Summary:
Yale researchers have restored hearing in mice with ENPP1 deficiency using a novel bone-targeted enzyme replacement therapy, offering hope for treating hearing loss in patients with this rare and often fatal genetic disorder.
Key Takeaways:
- Breakthrough in Treatment: The new therapy reversed hearing loss in ENPP1-deficient mice by normalizing mineralization in inner ear bones, fully restoring hearing.
- ENPP1 Deficiency Impact: This rare genetic disorder affects mineralization, leading to severe complications including skeletal issues, vascular disease, and hearing loss in up to 75% of patients.
- Broader Potential: The success of this bone-targeted enzyme therapy in mice may have implications for treating other forms of hearing loss linked to abnormal mineralization, such as age-related hearing decline.
Scientists have successfully restored hearing in animal models of ENPP1 deficiency, a genetic disease in which individuals lack an enzyme essential for bone and blood vessel health. The rare disorder can cause hearing loss in as many as 75% of patients who live with it.
ENPP1 deficiency can have devastating consequences. Half of infants born with the disorder will die within six months. Those that survive often experience complications such as skeletal abnormalities, impaired growth, and hearing loss. Over the last decade, Demetrios Braddock, MD, PhD, professor of pathology at the Yale School of Medicine, has been studying enzyme replacement therapy as a potential treatment for the disease. In 2015, he created a new therapy that has shown promise in improving the skeletal abnormalities associated with ENPP1 deficiency and is in the process of clinical trials. However, it was unclear if this drug could also improve hearing loss.
Now, as described in a study published in the Journal of Bone and Mineral Research, the researchers have adjusted the drug so that it specifically targets bone. They found that this novel bone-targeted enzyme replacement therapy reversed hearing loss in ENPP1 deficient mice.
“We developed this drug to see if we could improve hearing loss, and we found that the drug offers a complete restoration,” says Braddock. “The data is striking in that the bone-targeted drug completely normalizes the bones in the inner ear that are responsible for hearing.”
What is ENPP1 Deficiency?
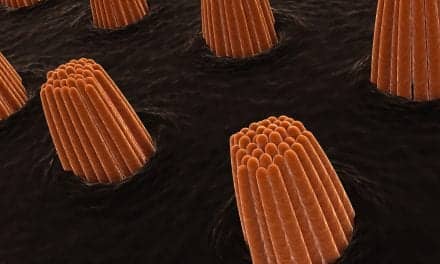
ENPP1 enzyme activity regulates how minerals are deposited in the body, a process called “mineralization” that is essential for maintaining healthy blood vessels and bone development. In individuals with ENPP1 deficiency, low levels of the enzyme contribute to a buildup of calcium deposits in the arteries, making them stiff and narrow, and hinder bone formation. The majority of people with ENPP1 experience hearing loss, which studies suggest may be due to dysfunctional mineralization of the bones in the ear.
Living with hearing loss as a result of ENPP1 deficiency can drastically affect one’s quality of life, especially for children. “For children who can’t hear, it can be socially isolating. They’re often delayed in terms of their performance in school,” says Braddock. “And this is on top of all of the mobility issues that these kids face.”
Bone-Targeted Enzyme Replacement Therapy Treats Hearing Loss
In the new study, the team treated mouse models of ENPP1 deficiency with weekly injections of their novel bone-targeted enzyme replacement therapy starting at 5 weeks old (equivalent to human adolescence, by which children with ENPP1 deficiency have typically already experienced hearing loss) to 17 weeks.
Mice that received the therapy fully regained hearing. The researchers also examined the bones in the inner ear and found that the therapy prevented dysfunctional mineralization.
“This suggests that we can treat the hearing loss in patients with ENPP1 deficiency and maybe even bring it back to normal,” says Braddock.
He is hopeful that these findings not only have implications for helping patients with the rare genetic disorder, but also those experiencing hearing loss due to a range of causes. Hearing loss caused by aging, for example, is also sometimes associated with mineralization, and a similar approach could potentially be used to treat these cases.
Outside of the laboratory, Braddock’s patients inspire him to keep searching for new ways to treat the devastating consequences of ENPP1 deficiency. “It’s a terribly impactful problem, but it has a very simple solution,” he says. “As a physician and a scientist, I feel compelled to try to explore that solution and bring it to patients.”