Why is it so difficult to predict patient outcomes?

|
| Mary Cord, AuD, is a research audiologist at Walter Reed Army Medical Center in Washington, DC; Deniz Baskent, PhD, and Sridhar Kalluri, PhD, are research scientists at the Starkey Hearing Research Center in Berkeley, Calif; and Brian C. Moore, PhD, is professor of auditory perception at the University of Cambridge in England. |
Better predictions of outcomes would help clinicians and patients develop more realistic expectations of improved communication ability, ultimately resulting in increased success and satisfaction with amplification.
For most hearing aid users, the primary reason for using amplification is to improve speech understanding. Thus, clinicians often use tests of speech recognition ability to assess hearing aid benefit. It seems reasonable to assume that the benefit measured in the clinic will relate to the benefit the patient will obtain in everyday life. However, clinical assessments of hearing aid performance are often not highly predictive of performance in the real world.1-4
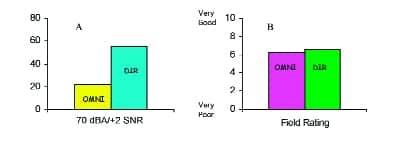
This is especially true with regard to speech understanding in noise. As an example, Figure 1 shows the results of a clinical study that assessed patient performance with directional microphone hearing aids.5 A total of 40 hearing-impaired adults were evaluated with a clinical measure of speech understanding in noise using both the omnidirectional and directional microphone settings of their hearing aids. The clinical test results (Figure 1a) showed a substantial advantage for the directional microphone when listening to speech in noise. The patients were then sent home and instructed to compare the two settings in their everyday lives. When the patients returned to the clinic 1 month later, they were asked to provide a subjective rating of their speech understanding ability in noise with each of the two microphone settings (Figure 1b). It was apparent that the substantial directional microphone performance advantage measured in the clinical testing was not perceived by the patients in everyday listening environments.
|
| FIGURE 1. Average performance measured in the clinic (left, 1a) and patients’ subjective ratings of performance (right, 1b) with omnidirectional and directional microphones. |
This presents a big problem. Based on the speech-in-noise testing, the patient may leave the clinic with very high expectations of the benefit for the directional setting, only to be disappointed when using the hearing aids in real-world noisy environments. This may ultimately lead to rejection of the hearing aids because they did not meet the patient’s expectations. Why does this discrepancy exist between benefit observed in the clinical test environment and the benefit perceived by the hearing aid user in everyday life?
Clinic Versus Real World
Most obvious, perhaps, is the fact that real-life listening situations may be very different from controlled clinical test conditions.5 In contrast to the static clinical test environment, real-life situations may involve talkers and listeners who are moving around and variations in environmental noise sources and levels. Interactions may occur between certain types of hearing aid signal processing and the listening environment. For example, in the case of directional microphone hearing aids, the effectiveness of directionality is diminished as the distance between the signal and the listener increases, as reverberation increases,6,7 and as the spatial separation of the signal and noise decreases.8
Interactive conversation may involve more complex cognitive functioning than clinical speech-in-noise tests. While trying to follow what is being heard, the listener may also simultaneously be processing and storing information in memory and thinking about how to respond to what is being said.9,10 The clinical test situations in which we assess speech recognition may be more or less difficult than those experienced by hearing aid users in the real world,3,11 making it problematic to determine the extent to which the benefit demonstrated in the clinic translates to real-life listening environments.
Visual cues. Many everyday situations involve face-to-face communication, with visual speech cues available to the listener. In the clinic, we typically test in an auditory-only modality. Visual speech cues may provide as much or more useful speech information than does amplification, and visual cues and hearing can interact to effectively reduce background noise by up to 8 dB.12 Some patients may rely on and benefit more from visual cues than others.13 Also, when visual information is available, low-frequency auditory cues become more important than when such information is not available.14 Thus, auditory-only testing in the clinic may not be highly predictive of an individual’s performance in real-world auditory-visual situations.
Aging. Older people often have a harder time than young people adjusting to amplification,15 which may be reflected in poor subjective outcomes, even if the hearing aids are providing good objective benefit in clinical testing. Also, for some older patients, visual problems may appear to be “hearing problems.” As visual disorders (eg, macular degeneration) develop, a decreased ability to communicate may be interpreted as decreased hearing ability, since visual speech cues are no longer being received clearly. Additionally, older patients may experience cognitive declines that will affect hearing aid outcomes.16
Listening effort. Hearing loss may be a risk factor for fatigue and mental distress.17 Patients often report being less tired and stressed at the end of the day once they begin using hearing aids. It appears that hearing aids not only improve the ability to hear more speech, but may also allow the listener to hear speech more easily.9,18,19 A patient may report significant benefit from the hearing aids because he or she is expending less effort to hear in everyday listening environments, even if the clinical performance measures do not show large benefits. Similarly, clinical performance measures may not adequately reflect other possible effects of hearing aids, such as processing unattended sounds.20
Individual differences. Substantial intersubject variability is a consistent finding in hearing aid outcomes research.21 This is likely due to the multitude of factors that may influence performance with hearing aids and that may interact with one another in unique ways for each patient. In addition to the underlying physiology of hearing loss that might differ from one patient to another, hearing aid benefit may be influenced by a number of variables such as personality, motivation, attitude toward hearing aids, readiness to accept change, educational level, overall health status, the “auditory ecology” of the patient,22 and prior hearing aid experience.
Signal-to-noise ratio (SNR) loss. People with similar hearing loss may differ widely in their ability to understand speech in background noise,23,24 and a number of researchers have suggested that individual differences in susceptibility to noise interference (SNR loss) may be a primary factor in explaining why hearing-impaired individuals obtain varying degrees of benefit from hearing aids.24-27 However, to date, no clear relationship has been found between objective speech-in-noise measures and success with hearing aids.
Recently, Nabelek and her colleagues28 reported on a variation of an SNR loss measure that results in a subjective estimate of the SNR at which a listener is comfortable listening to speech in noise. The acceptable noise level (ANL) is the difference between the most comfortable listening (MCL) level for quiet speech and the level of the maximum background noise that the patient is willing to accept while listening to speech presented at the MCL. It appears that the more noise an individual can tolerate, the more likely he or she is to be successful with amplification. These researchers were able to classify the participants in this study as successful or unsuccessful hearing aid users with 85% accuracy using ANL as a predictive measure.
Saunders and Cienkowski29 developed the Performance-Perceptual Discrepancy (PPDIS) test that evaluates a listener’s actual SNR for 50% performance in noise, and their perception of the SNR at which he or she can just follow the speech. The difference between the performance score and the perceptual score gives a measure of the extent to which the listener misjudges his or her hearing ability. This procedure correctly classified 75% of the study participants as “contented” or “discontented” hearing aid users, with discontented users believing they need a better SNR to hear than they really do.
Summit Recommendations
There are a number of significant challenges to solving the problem presented by the disparity between clinical and real-world hearing aid performance:
- Find ways to bring real-world conditions into the clinic. Datalogging hearing aids now allow this to be done to a limited degree by providing some information about the way a patient uses a hearing aid and the general types of listening environments encountered by the patient. Future advances may make it possible to expand datalogging to include audio recordings of problematic listening situations. This would allow the clinician to better understand the specific problems the patient is facing so that fine-tuning adjustments and/or counseling could be tailored to meet individual needs. Also, with advances in technology, virtual reality may allow patients to interact with a computer-simulated environment similar to the real world, and allow clinicians to obtain performance measures that are predictive of real-world benefit.
- Give greater control of hearing aid fine-tuning to the patient. “Self-learning” or “trainable” hearing aids that fine-tune themselves would reduce the amount of time the clinician must spend tweaking hearing aid parameters in response to a patient’s oftentimes vague complaints. Some hearing aids currently on the market have a trainable volume control, which adapts over time to the levels the listener prefers. It is possible that algorithms will be developed that give control over other fitting features (noise reduction, directionality) and parameters (compression, attack and release times) to the user, so that the fitting could be individualized to specific preferences in troublesome listening environments.
- Develop a clearer understanding of the audiological and nonaudiological factors that can influence hearing aid outcomes. The numerous audiological and nonaudiological variables, which may interact in complex ways for different patients, make it difficult for the clinician to predict benefit. More research is needed to understand how to quantify the influence of these factors and how they interact with one another for individual patients.
- Understand the relationship between SNR and patient satisfaction. Conduct additional research to determine the clinical utility of subjective SNR measures (such as ANL and PPDIS tests) as predictors of success with amplification.
- Explore the use of performance measures that assess cognitive effects, such as listening effort, in addition to measures of speech intelligibility. It may be important to consider perceived effort when evaluating hearing aid benefit. Measures of perceived effort, in combination with objective speech recognition testing, may provide a more complete picture of the amount of benefit an individual derives from amplification.30-32
If dispensing professionals had more accurate means for predicting how patients perform with hearing aids in everyday living, rehabilitation strategies could be tailored to more precisely meet their individual needs. Better predictions of outcome would help the clinician and the patient develop realistic expectations for improved communication ability, and ultimately result in increased success and satisfaction with amplification.
References
- Haggard MP, Foster JR, Iredale FE. Use and benefit of postaural aids in sensory hearing loss. Scand Audiol. 1981;10:45-52.
- Cox RM, Alexander GC. Maturation of hearing aid benefit: objective and subjective measurements. Ear Hear. 1992;13:131-141.
- Bentler RA, Niebuhr DP, Getta JP, Anderson CV. Longitudinal study of hearing aid effectiveness. II: subjective measures. J Speech Hear Res. 1993; 36: 820-831.
- Valente M, Fabry D, Potts L, Sandlin R. Comparing performance of the Widex Senso digital hearing aid with analog hearing aids. J Am Acad Audiol. 1998; 9:342-360.
- Walden BE, Surr RK, Cord MT, Edwards B, Olson L. Comparison of benefits provided by different hearing aid technologies. J Am Acad Audiol. 2000;11:540-560.
- Hawkins D, Yacullo W. Signal-to-noise ratio advantage of binaural hearing aids and directional microphones under different levels of reverberation. J Speech Hear Disord. 1984;49:278-286.
- Ricketts TA, Dittberner AB. Directional amplification for improved signal-to-noise ratio: strategies, measurement, and limitations. In: Valente M, ed. Strategies for Selecting and Verifying Hearing Aid Fittings, 2nd edition. New York: Theime; 2002:274-345.
- Leeuw AR, Dreschler WA. Advantages of directional hearing aid microphones related to room acoustics. Audiol. 1991;30: 330-344.
- Edwards B. The future of hearing aid technology. Trends in Amplif. 2007;11: 1-15.
- Sweetow R, Henderson-Sabes J. The case for LACE (Listening and Communication Enhancement). Hear Jour. 2004;57: 32-38.
- Mueller GH. Do hearing aids work in noise? That’s a simple question with no easy answer. Hear J. 1995;48(8):13-26.
- Grant KW, Walden BE, Cord MT. Should visual cues (speechreading) be considered when fitting hearing aids? Paper presented at: Meeting of the Acoustical Society of America; 2002; Pittsburgh.
- Walden BE, Prosek RA, Worthington DW. Predicting audiovisual consonant recognition performance of hearing-impaired adults. J Speech Hear Res. 1974;17:270-278.
- Walden BE, Grant KW, Cord MT: Effects of amplification and speechreading on consonant recognition by persons with impaired hearing. Ear Hear. 2001;22:333-41.
- Rupp RR. Predicting hearing aid use in maturing populations: the feasibility scale. Hear Aid J. 1982;January.
- Pichora-Fuller MK, Singh G. Effects of age on auditory and cognitive processing: implications for hearing aid fitting and audiologic rehabilitation. Trends in Amplif. 2006;10:29-59.
- Kramer SE, Kapteyn TS, Houtgast T. Occupational performance: comparing normally-hearing and hearing-impaired employees using the Amsterdam Checklist for Hearing and Work. Intl J Audiol. 2006; 45: 503-12.
- Sarampalis A, Kalluri S, Edwards BE, Hafter ER. Cognitive effects of noise reduction. Paper presented at: International Hearing Aid Research Conference; 2006; Tahoe City, Calif.
- Baer T, Moore BCJ, Gatehouse S. Spectral contrast enhancement of speech in noise for listeners with sensorineural hearing impairment: effects on intelligibility, quality and response times. J Rehab Res Dev. 1993; 30:49-72.
- Rivenez M, Darwin CJ, Guillaume A. Processing unattended speech. J Acoust Soc Am. 2006; 119:4027-4040.
- Kricos PB. The influence of nonaudiological variables on audiological rehabilitation outcomes. Ear Hear. 2000; 21(Suppl): 7S-14S.
- Gatehouse S, Naylor G, Elberling C. Linear and nonlinear hearing aid fittings. 2. Patterns of candidature. Intl J Audiol. 2006; 45:153-171.
- Nabelek AK, Pickett JM. Monaural and binaural speech perception through hearing aids under noise and reverberation with normal and hearing-impaired listeners. J Speech Hear Res. 1974; 17:724-39.
- Crandell CC. Individual differences in speech recognition ability: implications for hearing aid selection. Ear Hear. 1991; 12(Suppl):100S-108S.
- Plomp R. Auditory handicap of hearing impairment and the limited benefit of hearing aids. J Acoust Soc Am. 1978; 63: 533–549.
- Dirks DD, Morgan DE, Dubno JR. A procedure for quantifying the effects of noise on speech recognition. J Speech Hear Disord. 1982; 47: 114-23.
- Killion MC. Hearing aids: past, present, future: moving toward normal conversations in noise: Br J Audiol. 1997; 31: 141-8.
- Nabelek AK, Freyaldenhoven MC, Tampas JW, Burchfiel SB, Muenchen RA. Acceptable noise level as a predictor of hearing aid use. J Am Acad Audiol. 2006; 17: 626-39
- Saunders GH, Cienkowski KM. A test to measure subjective and objective speech intelligibility. J Am Acad Audiol. 2002; 13: 38-49.
- Hallgren M, Larsby B, Lyxell B, Arlinger S. Speech understanding in quiet and noise, with and without hearing aids. Intl J Audiol. 2005; 44: 574-583.
- Larsby B, Hallgren M, Lyxell B, Arlinger S. Cognitive performance and perceived effort in speech processing tasks: effects of different noise backgrounds in normal-hearing and hearing-impaired subjects. Intl J Audiol. 2005; 44: 131-43.
- Humes LE. Dimensions of hearing aid outcome. J Am Acad Audiol. 1999; 10: 26-39.

|
| “Addressing the Special Needs of Older Adults.” by Vishakha Rawool, PhD. |
Correspondence can be addressed to HR or Mary Cord, Walter Reed Army Medical Center, 6900 Georgia Avenue NW, Washington, DC 20307-5001; .



-300x264.gif)

