November 2013 HR | Cover Story
Interventional Audiology: Partnering with Physicians to Deliver Integrative and Preventive Hearing Care
Why physicians need audiologists and dispensing professionals, and why we need them.
Interventional audiology requires that audiologists and other hearing care professionals change their orientation toward patient care. Rather than centering on the dispensing of a hearing aid or medical device, interventional audiology revolves around the disease state of hearing loss and its relationship to the chronic medical conditions listed in this article.
As we grow older, most of us are inclined to ask, what is the secret to a happy life? Fortunately, we live in an era in which the near-infinite processing power of computer algorithms can help us more definitively answer this question.
A team of researchers led by George Vaillant at Harvard University have been collecting data for a longitudinal study that is attempting to better understand the secrets of a happy life. Through a painstaking, 4-decade process, 268 men participated in a series of interviews, which researchers used to establish a Decathlon of Flourishing—a set of 10 accomplishments that define success. Two of the 10 items were related to economic success, four with mental and physical health, and four with social supports and relationships. Researchers found that a loving childhood, filled with warm relationships through young adulthood, was highly correlated with all items on the Decathlon of Flourishing.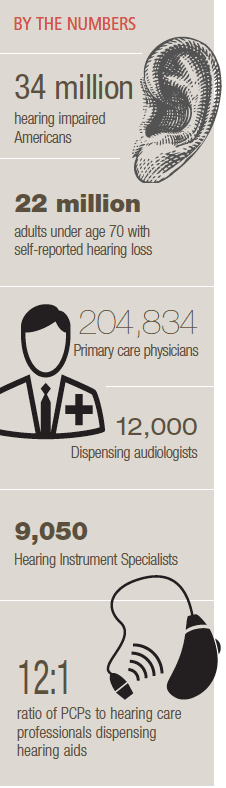
On the other hand, there were weak correlations among the other socioeconomic and biologic variables. Their work, Triumphs of Experience,1 demonstrates that an entire lifetime filled with warm and loving relationships (not high IQ, good grades, or wealth) are predictive of a happy life as you grow older.
This fascinating longitudinal study serves as a reminder that audiologists and hearing instrument specialists play a crucial role in maintaining the overall health and vitality of all individuals regardless of age. After all, if you have difficulty hearing, those warm and loving relationships that are the secret to a long and happy life are bound to suffer.
The primary objective of this article is to shed light on the emerging role audiology plays in the long-term delivery of care to patients of all ages, especially those with multiple chronic medical conditions. It is only through better communication—of which good hearing acuity is imperative—that adults suffering from multiple chronic medical conditions will be better able to more actively participate in their care, including the ability to follow a physician’s verbal instructions during a routine appointment.
The secret to a healthy practice may be similar to the secrets of a happy life: warm, lasting relationships with patients, colleagues, and other professionals. These interconnected networks may be more critical to your success than effective business management principles or the latest hearing aid technology that you offer in your clinic.
After reading this article, we hope you take action by fostering deeper relationships with the primary care physicians (PCPs) in your area. Before taking action, however, there are certain standards that must be put into place. Audiologists and their hearing instrument specialists cannot simply show up at PCPs’ offices and expect them to embrace your request to create a long-term partnership. Thus, we believe the profession needs a new subcategory, called Interventional Audiology. Authors’ Note: We use the term PCP to broadly define physicians, such as family medicine doctors, gerontologists, general practitioners, and others who are often the first to examine individuals who are likely to suffer from hearing loss and other conditions associated with hearing impairment. Likewise, although we use the term Interventional Audiology, we do not mean to exclude any qualified hearing care professional, including hearing instrument specialists, from this discussion.
Interventional Medicine
Over the past few decades, interventional medicine has become an important part of healthcare. As modern science has devised effective treatments for many disease states, healthcare delivery models have increasingly emphasized the treatment of chronic disease and the promotion of healthy lifestyles. By early detection and non-invasive treatment of various medical conditions, interventional medicine fits squarely within this preventive healthcare delivery model.
It should come as no surprise that the fundamental issue driving this change is the growing cost of healthcare. As costs have increased, so has the urgency to prevent illness whenever possible. The mantra of primary care today is “right care, right time, right provider.” This means prevention or the earliest possible intervention with the best possible treatment for chronic illnesses, such as diabetes, dementia, cardiovascular disease, and related disorders.
In fact, the most common chronic condition experienced by adults is some combination of many of these conditions, which is called multi-morbidity. Recent research suggests that almost 3 in 4 individuals over the age of 65 have multiple chronic conditions.2 Additionally, 1 in 4 adults 65 years of age and younger also have multiple chronic conditions.3 According to Anderson,3 patients with multi-morbidities are the major users of healthcare services and account for more than two-thirds of the healthcare spending in this country. To align with the clinical reality of multi-morbidity, experts have called for care to evolve from a disease orientation to a patient-goal orientation, focused on optimizing the long-term health of individuals.4 Hearing care professionals are well-equipped to step into this situation and provide valuable interventional services.
The rising costs of healthcare and the growing aging population are on a collision course that requires intervention from audiology. Audiologists have a significant opportunity to become an integral part of a physician’s team of trusted advisors and play an essential role in this effort to provide the right care at the right time. With interventional hearing healthcare strategies that seek to minimize impairment and maximize function, the audiologist will play an increasingly prominent role in the future in controlling healthcare costs, while delivering timely, cost-efficient, and highly effective care.
Interventional Audiology
Before going into the details of the role of audiology and hearing healthcare in an interventional delivery model, it is helpful to review the history of interventional medicine. Interventional medicine’s origins can be traced back to ancient Egypt and the Babylonian Period. With long-term accumulation of experiences, interventional medicine evolved as a system with the rise of interventional radiology treatment in the 20th century. New technological advances and innovative procedures have accelerated the improvement of interventional medicine in specialties that notably include interventional oncology, chemotherapeutic drug-eluting systems and bland beads for the targeted treatment of liver cancer, interventional cardiology, pulmonology, nephrology, pain management, as well as interventional otology and neuro-otology. Interventional audiology may soon be added to this list, as it offers tremendous promise in helping audiologists and hearing instrument specialists expand their reach to greater numbers of patients.
According to MarkeTrak data, the average age of a patient in the United States who is fitted with their first pair of hearing aids is 69 years, many of whom are seen for the first time by an audiologist for a hearing test shortly before their initial purchase. This suggests that society categorizes hearing loss as “a disease of the aged.” Recent research, however, demonstrates that hearing loss is now “a disease for all ages.”
Evolving to an interventional audiology model means, using one example, that a 21-year-old with a hearing disability caused by the co-morbid condition of type 2 diabetes may spend over 60 years of their life with communication disorders, an increased risk of depression, enhanced social isolation, and reduced employment opportunities because of a lack of systematic interventional strategies by both primary care specialists and hearing healthcare professionals. Earlier intervention from a hearing care professional has the potential to turn a lifelong handicap into a long-term improvement in quality of life that benefits the public good.
Hearing Loss as a Multi-morbidity
Hearing loss is the second leading cause of years living with disability (YLD)—second only to depression.5 John Bakke, MD, of Zolo Healthcare Solutions, refers to acquired hearing loss of adult onset as a triple threat to patients [personal communication, July 27, 2013]:
1) Clinically significant hearing impairment is itself a disability, and is an indication for effective remediation in its own right;
2) Hearing loss interferes with a patient’s ability to be treated for other medical conditions because it hinders an individual’s ability to engage with physicians and understand treatment advice and directives; and
3) Emerging research suggests that hearing loss may actually accelerate some disabilities such as cognitive dysfunction and vestibular impairment.
The prevalence, co-morbidity, and disabling effects of hearing loss underscore the need for aggressive preventive programs that identify conditions such as hearing loss that threaten health outcomes.6 Hearing healthcare may be an emerging interventional discipline within medicine that has an important role in breaking the cycle of morbidity and mortality associated with a patient’s inability to hear. The treatment of hearing loss by audiologists and qualified professionals can provide interventional assistance by providing routine hearing evaluations for patients of “patient centered medical care homes” (PCMH) that seek to focus on prevention, early detection, and evidence-based treatment. This is likely to result in improved quality of care, patient compliance, improved outcomes, and reduced overall cost of care.
Audiologists and hearing instrument specialists are now being increasingly viewed within the wider medical community as an essential component of patient care for a broad range of disease processes, which, previously, were not considered relevant to hearing impairment. Examples of the value of interventional audiology being included in the comprehensive team of primary care-givers who seek to minimize impairment and maximize function include:
Dizzy patients. Lin and Ferrucci7 recently published research documenting the robust association between high frequency hearing loss and an increased risk of falls. The researchers found for every 10 dB increase in hearing loss, there was a 1.4-fold (95% CI, 1.3-1.5) increased odds of an individual reporting a fall over the preceding 12 months.7
Early interventional audiological assessment, as well as balance testing, may allow primary care physicians to prevent unnecessary falls, hospitalizations, and even death associated with complications of hip fracture and other fall-related trauma.
Diabetic patients. The diabetic patient is at greater risk due to neuropathies in the feet that may cause ataxic gait, and with a twofold increase in the risk of high frequency hearing loss.8 Physicians and hearing healthcare specialists may jointly counsel this patient type on preventive care strategies that intervene in possible trauma-related health concerns related to falls.
Why intervention? Hearing impairment is a hidden disability that is not visible to patients and their support systems, including physicians. Audiologists and other healthcare professionals would be wise to intervene in the care of individuals with medical conditions, and high-risk co-morbidities associated with a higher incidence of hearing loss.
Although there is a paucity of evidence from randomized controlled trials, early identification, remediation, and treatment of hearing loss are thought to lead to higher overall quality of life outcomes. Common sense requires hearing care professionals to educate physicians and other medical practitioners about the linkage between hearing impairment and numerous medical conditions. Let’s examine some of these co-morbid conditions in greater detail.
Understanding the PCP PerspectiveHearing care professionals need to recognize the challenge and obstacles associated with building referral networks with PCPs. Specifically, we must recognize the busy nature of a PCP’s practice. Most PCP practices see patients of all ages with a range of conditions, many of which can be life threatening. For the typical PCP, issues related to hearing loss will remain a relatively low priority; therefore, hearing care professionals need to be sensitive to the practice’s needs. This usually means that we must work directly with the office manager or lead nurse to ensure our message is being received. Due to the extremely busy nature of their schedule, hearing care professionals must package educational material so that it is specific and free of jargon and slant. The educational material needs to be in alignment with how PCPs absorb information, thus materials need to be evidence-based and translate research into quality patient care. Finally, the educational material needs to be delivered to the PCP in a familiar format, such as grand rounds or one-page summary sheets.
|
Hearing Loss and Cognitive Decline
By 2050, 1 in 30 Americans will suffer from dementia. It is thought that delaying the onset of dementia by 1 year could potentially reduce the incidence of dementia by 15%, thus saving billions of dollars in healthcare costs. Lin et al9 at John Hopkins University followed 1,984 individuals between the ages of 36 and 90 years of age. None of the participants had cognitive impairment as measured on standardized tests at the beginning of the study, while some of them did have hearing loss. The participants were followed over an 18-year period. The effects of age, medical risk factors, diabetes, and hypertension were controlled in the study design. Results of the study indicated that individuals with hearing loss have a greater risk of subsequently developing dementia than do individuals without hearing loss.
Specifically, Lin and colleagues9 found that study participants with hearing loss at the beginning of this longitudinal study have a 40% chance of a greater rate of cognitive decline compared to those with normal hearing at the beginning of the study. Additionally, the researchers surmise that a mild (25 dB) hearing loss equates to a 7-year cognitive decline. A by-product of Lin et al findings would be to encourage patients to have their hearing screened at an earlier age, and to actively participate in the appropriate auditory treatment program, if indicated, which may result in a lower incidence of clinically significant dementia.
Hearing Loss and Diabetes
Hearing loss is more than twice as common in adults with diabetes compared to those who do not have the disease, according to a new study funded by the National Institutes of Health (listen to the HR podcast, “Diabetes and Hearing Loss,” an interview with Kathleen E. Bainbridge, PhD, which aired in January 2009).8 About one-fifth (21%) of the diabetics surveyed had hearing loss, compared to only 9% of non-diabetics in this outcomes-based study, which controlled for other variables. Of the diabetics tested, 68% of them were found to have hearing loss in the higher frequencies. Lin et al10 also evaluated NIH data with a higher age cutoff and also showed that diabetics have about twice the prevalence of hearing loss (20%) in the US population compared to those who do not suffer from type 2 diabetes.
A certain degree of hearing loss is a normal part of the aging process for all of us, but it is often accelerated in patients with diabetes—especially if blood-glucose levels are not being controlled with medication, diet, and exercise. Some 85% of diabetics do not achieve their annual healthcare goals for hypertension, cholesterol, and blood sugar; poor patient compliance is problematic in this patient population, and may be enhanced by diabetics who cannot hear, thus reducing their engagement with their caregivers, and increasing the risk of further complications.
Henry Ford Hospital in Detroit conducted a study showing that women between the ages of 60 and 75 with poorly controlled diabetes had significantly worse hearing than those whose diabetes was controlled. Given these findings, diabetic patients and those at-risk for developing diabetes should have their hearing screened on an annual basis. Recently, the American Diabetes Association recommended that diabetics who suspect they may have a hearing loss contact their primary care provider, who may refer them to either an audiologist or a licensed hearing aid dispenser for a hearing screening.11
Hearing Loss and Smoking
Approximately 45 to 48 million Americans currently smoke, with female smokers slightly outnumbering male smokers. Current estimates suggest that approximately 60% of children in the United States are exposed to secondhand smoke each day.
Research indicates that smokers were 1.7 to 2.1 times as likely to have a hearing loss as non-smokers.12 Secondhand smoking also appears to have a deleterious effect on hearing, as individuals exposed to smokers have a 1.83 increased risk of sensorineural hearing loss compared to those not exposed to secondhand smoking.13
Research findings show that different mechanisms play a role in hearing loss due to exposure to smoking. The first may be related to tissue hypoxia (lack of oxygen); nicotine and carbon monoxide may actually deplete oxygen levels to the highly vascularized cochlea, which is bathed in electrolytic fluids. If oxygen is depleted, tissue damage can occur.14
The effect smoking has on hearing also appears to be correlated with the amount of cigarettes smoked. In a study conducted on Japanese office workers who smoke,15 the research showed that, as the number of cigarettes smoked per day and pack years of smoking increased, the risk of high frequency hearing loss increased in a dose dependent manner. In other words, the more people smoked each day and the longer they smoked, the worse the hearing damage—especially in the high frequency range. Smoking and secondhand smoke are associated with elevated pure-tone thresholds and an increased prevalence of both low and high frequency sensorineural hearing loss that is directly related to level of exposure.
Hearing Loss and Depression
Depression is also associated with the elderly patient suffering from acquired hearing loss. Jones and White16 conducted a meta-analysis on studies that examined the relationship between hearing loss and mental health. They concluded that individuals with hearing loss were more vulnerable to depression than people from the general population.
More recently, Garnefski and Kraaij17 examined the relationship between cognitive coping strategies, anxiety, depression, and acquired hearing loss. Their results suggested that maladaptive coping skills and symptoms of anxiety and depression are related issues among individuals with acquired hearing loss. Simply stated, patients with hearing loss tend to suffer more from the ill effects of depression and anxiety when compared to individuals with normal hearing. It seems that hearing loss adds to the complexity of the situation for patients suffering from these conditions. Given the paucity of studies in this area, however, further research is necessary to better understand the relationship between hearing loss, anxiety, and depression.
Hearing Loss and Aging-in-Place
The importance of interventional audiology goes beyond its relationship to chronic medical conditions. There are also lifestyle necessities requiring the practice of interventional hearing care.
The Centers for Disease Control and Prevention (CDC) defines “aging-in-place” as the ability to live in one’s own home and community safely, independently, and comfortably, regardless of age, income, or ability level.18 Of course, most adults would prefer to age in place; in fact, 78% of adults between the ages of 50 and 64 report that they would prefer to stay in their current residence as they age. One-third of American households are home to one or more residents 60 years of age or older.
People unable to age-in-place are more like to be socially isolated and may become institutionalized—thus becoming more of a drain on the current healthcare system, including Medicare and Medicaid. In fact, the CDC estimates that, in the year 2020, for Medicare beneficiaries who are admitted to hospital due to injuries resulting from an accidental fall, the hospitalization charges paid by Medicare average in the range of $9,113 to $13,507.
As Genther et al19 recently demonstrated, adults with hearing loss have a higher rate of hospitalization and poorer overall health. This data represents an enormous opportunity for hearing care professionals to intervene in the efficient delivery of services that maintain a higher quality of life for a large and growing population of people.
Considering the growing aging-in-place population and the fact that nearly 2 out of every 3 adults over age 70 have hearing loss, hearing healthcare providers certainly have a significant role to play in the aging-in-place movement, and it is reasonable to hypothesize that proper treatment of hearing loss in the elderly population may result in a higher percentage of that population being able to remain in their own homes until a more advanced age than would otherwise be the case.
Hearing Loss and Healthy Aging
Another sub-category of patients who could potentially benefit from interventional audiology services are healthy-agers. Unlike Baby Boomers—who are defined as those born between 1946 and 1964—healthy-agers are best described as individuals who want to live to be 100 in the mind and body of a 45-year-old, and they often are willing to spare no expense to accomplish this goal.
Since healthy-agers are defined by lifestyle needs and not year of birth, this segment of the population is comprised of people of various ages. The role of interventional audiology within the healthy-aging movement is to raise the awareness of the impact diet, nutrition, and physical fitness play on hearing acuity. Additionally, interventional audiologists could demonstrate to healthy-agers the use of downloadable apps, which can be used to improve hearing and overall cognitive function.
Implementation of Interventional Audiology in Your Clinic
Let’s examine some specific areas in which audiologists can work in partnership with physicians and other medical professionals to deliver preventive, interventional patient care. Because 80% of older adults make at least one annual physician visit and sections of the Affordable Care Act incentivize younger adults to see their healthcare provider for routine check-ups, it is imperative for audiologists to educate primary care physicians and physician assistants. By adapting an “educate to obligate” communication strategy between audiology and primary care medicine, audiologists can partner with physicians to provide more rapid and effective diagnosis and treatment of hearing loss. There are three broad categories of audiologist-primary care physician engagement: 1) education about the impact of hearing loss; 2) identification and screening; and 3) professional services and aural rehabilitation.
Getting Started: Ensure Successful OutcomesEnsure that the culture of your practice is devoted to providing comprehensive hearing care services, including aural rehabilitation. Physicians must be given the proper signal that your practice exudes quality, and this starts with your ability to deliver complete care in a trusting and nurturing environment. Failure to deliver on this first step is likely to stymie any success with development of a physician referral network. To see if your office is signaling a culture of quality and excellence, contact the authors to find your Total Quality Score.
|
Education on Impact of Hearing Loss
Physicians must be educated about the impact hearing loss has on their ability to deliver effective care. Systematic, evidence-based targeted education of PCPs is the most fundamentally important component of implementation of interventional audiology. Given that most PCPs have had very little formal training on the consequences of untreated hearing loss, the education process must begin by raising awareness with the PCPs in your area. In short, PCPs need to know that untreated hearing loss impacts their own clinical effectiveness with patients suffering from hearing impairments. Some of the aspects of patient-physician communication affected by hearing loss include:
• Review of medication use, dosage, etc;
• Cognitive assessment when dementia or other cognitive deficits are suspected;
• Communicate key components of a treatment plan or follow-up care ;
• Discussion of palliative care and end of life issues;
• Cognitive or depression screenings as part of routine practice or in advance of a surgical procedure.
A miscommunication because of hearing loss during any of these routine patient-physician interactions may result in the inefficient delivery of care, which undoubtedly increases costs, but may result in catastrophic consequences—even death.
In regard to education of physicians, audiologists and others within the hearing care industry have a twofold responsibility:
1) Educate the medical community about the potential catastrophic consequences of untreated hearing loss.
2) The co-morbid relationship hearing loss has to the chronic conditions mentioned previously.
Educating the community is another important component to interventional audiology. In addition to the use of traditional newsletters, social media and websites are useful educational tools that raise awareness within the community of the consequences of untreated hearing loss, especially among the chronically ill. A practice’s website can be designed to meet the lay public’s educational needs, as well as primary care medicine’s, with the goal of informing physicians about their interventional capabilities.
Audiologists and hearing instrument specialists may seek to present the latest preventive and interventional treatment strategies to the medical community through presentations at hospital grand rounds, and at primary care physician teaching institutions. Educational opportunities that seek to provide hearing health educational programs can be offered in partnership with the American Diabetes Association, the American Cancer Society, and the American Lung Association. Professionals also can attend, display, and educate at cardiology, pulmonology, endocrinology, neurology, trauma, geriatric, and other physician specialty conferences, so that we begin to engage in a more effective partnership with medicine, and intervene where it is medically appropriate.
Identification/Screening
The second component to implementing an interventional audiology program in your practice is the ability to conduct routine hearing screening. Currently, the Preventive Services Task Force (PSTF) does not support hearing healthcare screening. This statement, along with other factors mentioned below, makes it challenging for hearing care professionals to move PCPs toward conducting hearing screening in their practices. Despite the position of the PSTF, audiologists may find themselves advising PCP practices in the implementation of an adult hearing screening program.
Due to the evolution of digital technology, accurate hearing screenings now can be conducted in an automated fashion using tablet computers or apps on a smartphone. Before using any of these computer-based hearing screening technologies, practitioners are urged to evaluate their reliability and accuracy. When establishing a screening program within a medical practice, there are 6 W’s that need to be thoughtfully considered:
Who does the screening? If it is not feasible for the hearing care professional to conduct the screening in the primary care physician’s office, a nurse or medical office assistant needs to be trained to conduct the screening or oversee it. Even automated tools (eg, Ultimate Kiosk system) require the presence of someone to monitor them.
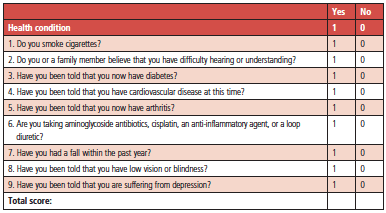
Who gets screened? It is probably not feasible to conduct the hearing screen on every patient examined by the PCP, even all patients over age 65. We recommend the use of a co-morbidity risk assessment, like the example designed by Weinstein,20 shown in Figure 1. This assessment can be added to a routine patient intake form, and medical assistants can be instructed to refer anyone with a score of 2 or higher, as this score indicates that hearing loss is more likely to be identified in these patients.
|
| Figure 1. The multifactorial risk assessment created by Weinstein.20 Reprinted with her permission. |
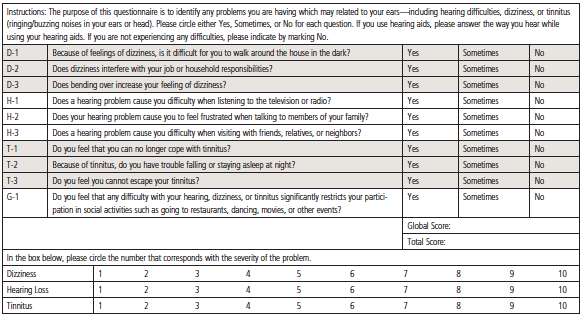
What screen is used? After consideration of who conducts the screening, as well as the target population, the next detail is to determine what screening tool you will use. There are many choices from smartphone apps (eg, uHear) to handheld devices to automated hearing screening programs placed on a tablet computer. In addition, practitioners may decide to forego a pure-tone screening and use any number of pencil and paper questionnaires. The 10-item Screening for Otologic Functional Impairments (SOFI)6 can be used to identify patients likely to be suffering from hearing loss (Figure 2). The SOFI is high in reliability, valid, and highly correlated with similar hearing handicap self-reports.20 Another pen and paper screening tool that has been validated is the Quick Hearing Check,21,22 which can be found at the Better Hearing Institute website: http://www.betterhearing.org/press/pdfs/QuickHearingCheck.pdf
|
| Figure 2. Screening Otologic Function of Older Adults (SOFI).6,20 Reprinted with permission. |
Where does the screening occur? A separate consideration is where the hearing screening will take place. Some of the choices include in an examination room, in a reception area, or even from the comforts of home if an app or questionnaire is used. Locations need to be chosen that minimally impact the normal workflow of a busy practice.
When does the screening occur? Another consideration is when the hearing screening should be conducted. Options include before or after the patient’s visit with the PCP.
What is the referral process? Perhaps the most critical question: you must determine the process in which patients who fail the screening are referred to the hearing care practice. Some of the considerations include the establishment of pass/fail criteria, scheduling an appointment to see the audiologist for a comprehensive assessment, and the manner in which follow-up reports are sent back to the patient’s primary care physician.
Professional Services and Aural Rehabilitation
As Lin25 stated, “Contrary to popular perceptions, proper hearing rehabilitative treatment is complex, does not simply consist of hearing aid use, can vary substantially depending on the treating audiologist.” This strongly suggests that audiologists and hearing instrument specialists must offer comprehensive and personalized aural rehabilitation services, if they want to develop viable partnerships with physicians.
Additionally, the entire profession needs to put into practice evidence-based clinical standards to ensure high-quality outcomes, as this will further enhance our professional credibility with PCPs. This process starts with educating PCPs on the comprehensive nature of the services a modern practice offers, including:
• Computer-based auditory training;
• Apps that allow patients to conduct auditory training exercises on their own;
• Aural rehabilitation classes, both group and individual;
• Comprehensive hearing aid orientation services;
• A choice of service packages that are bundled with product offerings;
• Consistent use of an evidence-based clinical protocol; and
• Use of self-report measures that document patient outcomes.
An “All Hands on Board” Approach NeededYou don’t necessarily need to be a licensed audiologist to deliver interventional audiology care to the growing number of individuals requiring integrative and preventive care. Licensed hearing instrument specialists who possess the following are a good fit for an interventional care model: • Maintain a strong referral network with audiologists and physicians. • Provide comprehensive services, including aural rehabilitation and auditory training. • Follow IHS best practice standards and code of ethics.
|
Change Is Inevitable, Transformation Is Optional
Interventional audiology requires that audiologists and others associated with the care of hearing-impaired individuals change their orientation toward patient care. Rather than centering on the dispensing of a hearing aid/medical device, interventional audiology revolves around the disease state of hearing loss and its relationship to the chronic medical conditions listed here.
In order for the interventional hearing healthcare professional to become a valuable and respected member of the physician’s preventive care team, several items and procedures are needed. These are listed in the sidebar labelled “Components of an Interventional Audiology Tool Kit.” Notice there are three distinct phases of interventional audiology: 1) awareness; 2) identification; and 3) treatment/follow-up. Table 1 lists the tasks and procedures that many audiologists currently don’t process, but are necessary to successfully implement an interventional audiology strategy.
Chronic diseases are the most costly health problem in the United States.23 The conditions mentioned in this article have evidence indicating a higher rate of hearing loss associated with them. Thus, hearing care professionals need to be directly involved in all phases of identification and remediation. The process must begin with a dedicated effort on the part of every audiologist and hearing instrument specialist to educate PCPs, as many of them lack the appropriate knowledge base to effectively identify patients with hearing loss and its ramifications for quality of life and successful outcomes.24
The broader negative consequences of hearing loss, particularly in older adults, are now beginning to surface. It is the responsibility of audiologists to draw attention to this using the best available evidence. This paper is intended to offer some preliminary guidance, foster the beginning of dialogue, and offer some first steps on a journey toward interventional hearing care for patients of all ages. It is in the best interest of the primary care physician, of the hearing healthcare professions, and certainly in the best interest of the patient’s quality of life.
Components of an Interventional Audiology Tool KitEducation/Awareness • Website and social media that provide data on the relationship of hearing loss to various chronic diseases, including links to patient organizations • Informational newsletters with latest evidence on the disease state of hearing loss, delivered to physicians on a monthly basis • Public lectures for the community that discuss disease state of hearing loss and what to do about it • Clinical processes and patient materials that facilitate the practice of healthy hearing behaviors • Evidence-based educational materials on the disease state of hearing loss that can be personally delivered to physicians • Use of a referral form like the one in the addendum Identification/Screening • Multifactorial risk assessment form6 • SOFI questionnaire20 • Use of a comprehensive case history form that asks patients about chronic diseases associated with hearing loss • Referral network of physicians that specialize in various chronic diseases • Detailed reports back to referring physicians, outlining auditory assessment outcome and comprehensive treatment options Treatment and Follow-up • Comprehensive habilitation services, aural rehabilitation programs—beyond simply dispensing hearing aids • Active participation in the health and wellness of patients, including providing support on healthy diets and exercise, consistent with regimens recommended by their physician
|
References
1. Vaillant G. Triumphs of Experience: The Men of the Harvard Grant Study. Cambridge, Mass: Harvard University Press; 2012.
2. Weiss CO, Boyd CM, Yu Q, Wolff JL, Leff B. Patterns of prevalent major chronic disease among older adults in the United States. JAMA. 2007;298(10):1160-1162.
3. Anderson G. Chronic care: making the case for ongoing care. Princeton, NJ: Robert Wood Johnson Foundation; 2010. Available at: www.rwjf.org/files/research/50968chronic.car:chartbook.pdf
4. Tinetti M, Fried TR, Boyd CM. Designing health care for the most common chronic condition—multimorbidity. JAMA. 2012;307(23):2493-2494.
5. Mathers C, et al. Global burden of hearing loss in the year 2000. Geneva: World Health Organization; 2003. Available at: www.who.int/heathcareinfo/statsitics/bod_hearingloss.pdf
6. Weinstein B. Screening for otological functional impairments in the elderly: whose job is it anyway? Audiol Res. 2011;1(e12):42-48.
7. Lin F, Ferrucci L. Hearing loss and falls among older adults in the United States. Arch Intern Med. 2012;172(4):369-371.
8. Bainbridge KE, Hoffman HJ, Cowie CC. Diabetes and hearing impairment in the United States (NHANES). Ann Intern Med. 2008;149(1):1-10.
9. Lin FR, Yaffe K, Xia J, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. 2013;173(4):293-299.
10. Lin FR, Niparko JK, Ferrucci L. Hearing loss prevalence in the United States. Arch Intern Med. 2011;171(20):1851-1853.
11. Taylor B, et al. Diabetes: a roundtable discussion. Audiology Practices. 2013;5(3):18-22.
12. Cruickshanks KJ, Klein R, Klein BEK, Wiley TL, Nondahl DM, Tweed TS. Cigarette smoking and hearing loss: the epidemiology of hearing loss study. JAMA. 1998;3(279):21.
13. Lalwani AK, Liu YH, Weitzman M. Exposure to secondhand smoke associated with hearing loss in adolescents. Arch Otolaryngol Head Neck Surg. 2011;7:655-662.
14. Katbamna B. Effects of smoking on the auditory system (2009). Available at: http://www.audiologyonline.com/articles/effects-smoking-on-auditory-system-899
15. Nakanishi N, Okamoto M, Nakamura K, Suzuki K, Tatara K. Cigarette smoking and risk for hearing impairment: a longitudinal study in Japanese male office workers. J Occup Environ Med. 2000;42(11):1045-1149.
16. Jones E, White A. Mental health and acquired hearing impairment: a review. Br J Audiol. 1990;24:3-9.
17. Garnefski N, Kraaij V. Cognitive coping and goal adjustment are associated with symptoms of depression and anxiety in people with acquired hearing loss. Int J Aud. 2012;51:545-550.
18. Older American 2010: Key Indicators of Well-Being. Federal Interagency Forum of Aging-Related Statistics. Washington, DC: US Government Printing Office; July 2010.
19. Genther D. Association of hearing loss with hospitalization and burden of disease in older adults. JAMA. 2013;12(309):22.
20. Weinstein B. Tool kit for screening otologic function of older adults. Am J Audiol. 2013;22:179-182.
21. Koike J, Hurst MK, Wetmore SJ. Correlation between the American Academy of Otolaryngology-Head and Neck Surgery five minute hearing test and standard audiological data. Otolaryngol Head Neck Surg. 1994;111:625-632.
22. Kochkin S, Bentler R. The validity and reliability of the BHI Quick Hearing Check. Hearing Review. 2010;17(12):12-28. Available at: /practice-management/17042-the-validity-and-reliability-of-the-bhi-quick-hearing-check
23. Wu SY, Green A. Projection of chronic illness prevalence and cost inflation. Santa Monica, Calif: Rand Health; 2000.
24. Johnson C, Danhauer JL, Koch LL, Celani KE, Lopez IP, Williams VA. Hearing and balance screening and referrals for Medicare patients: a national survey of primary care physicians. J Am Acad Audiol. 2008;19:171-190.
25. Lin FR. Hearing loss in older adults: who’s listening? JAMA. 2012;307(11):1147-1148.
CORRESPONDENCE can be addressed to Dr Taylor at: [email protected]
Citation for this article: Taylor B, Tysoe B. Interventional Audiology: Partnering with physicians to deliver integrative and preventive hearing care. Hearing Review. 2013;20(12):16-22.