counselor. To paraphrase the words of a psychotherapist that I have long remembered, audiologists are not working with mentally challenged individuals; they are working with people living within mentally and emotionally challenging circumstances. For many, hearing loss certainly would qualify as a source of mentally and emotionally challenging circumstances, but not all patients would need a mental health referral. However, we do need to be on the lookout for those who would benefit from a referral.
Do you believe that audiologists too frequently limit their counseling to information transfer?
Harvey: Yes. We all do what is most comfortable and familiar. Many people hypothesize that Sigmund Freud sat behind his patients who were on a coach, not as a psychoanalytic technique, but because he felt more comfortable having no eye contact.
Of course, professional boundaries are quite important, both ethically and efficaciously. Just as you’re not competent to practice psychotherapy, I’m not competent to practice audiology. But I think that, at times, one’s reluctance to so-called “cross boundaries” is more related to anxiety and the myriad of factors that are involved in effective teamwork.
You know, in school, I always preferred doing a project by myself because it didn’t involve the responsibility of maintaining clear communication, negotiating tasks, etc. As I’ve stated elsewhere,8 patients often tell their audiologists quite intimate feelings—some that they may not even share with a therapist—because they’re focusing on a third point, such as hearing aids or hearing test results and their implications. The clinician can and should respond in a therapeutic manner. Although it is therapeutic, it is not practicing psychotherapy.
John, turning to the topic du jour, I’m curious what you deem as unique personal adjustment considerations when treating patients with hearing loss in the midst of the pandemic?
Clark: As life for over two years in the midst of this pandemic has reminded us all, stress can take a tremendous toll on one’s psyche, emotional resilience, and health. Navigating life with hearing loss, caring for a child who has hearing loss, or serving as a primary caregiver for an older family member can certainly heighten one’s stress adversely, affecting physical health, outlook on life, and our emotional responses and behaviors directed toward loved ones. Stress associated with the pandemic can certainly amplify personal adjustment to other stressors, such as hearing loss.
I remember asking an elderly gentleman’s daughter-in-law while I was cleaning his hearing aids how she was holding up. As she shared with me, her whole life had been altered through the unanticipated life changes her new caregiver role presented. Her own children were grown, and both she and her husband were recently retired. They had just bought a small RV and had planned to travel to national parks around the states. And then changes in her father-in-law’s health resulted in his moving in with them, and she found she now had what appeared to be a new full-time job. While this patient encounter was pre-pandemic, one can only imagine how much greater this woman’s stress levels would have been during Covid. A brief mention of the existence of adult day care services for caregiver respite and the importance of self-care would certainly be appropriate.
Do you believe audiologist have a role to play in learning about the stresses their patients and family members may be experiencing and then providing recommendations that take these stresses into account?
Harvey: We healthcare providers, including hearing care professionals, have an important role to play in learning as much as possible about our patients’ lives beyond our individual specialties. In fact, this expanded understanding is essential! As one ophthalmologist joked, “I keep having to remind myself that it’s not only a pair of eyes who walk into my office.”
In terms of us empathizing with patients’ environmental stress and lifestyle challenges, the good news, at least from one perspective, is that we’ve all been through a hell of a time. As you said, Covid-19 has provided all of us with an unenviable opportunity to personally understand vulnerability, isolation, stress, etc, as we’ve struggled to maintain our own quality-of-life and relationships with loved ones in the midst of a worldwide pandemic.
Of course, in addition to the impacts of worldwide pandemics, our patients have relationships with key other people, referred to as the “relevant system.” There are always more people in the examination room than the audiologist and patient, although they’re invisible. Those persons may have a strong influence with how well, or if, the patient follows your treatment recommendations.
Regarding your example, it would be vitally important for an audiologist to understand and take into account potential caregiver stress and how this may effect, and be affected by, family dynamics. The identified patient affects the family which, in turn, affects the identified patient. At first glance, this so-called recursive cycle has the clarity of a bowl of spaghetti. How may the father-in-law’s challenges affect the daughter-in-law and vice versa? How may this dynamic affect the relationship between the daughter-in-law and her significant other? And how might this change affect other intra-familial relationships?
Clark: You mentioned the significant others who may not be physically present at the appointment—the invisible persons. How might the audiologist uncover who those might be and help patients explore how their own actions, or inactions, might impact more than themselves? We shouldn’t just leave it as a bowl of spaghetti.
Harvey: The audiologist can clarify who these invisible persons are who comprise the patient’s “relevant system” and their interactions—the patient’s bowl of spaghetti—by using a technique called circular questioning that was developed in Milan, Italy.9 This technique was developed as a result of examining unsuccessful clinical cases. Invariably, the lack of success was due to people in the relevant system that were not accounted for.
For example, you can ask: Who referred you and who knows about your appointment? Who is most concerned about your possible hearing loss? Second most? Third most? Which of these persons would be most concerned if you did or did not get hearing aids? Second most? Third most? These questions could be included in a form that the patient fills out. Filling out such questions on a form before meeting with the audiologist primes the thought process and prepares the patient for a more enlightening conversation when exploring responses later face to face, thereby saving clinical time.
Clark: Certainly patient and family emotions can be strong during clinical consultations. While hearing care professionals are well-versed in the impact of hearing loss and the emotions that may accompany different stages within a patient’s hearing loss journey, professional literature suggests that patients and family members may perceive us as lacking in empathy or requisite counseling skills.10-12 An attentive, non-defensive listening posture along with reflections of perceived emotions that might underlie patient statements (or family member statements as in the caregiver example) are key to combating negative perceptions of our levels of empathy.
Harvey:Adopting a non-defensive listening posture is easier said than done. Would you elaborate what this might entail and how one can demonstrate this?
Clark: Sure. Remaining non-defensive in clinical encounters becomes much easier when we learn to accept patient’s emotions in the clinic. For example, communication with hearing loss is stressful in some environments even with the best hearing aids. A patient may arrive at the clinic frustrated, exasperated, or possibly angry with a hearing aid that has left him stranded once again just when he felt he needed it most. The patient’s tone or demeanor toward the clinician may clearly reflect the emotions he’s experiencing.
A normal human response when we sense we are being blamed for something that was not our fault is to become defensive. Recognizing that the patient’s expressed emotions are really reflective of a situation and not necessarily aimed toward the clinician helps prepare us to be more empathetic in our response. An appropriate clinician response might be, “I’m so sorry you are having trouble with your hearing aid. That’s got to be upsetting. [Label the perceived emotion and reflect it back.] Let me see what we can do to get you hearing well again.”
Remaining calm and non-defensive, even if the patient’s response still seems negatively directed toward the clinician, will help to diffuse the situation and counter the possible impression that we might be insensitive or indifferent. What do you believe may be barriers to the success of a clinician’s empathic response?
Harvey: Displaying empathy is also easier said than done. Stalin said, “One death is a tragedy and one million is a statistic.” In other words, we can read about painful loss and trauma and hear stories, but it is another thing to bear witness to it firsthand from a patient in front of us. We have all learned from the news of the recurring shootings across our country, but a recent patient, in answer to my usual “How are you?” question, replied, “My sister-in-law got shot in the head and was among those murdered in Boulder, Colorado.” OMG!
Trauma is contagious. It’s frequently impossible to compassionately assist people who have suffered a major loss without somehow being changed. It has been described as the cost of caring.13 More precisely, those who bear witness to another’s traumatic hearing loss may experience vicarious trauma (VT): a psychological transformation in the helper’s inner experience resulting from empathic engagement with the patient. The helper becomes vulnerable to a variety of post-traumatic stress reactions that may feel like being hit with “a ton of bricks.”
Clark: I wasn’t expecting that response. Vicarious trauma and the ensuing compassion fatigue are such important topics for “helping professionals.” I was thinking of barriers such as the trap of treating all patients with similar hearing loss as if their experiences and needs are the same—in other words, treating the audiogram, or the need to avoid clinical multitasking so that we can better focus on the individual stories of our patients. What do you do for yourself, or recommend to others, to avoid VT?
Harvey: VT cannot be avoided. In fact, the most efficient way to increase VT effects is to pretend it doesn’t exist. So it’s not if, it’s when. There are well-documented, self-evident self-care strategies, such as being attuned to one’s needs, limits, emotions, and resources; maintaining balance among activities, especially work, play, and rest; and maintaining positive familial and social relationships.14,15 Personally, I have found that conversing with other professionals about my work is critical—as we are doing now.
I stumbled across another method, however. I had always wanted to play the hammered dulcimer. So I signed up for lessons. One day, the teacher talked about the value of improvisation: “Playing different notes keeps it new and interesting for both the audience and performer,” he said. That struck a chord for me (pun intended). Trying new techniques in my practice, and dealing with the fun and anxiety that goes with it, helps to keep it fresh. Sometimes, improvisation falls flat on its face; other times, it is a magical kind of creativity. But either way, it helps keep me psychologically alive and present.
By definition, improvisation is stepping outside your comfort zone, as you said earlier. However, while a comfort zone protects you from anxiety, it ushers in boredom. Comfort zones are overrated as their predictability and safety become routinized, and devoid of spontaneity. So improvisation is a win-win; it provides better patient care and protects us from the life-sapping effects of VT.
Clark: There are a number of threats to the well-being of our patients for which we should all be vigilant.3,16 The No Wrong Door Mental Health Charter posits that all healthcare venues should be able to serve as a portal to the wide variety of patient needs so that a range of services are accessible from multiple points of entry. Hearing care professionals are not mental health counselors, but we can open a dialogue, raise consciousness, and make referrals as the need arises. That’s clearly part of quality care.
While audiologists are not mental health professionals, we do see patients who may be at risk for suicide, childhood bullying, or child or elder abuse. Many of our patients may be living with encroaching cognitive decline, or within a strained relationship due to hearing loss and the challenges of life itself.16 How would you recommend that non-mental health professionals prepare themselves to broach needed conversations when these are suspected? And what wording would you suggest we use when making a referral for mental health care given the stigma many continue to hold toward seeking such assistance?
Harvey: This is an important consideration, as there are risks if a referral to a mental health professional isn’t done carefully. As one audiologist put it, “Suggesting mental health counseling to a patient could be badly bungled by even the most well-intentioned professional. There are lots of ways that could be misunderstood or presented in a poor way. It makes me nervous going that route.”
At the outset, one must have an appropriate referral network of psychotherapists who have specific competencies in evaluating and treating persons with hearing loss or tinnitus. Professionals without such expertise may do significant psychological harm by falsely minimizing and/or maximizing the effects of hearing impairment.
There are important steps to follow with patients who disclose painful feelings that warrant mental health treatment.
The first task is to validate a patient’s feelings by indicating that their feelings are normal—not crazy. Do not make the common mistake of saying “I understand how you feel.” It is impossible to truly “put yourself in another person’s shoes,” and patients are typically put off by this well-intentioned phrase. A better statement might be, “I can only imagine how difficult that must be.”
While validating a patient’s feelings, it is also important to gently set limits to (contain) their affect so it doesn’t consume the session or get out of control. Without limit setting, an audiologic visit may become more like a psychotherapy session. For example, an audiologist may say: “It sounds like you have a lot of painful feelings. I can appreciate that, as I’ve heard many people with hearing loss talk about this a lot. We don’t have more than a few minutes, but I’d really appreciate it if you could give me a glimpse of your pain.”
Second, normalize (de-stigmatize) the referral. When first referencing the patient’s persistent emotional pain that might warrant a referral, do not use loaded words such as “therapist,” “mental health,” or “psychotherapy.” Although well intentioned, these words may be experienced by patients as assaults to their self-esteem and integrity. Instead, it is important to justify a referral according to what the patient values. Skills training is a common strategy. For example, an audiologist may say, “You know, there are audiological ways of helping with hearing loss and there are also psychological techniques, especially for the pain that accompanies hearing loss. The first is something I do; the second is another professional I know.”
Third, emphasize that optimal treatment of hearing loss often necessitates a team approach. The clinician can make reference to the mind-body connection or terms such as “holistic” or “multi-disciplinary approach” which are recognized and accepted in today’s culture. The team can be framed as a partnership between audiology and psychology.
Fourth, humanize the mental health professional. The more patients know about who they are being asked to see, the less anxiety and fear of the unknown they will experience. Anticipatory anxiety will be reduced. Most patients assume adequate professional competence and training, so this is typically not a major source of anxiety. However, a prospective professional’s personality, warmth—his/her human qualities—typically are deemed most important.
Fifth, ask permission to telephone the mental health professional in front of the patient. As a second option, ask permission to make that contact soon afterward and inform the patient immediately after you have made the call. The goal is to decrease the psychological space between the audiologist-patient and the therapist.
Finally, at a subsequent visit ask the patient about the status of the referral appointment as a way of keeping the referral “on the front burner.” The tone of this inquiry should be one of support, as opposed to undue pressure. If a patient doesn’t follow through on contacting the therapist, an audiologist may say, “You know, this is not the kind of thing that points are taken off of your final grade. But would you help me understand what you were thinking or feeling that may have made you not make the call?”
As we’ve discussed, teamwork often is more effective than working in isolation. The gestalt is more than the sum of its parts. And collaboration is also much more rewarding, despite its inherent tasks. In many cases for providing optimal treatment for patients with hearing loss and/or tinnitus, two heads—an audiology head and a psychology head—are better than one.
However, as you know, our healthcare system isn’t set up for this as there is no reimbursement for collaboration. Do you have any thoughts about how such collaboration can happen more often?
Clark: Yes, it is unfortunate that healthcare doesn’t foster better collaboration. Collaboration takes many forms and often is not as time-consuming as one might think. As I said, we need to remember we aren’t working with mentally ill people. Most of our patients don’t need mental health services. But, just like the general population, many do. And with the additional stresses and social isolation that may accompany hearing loss, the numbers may be higher within one’s clinical caseload than within the general population.
Like most codes of ethics, the code of ethics of the American Academy of Audiology specifically states that, “individuals shall use available resources, including referrals to other specialists…”17 As you said earlier, it is important that we establish a referral network of psychotherapists who have competencies in working with those who have hearing loss. Mental health professionals who are seeking new patients are most often open to meeting with other professionals who state they are looking for someone who could work with their patients when the need arises. A luncheon meeting affords the opportunity for the audiologist to discuss the limitations of hearing aids which can result in ongoing interpersonal challenges and isolation, as well as to provide specific suggestions for successful communication in a clinical session such as clear speech and other communication strategies.
This type of networking is what makes one a professional and has benefits that serve both parties. It is very likely that the psychotherapist will begin to recognize those patients who may need audiologic services and be in the position to make a reciprocal referral to the hearing care professional.
Harvey: Often, our careers and specialties are shaped by life experiences. In my case, when I learned about my parents’ impending divorce at age 13, I offered to try to talk some sense into my father. My mission failed. It’s no wonder then why I became a psychologist! John, you are among the mavericks in what you and Kris English have come to call counseling-infused audiologic care, the title of the most recent edition of your book. May I ask what prompted you to emphasize the personal adjustment counseling aspect of audiology as opposed to what you term “Dr Informative”?
Clark: Well, after more than 25 years in private practice, I certainly recognize that the bulk of the counseling audiologists do is information transfer or content counseling. Hearing loss treatment simply requires delivery of a lot of information to patients and family members. Certainly when we look at studies on information retention,11,18-21 there is a great deal of improvement most of us could make, even in the area of content counseling.2
Years ago when I was exploring a personal health concern, I realized that many of the healthcare providers I consulted failed to recognize the depths of my own concerns (heightened emotions), didn’t ask me how I was feeling about the information I was given, glossed over questions I asked, and didn’t openly encourage additional questions. I found that I often left appointments unsure of where things were going or what active measures could be taken to aid in rendering a diagnosis or assist in treatment. In short, the humanistic side of patient care delivery that we now refer to as person-centered care was lacking.
I began a journey of reading on healthcare and counseling that quickly revealed that my experiences were very common. At one point I ran across Sir William Osler’s admonition to medical students that “The good physician treats the disease; the great physician treats the patient who has the disease.”
I don’t know if Dr English has a similar story, but we have both long believed that by expanding content counseling with more active engagement, audiologists can serve their patients better. Beyond providing information, there is a great deal that audiologists can do to help both pediatric and adult patients, as well as their family members, better combat the negative impacts of hearing loss; to assist them to act on identified internal motivators to more fully embrace recommendations; and to facilitate the personal empowerment requisite to successfully address hearing challenges.
To do these things is not outside of an audiologist’s scope of practice, is not time prohibitive (and sometimes saves clinical time), and is rewarding to both those we serve, as well as ourselves.
There are many wonderful audiologists in this country and many of them know and do most everything we’ve been talking about. Hopefully, parts of our conversation will be helpful to some of those who struggle with how to expand the counseling they give to their patients.
Harvey: Agreed. A multi-disciplinary approach with patient-centered care and counseling at the forefront is helpful to our patients, our professions, and ourselves—both as practitioners and individuals!
Correspondence can be addressed to HR or Dr Clark at: [email protected].
Citation for this article: Clark JG, Harvey MA. A conversation between an audiologist and a psychologist. Hearing Review. 2022;29(2):12-17.
References
- National Institute on Deafness and Other Communication Disorders (NIDCD) website. Quick statistics about hearing. https://www.nidcd.nih.gov/health/statistics/quick-statistics-hearing. Published March 25, 2021.
- Clark JG. The geometry of patient motivation: Circles, lines, and boxes. Audiology Today. 2010;21(4):32-40.
- Clark JG, English KM. Counseling-infused Audiologic Care. 3rd ed. Cincinatti, OH: Inkus Press; 2019.
- Clark JG, Maatman C, Gailey, L. Moving patients forward: Motivational engagement. Seminars in Hearing. 33(1):35-45.
- Harvey MA. What your patients may not tell you. Hearing Review. 2010;17(3):16-20.
- Harvey MA. The hearing health care journey: Putting beans in your cups. Seminars in Hearing. 2020;41(1):68-78.
- Harvey MA, Citron D. The Tevye phenomenon: Why one may be ambivalent about using motivational engagement tools. Hearing Review. 2020;27(1):14-19.
- Harvey MA. The transformative power of an audiology visit. Hearing Journal. 2000;53(2):43-47.
- Palazzoli MS, Boscalo L, Cecchin G, Prata G. The problem of the referring person. Journal of Marital and Family Therapy. 1980;6(1)3-9.
- Glass LE, Elliot H. The professionals told me what it was, but that’s not enough. SHHH Journal. 1992;12(1), 26-29.
- Martin FN, Krueger J, Bernstein M. Diagnostic information transfer to hearing-impaired adults. Texas Journal of Audiology and Speech Language Pathology. 1990;16:29-32.
- Sjoblad S, Harrison M, Roush J, McWilliam RA. Parents’ reactions and recommendations after diagnosis and hearing aid fitting. American Journal of Audiology. 2001;10(1):24-31.
- Figley CR, ed. Compassion Fatigue. Routledge; 1995.
- Meichenbaum D. Self-care for trauma psychotherapists and caregivers: Individual, social and organization interventions. Handout for workshop at the Melissa Institute.
- Saakvitne KW, Pearlman LA. Transforming the Pain: A Workbook on Vicarious Traumatization. New York, NY: WW Norton; 1996.
- Clark JG, English KM, Montano JJ. Heightening our vigilance towards patient well-being. International Journal of Audiology. 2021; 60(Sup2):4-11.
- American Academy of Audiology (AAA) Code of Ethics. https://www.audiology.org/wp-content/uploads/2021/05/201910-CodeOfEthicsOf-AAA-1.pdf. Published 2019.
- Anderson JL, Dodman S, Kopelman M, Fleming A. Patient information recall in a rheumatology clinic. Rheumatology. 1979;18(1):18-22.
- Kessels RPC. Patients’ memory for medical information. Journal of Royal Society of Medicine. 2003;96(5):219-222.
- McGuire LC. Remembering what the doctor said: Organization and older adults’ memory for medical information. Experimental Aging Research. 1996;22(4):403-428.
- Reese JL, Hnath-Chisolm T. Recognition of hearing aid orientation content by first-time users. American Journal of Audiology. 2005;14(1):94-104.