Your next patient is about to walk through the door for a hearing aid evaluation appointment. You have your pen, audiogram, blank chart, and clipboard ready, and you are about to take a detailed case history. You want to understand the motivation behind your patient’s visit when he or she comes through the door today. Naturally, you want to provide the best technology and professional service that your education and years of experience have taught you. You want to fit the hearing instrument to provide audibility and comfort for all of the environments in which your patient wants to use the hearing instruments. How can you integrate the information about the client into the fitting process?
Even though hearing aid fitting technology has evolved tremendously, it is still necessary to identify and address the fundamental communication goals of the user. To assume that two individuals with similar audiograms can be fitted with identical hearing aids and require the same program allocation, settings, and counseling is a gross oversimplification. A successful hearing aid fitting means more than just providing the latest technology.
Patient Satisfaction and Identifying Patient Needs
Through his MarkeTrak research, Kochkin1 states that one of the strong drivers of customer satisfaction is the ability of the hearing instrument to provide reliable, high-quality sound across multiple listening environments. Kochkin has shown that hearing aid users are more satisfied when their instruments provide overall hearing improvement, whereas low satisfaction ratings are seen when the instrument only improves hearing in some situations.2
This information tells us that everyone has different communication needs based on their lifestyles. More importantly, patients expect their hearing instruments to work optimally in the environments that are important to them.
Since customer satisfaction is strongly associated with the benefit gained from the hearing instrument in a variety of listening environments, it is imperative that the hearing care professional learn more about the lifestyle of each patient. The patient’s lifestyle has many dimensions, and consequently, the needs and priorities of individuals differ significantly. How often is the patient in greatly varied acoustic environments? What are the communication needs in these different situations?3 What are the patient’s goals in each situation?
Identifying Needs
According to Cox,4 health care is shifting from a provider-driven to a payer/consumer-driven service. As a result, our patients are becoming more educated about their health care options, especially through the Internet, and are searching for their own solutions. In a broader sense, there is an emerging worldwide consensus about the needs of people with physical impairments. The recent International Classification of Functioning and Disability5 put forth by the World Health Organization represents a fundamental change in the way impairments such as hearing loss are viewed. In contrast to the old medical model, functioning and disability are now seen as a complex relationship between the health condition (eg, hearing impairment) and contextual factors, such as environment and personal variables that interact to influence the person’s level of functioning.
The new model focuses on how the patient’s hearing impairment affects specific activities (eg, communicating in a noisy environment), and how activity limitations in turn affect the individual’s participation in society (eg, restricted social activities). Simply put, we need to consider hearing loss from the patient’s perspective. How does a hearing loss affect the individual’s day-to-day functioning, and how does it affect his or her lifestyle? As hearing care professionals, we are constantly trying to assess the needs and interpret the goals of our patients in order to provide appropriate amplification technology and counseling.
Guidelines for the management of hearing loss in adults have recommended that the selection and provision of hearing aids should involve an assessment of the effects of the hearing loss on the patient’s lifestyle.6,7 There are numerous tools that can be utilized to achieve this. One well-researched and widely accepted tool is the Client Oriented Scale of Improvement (COSI™),8,9 developed by Harvey Dillon and his colleagues at the National Acoustic Laboratories in Australia. A major function of this tool is to record five realistic communication goals as specifically as possible. For example, to state “I want to hear my wife better at the noisy local seafood restaurant,” is better than “I want to hear well in noise.”9 The COSI can also reveal any unrealistic goals, and the hearing care professional can counsel and explain why these goals may either be out of the question or not reachable with the degree of success the patient expects.
Therefore, the hearing care professional needs to invest the time and have the skill to discover the areas most important to the patient, where the hearing instrument must perform optimally. For many hearing care professionals, this process of discovering patient needs may be second nature. For others, it may be difficult if no context is provided. By having realistic goals, it is easier for both the hearing care professional and the patient to be partners in the rehabilitation process and evaluate how successful the process has been. The hearing care professional is able to develop a closer professional relationship with the patient, which should be beneficial to both parties.
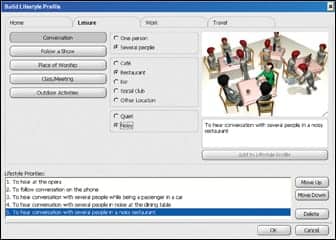
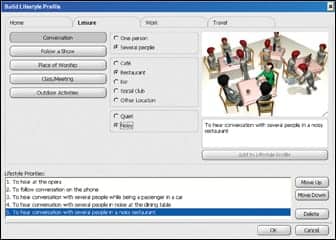
The Lifestyle Profile (Figure 1) is a software tool developed by Bernafon. It builds on the research and work conducted on the COSI and provides a structured framework for the quick identification and prioritization of a patient’s important communication goals. The Lifestyle Profile should be used at the initial appointment just like a case history that health care professionals do every day. It is divided into four main categories—home, leisure, work, and travel—reflecting the various dimensions of a person’s lifestyle.
|
| FIGURE 1. The structured framework of the Lifestyle Profile, offering possible options to build and then prioritize the communication needs of the client. |
This format assists the hearing care professional in choosing the appropriate questions to ask to discern a patient’s particular priorities in a systematic and efficient manner. The Lifestyle Profile is very comprehensive, with more than 200 billion possible combinations. It is, however, designed for easy use. Just choose the situation and goals under each category, then select what is most applicable to the patient. It is also possible to enter manually a “write-in” goal not seen in the software and rank it in importance among all the patient’s other communication goals.
Benefits of Identifying Needs
Identifying specific listening needs is essential at the initial stages of any rehabilitation program. Hearing care professionals should use this information to recommend the most suitable hearing instrument technology to meet the patient’s needs. In this way, dispensing professionals can gain greater insight into the expectations of their patients and counsel them appropriately.
The result is patients who feel that their concerns are acknowledged and understood, which builds rapport and trust. The Lifestyle Profile is designed to improve the level of communication between the patient and the hearing care professional. Taylor10 states that it is this interaction that is the most important driver of overall patient satisfaction.
I’ve Identified Their Needs. Now What?
After identifying and documenting the primary needs of the client, the hearing care professional needs to tailor the hearing instrument to work optimally in environments most important to the patient. Achieving each client’s goals with a customized formula usually involves creating dedicated listening programs and maximizing the appropriate features. We can see how this works using examples of the two hypothetical patients who have identical hearing losses:
Patient Smith, 49-year-old businessman. Mr Smith is constantly on the phone and in meetings with his staff and customers. These meetings, with one or several people, usually take place over lunch in restaurants, which may be quiet or noisy. He also socializes with customers and friends on the golf course, and he is passionate about music, attending a concert each month. Naturally, Mr Smith expects his hearing instrument to work in these listening environments.
Patient Jones, 49-year-old part-time mechanic. Mr Jones is responsible for conducting listening checks on engines and detecting any faults. His workplace, where he receives verbal instructions from his colleagues and customers, is quite noisy. Mr Jones also drives a taxi and frequently converses with his passengers. He is married and takes his wife to their favorite restaurant every Sunday night. He expects his hearing instrument to work in these listening environments.
Despite having identical hearing losses, Mr Smith and Mr Jones have lifestyles and specific communication goals that are incredibly different. Fitting them with instruments programmed identically would not meet their individual—and very different—needs.
Offering only one listening program for use in all listening environments would not provide an optimum outcome. Depending on the patient’s environment and the communication goals within that environment, dedicated listening programs may be needed to offer the best amplification response. For example, speech and music have very different spectral, temporal, and intensity qualities, and therefore, the hearing instrument should deliver different frequency responses and time constants to maximize the response.
But what if the patient wants to hear speech in a car, as does Mr Jones? In this case, a directional microphone might be detrimental because the speaker is seated behind or to the side of the patient. In addition, as a mechanic, Mr Jones needs to hear engine sounds. In his program, adaptive noise reduction should be inactive, with the instrument in omnidirectional mode, to ensure audibility of the signal. Only separate programs with specific active features can handle all of these communication goals effectively.
Using the Patient’s Lifestyle Profile To Program Hearing Aids
The advancement of hearing aid technology has introduced a heightened level of fitting complexity. Instruments are now equipped with sophisticated features to manage several different environments—in either one dedicated program or several specialized programs. As a consequence, hearing care professionals have to understand the functionality of these new features and how to manage them in the fitting software. In turn, they must somehow translate the often cryptic comments and wishes of their patients into parameter actions. In some cases, it may take numerous follow-up appointments to deliver the optimum response.
To reduce confusion when creating a customized instrument, the Lifestyle Profile will directly influence the initial settings of ICOS, Bernafon’s premium hearing instrument family. The Lifestyle Profile automatically establishes dedicated listening programs, with the appropriate adaptive features and settings configured to meet the specified listening goals of each patient—based solely on the patient’s communication needs shown in the Lifestyle Profile (Figure 1).

|
| FIGURE 2. The automatically assigned program allocations for Mr Smith (top) versus the program allocations for Mr Jones (bottom), based on the Lifestyle Profile. Each program will have the appropriate frequency response, features, and its own set of dedicated controls to make fine-tuning easier. |

|
| More on custom fitting “Toward Normal Hearing in Noise: How to Steer Your Patients Through the ALD Maze.” By Brian Taylor, AuD. August 2006 HR. “Volume Control Preferences with WDRC Digital Aids.” By Rhys Meredith, MSc. July 2006 HR. “Evidence of Enhanced Fine-Tuning with a New Datalogging System.” By Neil S. Hockley, MS, Reinhard Winter, and Lorrie Scheller, AuD. October 2006 HR. “Understanding People’s Social Styles Can Boost Productivity.” By Brian Taylor, MA, and Rebecca Younk, MS. January 2005 HR. “The Platinum Rule: Protocol and Process.” By Von Hansen. April 2001 HR. |
Even though Mr Smith and Mr Jones both have identical hearing losses and are fitted with identical ICOS instruments, their outcomes are significantly different with regard to program allocation, use of adaptive features, frequency response, and the software controls available to the hearing care professional. Each assigned program is tailored specifically to optimize the listening goal of the patient (Figure 2).
Conclusion
The goal of all hearing aid fittings is to achieve patient satisfaction. Hearing care professionals should recognize that one of the key factors in achieving this goal is to integrate the patient’s individual needs and preferences into the hearing instrument fitting via the fitting software. This eliminates guesswork and can lead toward a truly personalized outcome.
References
- Kochkin S. MarkeTrak VII: Customer satisfaction with hearing instruments in the digital age. Hear Jour. 2005;58(9).
- Kochkin S. On the issue of value: Hearing aid benefit, price, satisfaction, and brand repurchase rates. Hearing Review. 2003;10(2):12-25.
- Dillon H. Hearing Aids. Sydney, Australia: Boomerang Press; 2001.
- Cox RM. Outcome measures and their relevance to the retail dispenser. Paper presented at: Biennial Meeting of British Society of Hearing Aid Audiologists; November 2002; Birmingham, UK.
- World Health Organization. Toward a common language for functioning, disability and health. Geneva, Switzerland: WHO;2002.
- Sutherland G, Millett P, Parnes P, et al. Preferred Practice Guideline for the Prescription of Hearing Aids to Adults. College of Audiologists and Speech-Language Pathologists of Ontario. Approved 2000. Available at: www.caslpo.com/english_site/m_memppg.asp. Accessed: April 2, 2007.
- Valente M, Abrams H, Benson D, et al. Guidelines for the audiologic management of adult hearing impairment. Audiol Today. 2006; 18:5:32-36.
- National Acoustic Laboratories (NAL). Instructions for COSI™ Administration. Available at: www.nal.gov.au/nal_products%20front%20page.htm. Accessed April 10, 2007.
- Dillon H, James A, Ginis J. Client Oriented Scale of Improvement (COSI) and its relationship to several other measures of benefit and satisfaction provided by hearing aids. J Am Acad Audiol. 1997; 8(1):27-43.
- Taylor B. How quality of service affects patient satisfaction with hearing aids. Hearing Review. 2006; 59(9): 25-34.