ANSD or retrocochlear pathology? And what should be recommended?
Pediatric patients do not always fit neatly into a definitive diagnostic category. This case shows that test results can be confusing or misinterpreted on face value, and also demonstrates the importance of a multidisciplinary team approach in the diagnosis and treatment of pediatric patients.
Diagnosis and intervention for auditory neuropathy spectrum disorder (ANSD) are debatable and controversial topics in the world of pediatric audiology. The case study presented here is complicated by the question of differential diagnosis between a potential diagnosis of ANSD versus a diagnosis of retrocochlear pathology in a preterm infant.
Confusing Test Results
A.B. was born at 34 weeks (8.5 months) gestation, had hyperbilirubinemia, and utilized mechanical ventilation for 5 days after birth. He did not pass his newborn automated au v fcd Figure 1 shows that the ABR results were not consistent with any repeatable waveform function and were inaccurately identified as being “normal.” Unfortunately, this ABR represents the beginning of a very long road for this family to obtain an accurate diagnosis for their child.
Three years later, A.B. was referred to an audiologist by his pediatrician due to concerns regarding speech delay. The family had no reason to believe that their child had hearing loss because of the previous normal ABR finding, and they went to a local university for a hearing evaluation. This family then went through 2 years of inconsistent audiological evaluations. Every evaluation had different results, but OAEs were reported to be present bilaterally on two occasions.
Finally, the educational audiologist through the public schools recommended that this patient receive a follow-up sedated ABR to confirm the presence or absence of a hearing loss. The ABR results were reported by the audiologist as “no clear repeatable air or bone conduction ABR responses noted at maximum levels of the equipment bilaterally.” Cochlear microphonic was noted at higher levels of stimulation. ASSR thresholds were also reported between the 90 to 100 dBeHL range for the frequencies 500 to 4000 Hz.
ANSD or Retrocochlear Pathology?
Although ASSR is a very beneficial diagnostic tool in audiology, recent research suggests that, in cases where auditory neuropathy is present, the ASSR thresholds may not be accurate.1 The results of the ABR were consistent with ANSD, and the audiologist reported this to the family. The child was then fit with low-gain hearing aids bilaterally, and the family was instructed to enroll him in speech and language therapy.
The parents received the diagnosis of ANSD and were confused and frustrated, so they then came to Cincinnati Children’s Hospital Medical Center (CCHMC) for a second opinion and possible cochlear implant referral. Four years after their initial evaluation, they received another sedated ABR at CCHMC. After evaluating the morphology of the ABR waveforms to click stimuli at 95 dBnHL, the results showed a clear Wave I and a clear Wave III. All other waveforms were questionable or absent.
At this point in his care, the results were consistent with a retrocochlear pathology. Since Wave I arises from the distal portion of the VIIIth nerve, and Wave III arises from second order neuron activity in or near the cochlear nucleus, the results suggested synchrony up until this point in the brainstem. OAEs were also measured and were found to be absent from 1500 to 8000 Hz bilaterally. Thus, the OAE results changed in the course of this child’s evaluation, as OAEs were reported to be present during two evaluations in the past.
Puretone Testing and Amplification
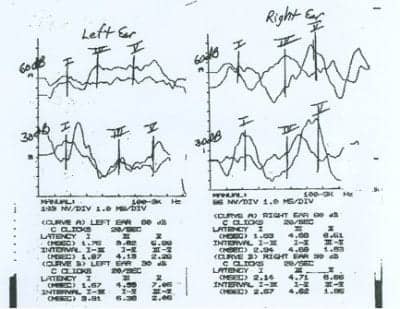
Figure 1. ABR results for A.B. that were unfortunately misidentified as being “normal.”
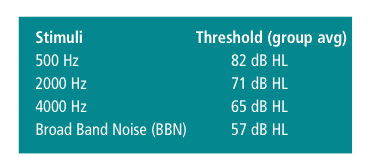
Following recovery from sedation, A.B. returned to the audiology department for puretone audiometry in the sound booth on the same day. These results differed greatly from the ABR results. Threshold testing was consistent with a moderate-to-severe sensorineural hearing loss bilaterally. Word recognition testing was also completed and was very poor bilaterally. A.B. had no open-set word recognition and had to complete the testing using a NU-Chips closed-set picture identification test, indicating very poor receptive word recognition skills.
A.B. was wearing his hearing aids, but they were programmed for a mild hearing loss. Historically, when auditory neuropathy was discovered, the initial recommendation was to fit the children with low-gain hearing aids.2 The reasoning behind this recommendation was the potential risk of damage to outer hair cell function (if present) and/or uncertainty regarding how children with AN would react to hearing aids.
Since 1998, research now supports fitting to the audiogram in almost all cases of auditory neuropathy.3 The audiologist refit A.B.’s hearing aids to his puretone audiogram. Aided testing completed that day yielded responses in the mild hearing loss range. A.B. and his family returned home to wear the aids for a couple of months and enroll the child in speech and language therapy in their community.
More testing and investigation. Once a patient is identified with a hearing loss at CCHMC, they are referred to the Ear and Hearing Center. This is a multidisciplinary clinic within the Division of Otolaryngology comprised of professionals who specialize in assessment and intervention for children with hearing loss. Once a child is referred to this clinic, they are scheduled with a series of appointments including genetics, aural rehabilitation, speech pathology, audiology, psychology, developmental pediatrics, radiology, and otolaryngology. This allows all aspects of the child’s auditory system to be evaluated and any potential diagnosis to be identified. In this case, A.B. had a normal MRI, which was very important in terms of his diagnosis. There was no evidence of a retrocochlear pathology as seen by his radiographic images. It is also important to note that his developmental evaluation concluded that his global development was age-appropriate.
A.B. returned approximately 1 month later for a hearing and aural rehabilitation evaluation. His hearing thresholds in the right ear remained stable, while his left ear dropped to a moderately severe to profound hearing loss. Open-set word recognition scores were unobtainable, and age-appropriate closed-set word recognition scores using Word Intelligibility by Picture Identification (WIPI) were <50%. Amplification benefit was judged poor, as the aided WIPI scores in the binaural condition did not improve. Despite consistent hearing device usage, A.B. did not make expected auditory comprehension progress.
The patient then had an aural rehabilitation evaluation composed of several tests. The first test he completed was a Ling 6 Sounds Test4 designed to assess his ability to perceive and recognize speech sounds. A.B. was able to detect all the sounds at 3 and 6 feet, but was unable to discriminate or produce any of the sounds.
He then completed an Auditory Skills Checklist (ASC)5 to assess his auditory skill level. The ASC assessment determined that A.B.’s auditory skills did not follow the typical auditory hierarchy of development.6 His identification scores were better than his discrimination scores; thus, his language development was more advanced than his auditory perception development. This finding indicated that his auditory comprehension and production were not consistent with sensorineural hearing loss.
His results also showed poor auditory memory. He was unable to recall two-word phrases and could only recall one familiar word with accuracy. The Test of Auditory Comprehension of Language (TACL) was also completed to assess auditory language comprehension. A.B.’s performance was no better than the 5th percentile on any portion of the examination. The aural rehabilitation audiologist reported that A.B. exhibited results very similar to patients with diagnosed auditory neuropathy.
Counseling and New Amplification
At this point in A.B.’s intervention, the audiologist needed to ask the family some key questions: Do the parents understand his auditory capacity at this time? Is A.B. in the appropriate learning environment? Are the tools he needs to succeed available to him? Is he enrolled in the appropriate therapy for his skills to improve? Does he have appropriate goals? The team felt as though his family was giving him all the tools necessary to succeed to the best of his abilities. His family understood his auditory limitations and made the appropriate accommodations. He was also a very good hearing aid user, so any benefits from the amplification would be conveyed in his results.
A.B. returned in 6 months and was refit with power hearing aids. He performed significantly better with these aids. He was able to complete a WIPI with 84% accuracy in his better ear, which is a vast improvement compared to his previous word recognition testing.
His family, teachers, and private speech pathologist reported progress in his receptive and expressive language. He currently utilizes an FM system, interpreter, and note-taker during school. His parents engaged in many communication strategies with him, such as signed speech, “auditory sandwich,” pre-teaching, and repetition at home. Despite these gains, A.B.’s speech pathologist reported that he did not receive sufficient spectral information to fully support auditory learning, and reported back to the team that a cochlear implant should still be a consideration. Although this opinion was taken into consideration, the parents and cochlear implant team decided that, since he was making significant progress, a cochlear implant would not be pursued at this time.
Discussion
As clinical audiologists, A.B.’s case reminds us of many things. Some patients do not neatly fit into a definitive diagnostic category. Although A.B. has characteristics of ANSD, his ABR was not consistent with this diagnosis. In the end, every child is different and it’s better to leave the diagnosis as “undetermined” or “possible” than to treat a child for a disorder that they may not have.
This case also reminds us of the importance of a team approach in diagnosis and treatment. All aspects of this child’s hearing loss, anatomy, language skills, and speech development were evaluated prior to determining a treatment plan. A.B. was able to use appropriate amplification and expand on his skills.
At this point, A.B. is making progress but will be monitored every 6 months by the cochlear implant team. In the end, thanks to the team approach, family involvement, and alternative communication methods, A.B. continues to make progress and is able to communicate to the best of his abilities.
Acknowledgements
The author thanks Molly Bertinato, AuD, Laura Welte, AuD, David Brown, PhD, and Lisa Hunter, PhD, for their contribution, assistance, and support. This case study was originally presented at the Starkey First Pediatric Symposium in September 2010.
References
- Jafari Z, Malayeri S, Ashayeri H, Farrahani MA. Adults with auditory neuropathy: comparison of auditory steady-state response and pure-tone audiometry. J Am Acad Audiol. 2009;20(10):621-628.
- Hood L. Auditory neuropathy: what is it and what can we do about it? Hear Jour. 1998;51(8):10-18.
- Hayes D, Sininger Y, Starr A, et al. Guidelines for Identification and Management of Infants and Young Children with Auditory Neuropathy Spectrum Disorder (2008). Available at: www.thechildrenshospital.org/conditions/speech/danielscenter/ANSD-Guidelines.aspx. Accessed September 7, 2011.
- Ling D. Speech and the Hearing-Impaired Child: Theory and Practice. Washington, DC: AG Bell Association; 1976.
- Meinzen-Derr J, Wiley S, Creighton J, Choo D. Auditory Skills Checklist: clinical tool for monitoring functional auditory skill development in young children with cochlear implants. Ann Otol Rhinol Laryngol. 2007;116(11):812-818.
- Erber NP. Auditory Training. Washington, DC: Alexander Graham Bell Association for the Deaf; 1982.
Correspondence can be addressed to HR or Erin Pinsky, AuD, at .
Citation for this article:
Pinsky E. Amplification and Team Management of a Pediatric Patient with Suspected ANSD Hearing Review. 2011;18(11): 24-26.